3.3 The Brain and Body During the Experience of Emotions
We neither have “happy centers” nor “sadness centers” in the brain (Freberg, 2019, p. 505). Demasio and colleagues in 2000 found in their research that each emotion is characterized by “complex patterns of activity involving multiple regions of the brain” (cited in Freberg, 2019). However, they also suggested that each time the same emotion was experienced and expressed, the same regions would be activated in the same way. A bit like an emotional fingerprint for each emotion. Feldman Barrett, however, found in her research that even individual emotions (called “emotion categories”) such as anger, fear and sadness do not have a “biological fingerprint”, but that each instance of emotion can vary in terms of how they are processed by the brain (you have learned about this phenomenon as degeneracy).
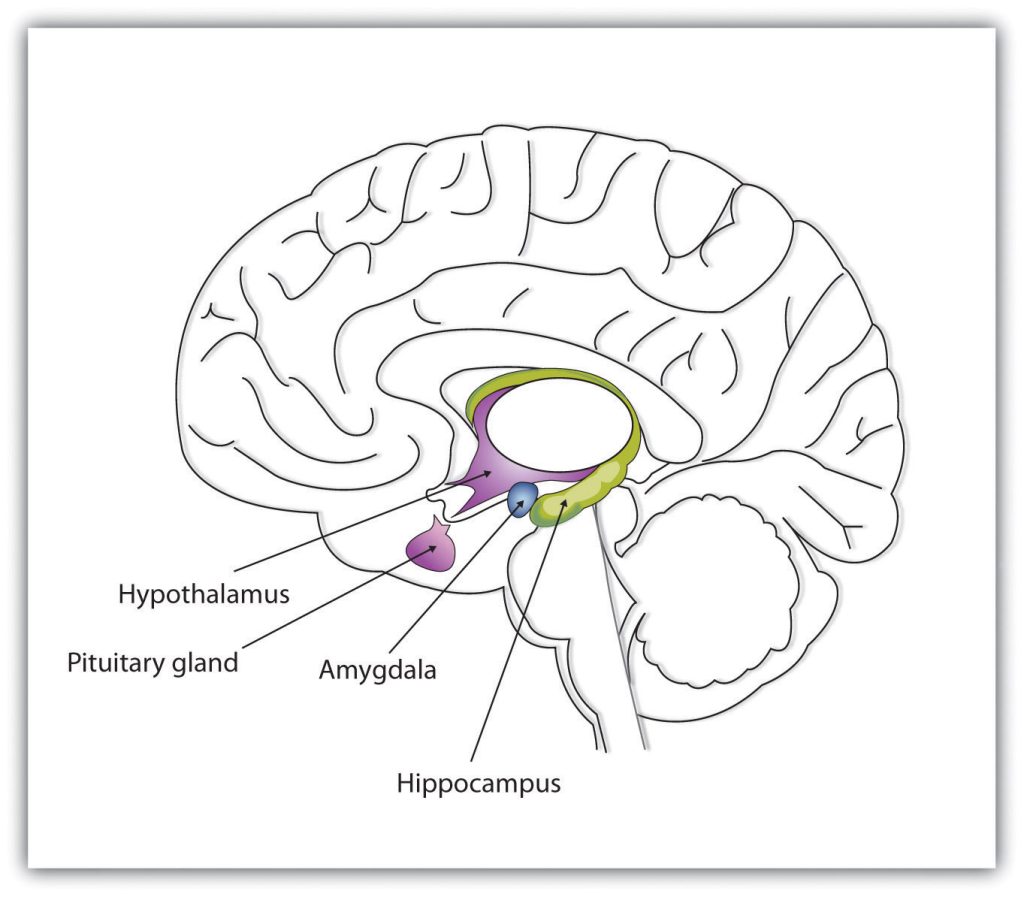
We will now briefly revisit some (but not all) of the brain structures to which you were introduced in Chapter 1, focusing on those brain structures that have been found to play a significant role in the experience of many emotions.
Note: Much of the information listed above is adapted from Freberg (2019), but also from other sources included in the references..
Now that we have brushed up on our knowledge about brain structures that play an important role in the experience of emotions, we will have a look at how these structures and systems may function during affective states and emotions, including during stress and fear. We will start with an exploration of what is commonly termed the “stress response”. As an introduction to this topic, please watch the following video [11:22] by Sam Hardy (used with her permission):
We will look at some of the topics discussed by Sam in her video in more detail now.
Stressors
Stress, as we noted earlier in this chapter, may be defined as an unpleasant and disruptive state resulting from the perception of a so-called stressor (Freberg, 2019). The term stressor refers to situations or events that elicit a physiological stress response in a person, like the perception of danger and threat. Note that the perception of threat and danger is not limited to obvious and objectively dangerous events (like exposure to extreme heat, confrontation with a weapon, or seeing a crocodile jump out of the water in front of you), but may also be of psychological, emotional, or social nature, such as reliving a specific traumatic event, losing a loved one, or being ridiculed by your boss in front of your co-workers.
According to Tanz & McClintock (2017) “the two most potent psychological stressors are being negatively evaluated by others and not having a sense of control” (p. 37). The latter is of great importance in the context of conflict resolution processes like mediation and coaching, since the feeling of being in control can be supported through these processes.
Certain stressors are likely to evoke a much stronger reaction in some individuals than in others, depending on factors like gender, cultural background, personality, etc. For example, research suggests that men are more likely to respond to insults than women (O’Dea et al., 2017). Research also indicates that a strong belief in masculine honour may make it more likely for men to engage in fighting behaviour in response to insults that challenge masculine honour (e.g. being called a “pussy”) (O’Dea et al., 2017).
Please now watch the following video [9:48] by Sam Hardy (used with her permission) in which she discusses stressors (also referred to as triggers or hooks) in more detail:
In the previous chapter, we learned that perception depends on subjective experiences. The perception of a stimulus as a stressor and the resulting experience of stress is also highly subjective and variable from person to person (Freberg, 2019). This also means that the perception of a stressor may be altered, such as that a person may be able to change the meaning of a stimulus from being a stressor to being a neutral or even positive stimulus (as also discussed by Lisa Feldman Barrett in her Ted Talk in Chapter 3.2). We will talk more about strategies to master our reactions to stressors further below as part of the topic on “emotion regulation”.
Components of the Stress Response
The perception and identification of a certain stressor typically initiates a “predictable series of reactions” (Freberg, 2019, p. 514), including physical, cognitive, and behavioural responses. The physiological response involves the nervous system, hormones, and immune system, which induce increased heart rate, blood pressure and respiration. These changes support our cognitive system to become highly aroused and vigilant and prepare us for behaviours to cope with the stressor, including what is typically called “fight or flight” behaviour. We will have a look at the physical and cognitive changes first before we focus on various fight-or-flight behaviours in more detail.
When the sensory system detects a stressor, information is sent simultaneously to 1) the amygdala for rapid assessment of the stimulus as a potential threat (referred to as the direct pathway or “fast road”) and 2) to higher cortical processing centres for a conscious appraisal of the situation (referred to as the indirect pathway or “high road”).
As shown in Figure 3.3.1, the amygdala can identify a stimulus as threatening before we have consciously appraised it. Patients who are blind because of damage to the occipital lobe – remember that this is the lobe that is responsible for visual processing – have been found to still show reactions in their amygdala when shown a potentially threatening stimulus even without being able to consciously, visually identify the stressor (Freberg, 2019). After the perception of a stressor, regardless of the road taken, two systems are typically activated to cope with the stressor.
The 1st system – this system is called the sympathetic adrenal-medulla, in short SAM, system – is very quick and involves the release of epinephrine (adrenaline) and norepinephrine (in under a minute) from the adrenal glands into the bloodstream. From there, the epinephrine and norepinephrine travel to the brain and other organs to produce immediate and short-term fight-or-flight responses (note that epinephrine released from the adrenal glands cannot cross the blood-brain barrier and thus produces effects on the brain indirectly) (Freberg, 2019). These responses include an increase of heart rate and breathing, constriction of blood vessels, alertness, and energy availability (adrenaline stimulates the release of stored glucose into the bloodstream) (Freberg, 2019). The norepinephrine released as part of this system also enhances memory formation (by being released into the amygdala and hippocampus) (Freberg, 2019). This first system starts going back to normal after about two to three minutes after detection of a stressor and recovery is typically completed within 20 minutes.
The 2nd system – this system is called the hypothalamic-pituitary-adrenal (HPA) axis – is slightly slower to be activated, but its effects last for longer. This system involves the release of cortisol. Cortisol is associated with increased blood pressure, heightened levels of alertness, as well as additional energy to enable dealing with a stressor. Cortisol rises during a stressor but may also already rise in anticipation of a stressor (e.g., before having to give an opening statement during a mediation). For a mild stressor, cortisol has been found to peak after about 20 minutes after a stressor is detected and remains in the blood for at least 2-3 hours after a stressor is gone (Freberg, 2019; Lempert & Phelps, 2016). This process may take much longer for emotionally traumatic events. The experience of ongoing stress without breaks for recovery bears the risk of chronically high levels of cortisol.
| Increases in… | Decreases in… |
| Blood pressure and heart rate | Digestion |
| Respiration | Immune system function |
| Blood glucose level | Sexual arousal |
| Pain suppression | Touch sensitivity |
| Perception and awareness | Peripheral vision |
| Blood flow to large muscles in legs and arms | Growth |
While short-term stress can have beneficial effects (if experienced short-term and in manageable doses), including boosting our immune system or increasing our attention and alertness (e.g. during an exam or job interview), chronic stress, for example, as experienced during ongoing conflict, can weaken our immune system and thus have negative and long-lasting health consequences (Feldman Barrett, 2017a; Freberg, 2019; Kemeny & Shestyuk, 2008).
Cortisol impacts those brain areas that are responsible for our experience and perception of emotions like fear and anger. For example, cortisol appears to enhance the functioning of the amygdala, the hippocampus (involved in memory) and our frontal and pre-frontal cortex (involved in cognitive processes like reasoning and decision-making) (Lempert & Phelps, 2016). We will look at this impact in more detail in the next section. Cortisol has also been found to affect the mesolimbic dopamine system, thereby altering our processing of incentives and rewards (Lempert & Phelps, 2016; Tanz & Mcclintock, 2017). Since all these emotions and cognitive functions (fear, anger, memory, decision-making, etc.) are highly relevant for conflict management, and since the effects of cortisol can last for several hours, understanding the impact of cortisol is of particular interest for conflict practitioners when dealing with people in conflict.
Behavioural Component of Stress Response
Possible behaviours that people may display during the stress response include fight, flight, freeze, or tend and befriend, also referred to as fawn. Let’s look at these behaviours in some more detail now. Most of the information below has been gathered from the web page Fight, flight and freeze responses of Trauma Recovery.
The Stress Response and Behavioural Components in Action
Please watch the following videos [1:24 & 5:45] about Will Smith slapping Chris Rock during the Oscars 2022 and think about what the main stressor may have been for Will Smith, what sort of emotions may have been going on for both men in the situation (before and after the slap), which behaviours they were both displaying during the situation and afterwards and which factors may have impacted on their behaviours.
The Physiological Side of Emotions More Generally
Before we conclude this session, we would like to highlight that physiological changes associated with emotions are not limited to the stress response. In fact, the stress response is associated predominantly with perceptions of danger and threat and the experience of fear. However, as we know the range of possible emotions is much wider than that.
Reflection Activity
One goal of this eBook is to develop your skills as a conflict practitioner and support you in understanding your own thoughts, feelings and behaviours associated with conflict better. Please spend about 10 minutes now considering which stimuli, including events, situations, objects, people, you have perceived/perceived as stressors eliciting your stress response. You might want to think about some specific conflict scenarios from your past.

