33 Crisis governance and COVID-19
Nicholas Bromfield
Key terms/names
Australian Health Protection Principal Committee, COVID-19, Communicable Diseases Network Australia, Council of Australian Governments, crisis, crisis preparation, crisis prevention, crisis recovery and learning, crisis response, Department of Health, federalism, governance, JobKeeper, JobSeeker, lockdown, public health, vaccination
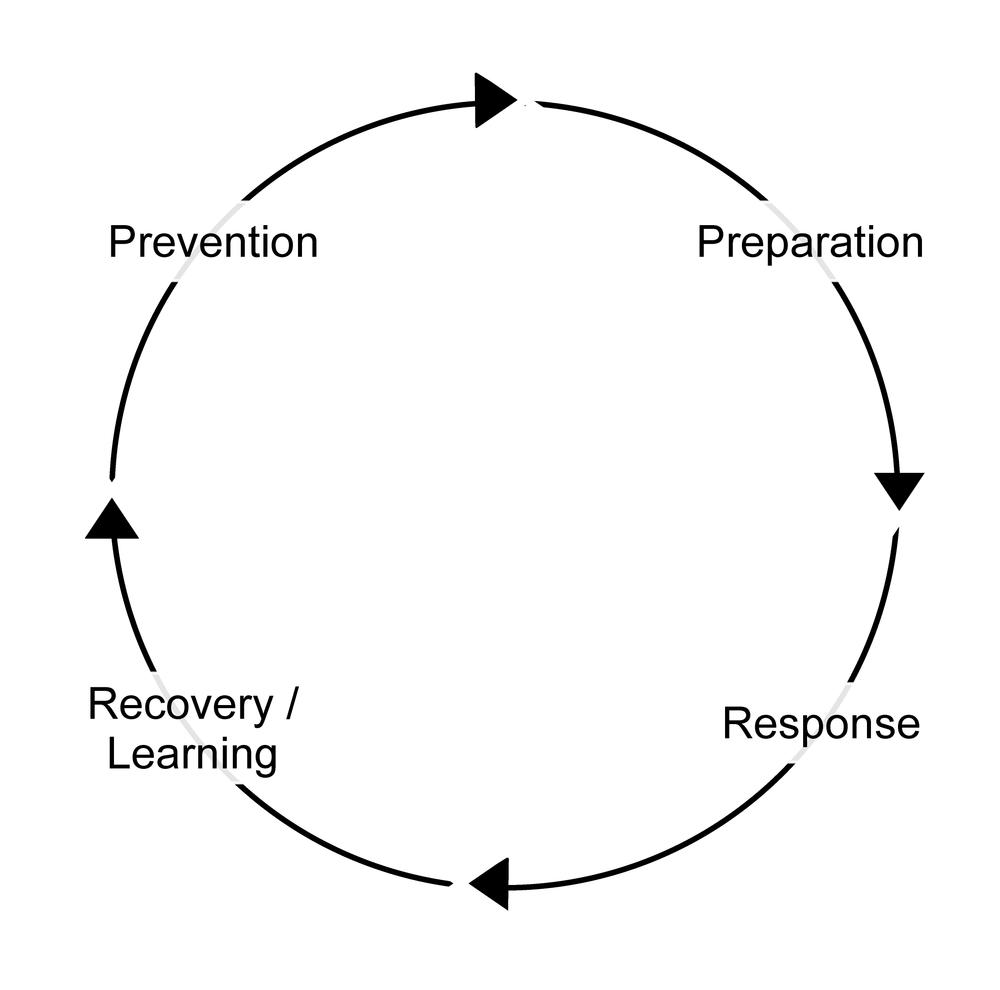
COVID-19, a coronavirus emerging in late 2019,[1] quickly snowballed into a global public health crisis on a scale not seen in generations. Crisis, ‘a set of circumstances in which individuals, institutions or societies face threats beyond the norms of routine day-to-day functioning’,[2] is a situation that governments must face as both an objective fact and subjective perception. These dual dynamics of fact and perception have shaped the responses of Australian governments to COVID-19 at both the federal and state level. While there are many ways we can examine the policy process (see Weible and Sabatier’s Theories of the policy process for an excellent introduction),[3] a relevant introductory method to examine the governance of COVID-19 in Australia is the crisis management cycle, illustrated in Figure 1.[4] This applies the cycle of prevention, preparation, response, and recovery and learning, and points to the role of actors, institutions and policy design, and tools in crisis management across these stages. The chapter demonstrates that crisis evaluation is a tricky and political activity characterised by contested perceptions and complicating evidence.[5]
The crisis management context
It is important to understand the context of Australia’s COVID-19 governance response. Of particular significance are institutions, actors and dominant modes of governance that inform policy design. This section briefly introduces these factors that need to be considered when assessing Australia’s response to COVID-19.
The first point to consider is Australia’s institutional framework. Australia is a settler society, established by the British and imposed violently upon Indigenous peoples. Australia adopted the Westminster tradition of responsible government ‘with a fused executive and legislature, ministerial responsibility, and a separate public service’[6] but also adopted elements of the American system with federalism, the constitutionally enshrined division of power between a central government and subnational governments.[7] The politics, contestation and bargaining that these institutional structures produce across layers of government must be incorporated into our assessment. This is particularly true of health policy, where different levels of government (federal, state and local) play a role in the development, funding, and delivery of health services.
These institutions are populated by actors in positions of decision-making power. While the institutional framework provides a decision-making matrix that actors must operate within, their approaches and strategies matter too.[8] Federalism, and the sharing of governance responsibilities across layers of government, multiplies the number of actors who need to be incorporated into the decision-making process – cabinets of ministers at federal and state levels, and the attendant ministerial portfolio public servants – and complicates the coordination of a crisis response.
Finally, governance itself needs to be assessed. Governance is the trend in recent decades away from top-down, state-led decision making and policy implementation. Instead, governments have tended to retain the ultimate say over making and implementing policy decisions, while also accommodating less hierarchical decision making and policy delivery. This has involved a greater plurality of actors within governments, markets and the third sector.[9] Modes of governance refer to the different emphases of governance and policy delivery, with state-led governance, market-oriented governance, and networked and third-sector governance.[10] These government, market and network/third-sector modes of governance have all been mobilised by Australian governments during the pandemic and offer the final contextual factor under consideration.
In sum, institutions of responsible government and federalism provide a framework that multiple actors must operate within. These actors, at various levels of government, still retain choices regarding making policy decisions and adopt modes of governance according to situational appropriateness and ideological preference.
Crisis prevention
Crisis prevention can be achieved if potential risks are first identified, evaluated and managed, but this may not always be possible or necessary. One approach is to think about risk in probabilistic terms: ‘a mode of thinking in which the costs and benefits of specific actions and discrete events are weighed in the balance.’[11] Policy makers who employ probabilistic risk assessment may well identify risks related to an action, assess them and identify that the risks they pose are tolerable. An example might be weighing the benefits of a hazard-reduction burn in a remote location versus the low probability posed by a bushfire in this remote location affecting infrastructure or posing a danger to human life. In these circumstances, a probabilistic risk assessment would likely conclude that the risk posed by a fire is present, but tolerable, and choose not to do a hazard-reduction burn.
In other circumstances, we may have the means to avoid the risks associated with crises and also the means to achieve this. These kinds of risks are usually associated with a form of human behaviour that can be controlled or mitigated. An example might be the introduction of financial laws that regulated the risky loans practices by lenders to borrowers who could not afford the repayments – the situation ultimately contributing to the Global Financial Crisis (GFC) in 2007–08. But ‘pure’ risks, like natural disasters or pandemics, are usually inherent and unavoidable and consequently need to be controlled or contained, rather than tolerated or avoided.[12]
The Australian federal government assessed pandemics to fall into this ‘unavoidable’ category, recognising prior to the COVID-19 pandemic that ‘it is inevitable that the world will face another influenza pandemic. While there is no certainty about where or when the next one will occur, Australia must be prepared.’[13] As such, the prevention measure in place prior to the outbreak of COVID-19 was a surveillance program to monitor for communicable disease and pandemic influenza outbreaks. Reflecting Australia’s federal system, the Commonwealth was responsible for monitoring communicable diseases domestically and internationally, and liaising diplomatically with neighbour nation-states regarding monitoring. The states and territories were responsible for collecting influenza data from their health systems to contribute to the national picture of pandemic preparedness. The Australian Health Protection Principal Committee (AHPPC) peak body and its Communicable Diseases Network Australia (CDNA) subcommittee were responsible for coordinating this surveillance across Australia’s system of federalism.[14] Notably, more authoritative COVID-19 management policy tools, like ‘enhanced border measures’, were conceptualised as pandemic response measures, rather than as pandemic prevention measures in the Australian Health Management Plan for Pandemic Influenza (2019).
The surveillance and prevention stage was short lived during the COVID-19 crisis. The World Health Organization (WHO) received notification of ‘pneumonia of an unknown cause’ from the Chinese government in late 2019 and notified all member states, including Australia, in early January 2020.[15] Australian authorities acknowledged the potential risk posed by COVID-19 and quickly shifted to the response stage. On 19 January, the Australian Chief Medical Officer publicly acknowledged COVID-19, the National Incident Room in the Health Department was activated on 20 January and ‘human coronavirus with pandemic potential’ was added to the Biosecurity (Listed Human Diseases) Determination (2016) on 21 January.[16] These acts triggered several pandemic mitigation measures that had been planned. This contingency planning is considered below.
Crisis preparation
Crisis planning is both an objective process and one of perception and evaluation. As above, assessing and planning for risk involves an assessment of the nature and likely impact of the crisis, both of which are uncertain and based upon probabilistic reasoning. Evidence may be incomplete or based upon models underpinned by partial consideration of potential variables, and is weighed against more political considerations of competing priorities and limited resources.[17] Governments should therefore expect to be agile and adaptive in the face of crisis.[18]
Nonetheless, an imperfect crisis plan is better than no crisis plan.[19] Crisis planning should also integrate all key institutions in a ‘whole of government’ approach that joins up the key actors and organisations in government and connects them to relevant market and third-sector organisations and actors outside government. Kamradt-Scott argues that an influenza pandemic’s ability to disrupt national and global societies and economies means that a response cannot be limited to dedicated emergency agencies.[20] This notion is reflected in both Australia’s pandemic and disaster standing plans and arrangements, which dedicated considerable effort into whole-of-government and joined-up planning across Australia’s system of federalism.
Significant contingency planning for disasters, crises and pandemics had been completed by the Commonwealth government prior to the outbreak of COVID-19. Coordination of influenza pandemic planning across Australia’s federal layers of Commonwealth, state and territory governments has been in place since 1999. The last major update was in 2014, incorporating lessons from the H1H1 ‘swine flu’ pandemic of 2009, and a minor update in August 2019: Australian Health Management Plan for Pandemic Influenza (AHMPPI). Whole-of-government language was emphasised throughout the plan and the logic was explained as: ‘Maintaining essential services may require a whole-of-government response, incorporating agencies at the Australian Government and state and territory government level’.[21]
The key documents in Australia’s standing pandemic plans and related health and crisis management documents are summarised in Table 1.
| Standing plan | Purpose |
|---|---|
| The Australian Government Crisis Management Framework (2017) (AGCMF) | The AGCMF is the overarching framework plan for response to and recovery from any crisis or disaster in Australia. The plan also sets out the whole-of-government response to public health crises. |
| The COMDISPLAN 2017: Australian Government Disaster Response Plan (2017) (COMDISPLAN). | The COMDISPLAN sets out the arrangements and coordination required for federal provision of non-financial assistance (e.g. planning expertise, advice, Commonwealth resources and physical assistance) to Australian states and territories in the event of a crisis, emergency or disaster. |
| Emergency Response Plan for Communicable Disease Incidents of National Significance (2016) (the CD Plan) | The CD Plan is the overarching Australian health plan for communicable diseases, standing above the AHPPMI. The plan sets out the role of federal and state health authorities in the event of a communicable health emergency, preparedness and responses measures, and describes how a communicable disease incident of national significance (CDINS) is declared, escalated and stood down. |
| The Emergency Response Plan for Communicable Disease Incidents of National Significance: National Arrangements: National CD Plan (2018) (the National CD Plan) | The National CD Plan’s purpose is to supplement the CD Plan in any CDINS circumstance where national coordination may be useful. The plan emphasises whole-of-government coordination and sets out the role of Australian federal, state and territory governments, but also emphasises the role of local government. |
| The Australian Health Management Plan for Pandemic Influenza (2019) (AHPPMI) | The AHPPMI is the Australian Commonwealth’s whole-of-government response plan to an influenza pandemic. The plan emphasises flexibility, proportionality and scalability. Four areas of priority are identified: prevention, preparedness, response and recovery. |
But plans are only part of the preparedness mix. Also important is the testing and simulation of crisis responses. Australia was something of a world leader in pandemic planning and preparation during the 2000s, initiating the governance frameworks outlined above and running full-scale simulations of pandemic scenarios. But a combination of changing priorities and austerity after the GFC, combined with the relative mildness of H1N1 in 2009, saw a de-prioritisation of this scenario training, a situation some have identified as contributing to confusion over responsibilities between layers of government during the early months of the COVID-19 crisis in Australia.[22] Nonetheless, the 2019 Global Health Security Index, which benchmarked the health security and related capabilities of states, ranked Australia fourth out of 195 countries in terms of preparedness for pandemics and their consequences prior to the crisis.[23] So, while pandemic preparedness had evidently needed to compete with other government priorities in Australia prior to COVID-19’s emergence, comprehensive planning and (dated) testing of that plan was in place.
Crisis response
Crises vary in their length and impact, which in turn affects the nature of the acute phase of the crisis response. For instance, the acute phase of crisis events like an earthquake or a terror attack may be over quickly and limited to small locales. In these instances, the crisis response stage may be largely limited to securing the area and managing casualties before shifting promptly to recovery. In other ‘pure’ crises, like fires, floods and pandemics, the crisis and its effect may continue for weeks, months or, in the case of COVID-19, years. In these circumstances, when control over events is limited and precarious, crisis management becomes a process of ‘coping through’ as unharmed as possible.[24] The crisis context, adaption and improvisation of plans and responses, response leadership, knowing when to act, and by how much, all influence the outcome of crisis management. Australia’s response to the acute phase of the COVID-19 crisis is evaluated against these factors below.
The acute stage of the COVID-19 crisis in Australia, and the response to it, is here defined as the ‘pure’ stage of the crisis, the 12-month period from the emergence of COVID-19 in January 2020 to February 2021, when the Sydney Northern Beaches cluster began to dissipate and COVID-19 vaccines could reasonably have been expected to have become available to mitigate the crisis and move the response into the recovery and learning stage. The context of the crisis was Australia encountering COVID-19 at the tail-end of the Black Summer bushfire crisis, an event that saw one of the most widespread and destructive fires in Australian recorded history and widespread criticism of the federal Coalition government’s handling of this disaster.[25]
Despite this context, Australia quickly responded to the COVID-19 crisis and activated several pandemic arrangements, adopting (after contestation between states and the Commonwealth) an ‘aggressive suppression’ strategy of COVID-19 management. The January 2020 activation of the National Incident Room in the Health Department and adding of COVID-19 to the Biosecurity (Listed Human Diseases) Determination triggered a number of pandemic arrangements:
including daily meetings of the Australian Health Protection Principal Committee (AHPPC) and meetings of federal, state and territory health ministers. On 25 February, the Australian government activated the National Communicable Disease Plan, and two days later, the COVID-19 Plan was agreed upon and activated by the National Security Committee of Cabinet.[26]
Australian governments also quickly adapted their crisis and pandemic planning to the COVID-19 crisis. This initial adaptation is summarised in the response documents in Table 2.
| COVID-19 response plan | Purpose |
|---|---|
| The Australian Health Sector Emergency Response Plan for Novel Coronavirus (COVID-19) (7 February 2020) (COVID-19 Plan) | The COVID-19 Plan is a living document that adapts the Australian Pandemic Plan (AHPPMI). It focuses on the response elements of AHPPMI, with initial action (while information is scare) and targeted action (when enough information is known to allow tailored measures to specific needs), and stand down. The COVID-19 Plan also draws upon the Australian Government Crisis Management Framework and the National CD Plan for whole-of-government structures and coordination of the response. |
| The National Partnership on COVID-19 Response (13 March 2020) | The National Partnership on COVID-19 Response established the National Cabinet arrangements (later made permanent on 29 May 2020). It is an intergovernmental agreement between the Australian Commonwealth and the states and territories. The agreement provides for arrangements whereby the Commonwealth will provide financial assistance to the states and territories for the additional costs incurred by state health services in responding to the COVID-19 outbreak. |
| The Management and Operational Plan for Aboriginal and Torres Strait Islander Populations (MPATSI) (30 March 2020) | The MPATSI is a living document that is an adaption of the COVID-19 Plan developed by the Aboriginal and Torres Strait Islander Advisory Group on COVID-19. The MPATSI acknowledges the higher risk from morbidity and mortality that Aboriginal and Torres Straight Islander peoples face generally and during a pandemic, and that a culturally appropriate response is necessary. It provides an overview of the approach to COVID-19 as it relates to Aboriginal and Torres Strait Islander peoples and communities, and an operational plan. |
This adaptation reflects the negotiation of Australia’s federal institutional features and whole-of-government mode of crisis governance to suit the leadership styles and political preferences of Australia’s federal, state and territory leaders. While Prime Minister Morrison demonstrated a masculine and semi-presidential leadership style, he also had to negotiate with state counterparts who brought their own leadership styles and party allegiances (five state and territory governments were Labor-controlled and three Liberal- or Liberal–National-controlled).[27]
The National Cabinet was one forum for the cooperative and combative relations of federal, state and territory relations to play out. The National Cabinet was perceived to streamline intergovernmental relations, replacing the Council of Australian Governments (COAG). National Cabinet was seen as a less bureaucratic and more personalised forum, free from the more formal agenda and process constraints of COAG. While not a true cabinet,[28] it was argued that this adaption of institutional arrangements was necessary given the complexities of sustained and ongoing crisis coordination across diverse Commonwealth, state and territory jurisdictions and leaderships. National Cabinet largely worked well during the acute phase of the crisis ‘effectively managing the “flattening of the curve” and engendering public trust in the intergovernmental response’ via mostly cooperative federal relations.[29] A notable exception was the prominent tension with Victoria during the state’s second-wave outbreak from June to October 2020, which saw 112 days of lockdown and a four-month closure of the border with New South Wales. This outbreak saw some of the most stringent lockdown regulations and enforcement in the country up until that point. Perhaps most controversially, the measures also included a ‘hard lockdown’ of 3,000 residents in nine public housing towers that was imposed without notice and prevented residents from leaving. The Victorian Ombudsman later found the public housing lockdown’s timing was not based on health advice and violated Victorian human rights laws.[30]
Arrangements were also developed to incorporate market and third-sector actors into the governance of the acute phase of the crisis response. For example, the National COVID-19 Coordination Commission (NCCC) – subsequently renamed the National COVID-19 Commission (Advisory Board) (NCC) – was created to incorporate business and government leaders into an advisory forum. The NCC initially mobilised the networks and experience of the committee members to troubleshoot personal protective equipment, supply chain, and freight and transport issues, as well as connect laid-off workers to emerging labour shortage needs. As restrictions began to ease, the NCC switched focus to providing support and information for businesses as they reopened and to providing an advisory role to government regarding the long-term economic recovery from COVID-19. Here it attracted controversy by advocating for a ‘gas-led recovery’ from the economic downturn caused by COVID-19 and the potential conflicts of interest this posed for NCC members.
Another example was the Aboriginal and Torres Strait Islander Advisory Group on COVID-19, who developed and delivered the MPATSI (see Table 2). The Aboriginal and Torres Strait Islander Advisory Group on COVID-19 incorporated Indigenous public sector and third-sector stakeholders and public health experts. The group recommended policies co-designed with Indigenous peoples, including legislative changes to minimise travel to remote and vulnerable communities, culturally specific health promotion materials, infectious disease modelling, epidemiological tracking, rapid testing, and infrastructure and workforce preparations.[31] As evidence of the success of these efforts during the acute phase of the crisis response, as of 28 February 2021, there had only been 150 cases of COVID-19 amongst Aboriginal and Torres Strait Islander peoples, representing 0.5% of total cases.[32] However, critics have argued that these policies also failed to acknowledge the diversity of Indigenous needs, and perpetuated paternalistic and racialised discourses of Indigenous vulnerability and deficit. This fed into the use of law-and-order enforcement responses to control movement, and an emphasis on individualised health focus over social models of health promoted by Aboriginal Community Controlled Health Organisations (ACCHOs).[33]
Other prominent COVID-19 policies included the plethora of authoritative policy tools adopted by the Commonwealth and states and territories to deal with case numbers. The Commonwealth introduced border controls that limited or banned travel to and from the country and two-week quarantine periods for returned travellers. State and territories introduced various levels of stay-at-home orders, which limited visitation and movement of people within states and, more controversially, closed borders between states. This massive use of state power was also augmented with test, trace and isolate policies that sought to identify positive cases through mass public testing, track their movements in the community and order them to stay at home while infectious. Critics have argued that the adoption of these authoritative measures reflected Australia’s lack of state capacity to deal with disaster after decades of contracting out to the market and third sector.[34]
Finally, this acute period of the crisis also saw the Commonwealth, states and territories introduce various payments to businesses and individuals affected by lockdown orders. This prominently included the Commonwealth JobKeeper and JobSeeker payments that aimed to ameliorate the economic impacts of the crisis. JobKeeper provided funds to businesses to keep employees on, rather than to lay them off, and JobSeeker doubled unemployment benefits for those that found themselves out of work.[35]
These measures proved to be quite effective when assessed against the aims of the ‘aggressive suppression’ strategy, with only 64 COVID-19 cases in the country in the fortnight leading up to 28 February 2021 and no deaths, and with the cumulative case count being 28,937 with 909 deaths. We can compare this with some of the hardest-hit countries during February 2021 (Table 3).
| Nation | Total cases | Cases per million people | Nation | Total deaths |
|---|---|---|---|---|
| United States | 2,498,366 | 7,527 | United States | 73,587 |
| Brazil | 1,337,117 | 6,290 | Brazil | 31,169 |
| France | 544,857 | 8,078 | Mexico | 27,895 |
| Russian Federation | 395,640 | 2,743 | United Kingdom | 17,134 |
| United Kingdom | 374,431 | 5,569 | Germany | 13,100 |
Unsurprisingly, given this comparative picture, there is evidence that Australian public opinion largely agreed with COVID-19 measures and was satisfied with their level of effectiveness, with trust in government and the government response increasing during this acute phase of the crisis.[37] In sum, the governments of Australia had managed to ‘cope through’ the acute phase of the COVID-19 crisis quite effectively, keeping case numbers and deaths comparatively low and sustaining a high level of trust in their COVID-19 management policies.
But what does Australia’s COVID-19 management success during this acute phase look like when assessed against other policy outcomes? The top-line focus on Australia’s success in managing case numbers and deaths masks the controversies and contestation evident during this acute phase of the crisis, especially surrounding the use of state power and authority. For instance, international border restrictions limited both the ability of Australian citizens and residents to arrive in the country, and unusually, banned leaving the country without approval. This had the effect of stranding citizens and residents overseas and prevented others from leaving Australia to see overseas family and loved ones – a massive curtailment of the right to freedom of movement. Similar border closures were evident internally too:
some main points of inter-jurisdictional or bureaucratic tensions were between states over border controls (particularly New South Wales and Queensland, and later with Western Australia) and in the blame games over who authorised (notably, NSW Health or the Australian Border Force) 2,671 passengers, including 110–120 sick passengers and crew, to disembark from the cruise ship Ruby Princess.[38]
The states and Commonwealth also disagreed amongst themselves regarding responsibility for quarantine arrangements and the form those arrangements should take, notably regarding the use of hotels to quarantine returning travellers. National Cabinet operated as a forum for contestation over these competing preferences and perceptions, which points to the differing aims, priorities, and accountabilities that existed between the states, and between the states and the Commonwealth, that can complicate a crisis evaluation.
As the acute phase came to an end, the focus shifted to vaccine procurement and distribution – the means to shift to the crisis recovery and learning phase of crisis management. The relative slowness of the vaccine rollout precipitated the challenges Australia faced as the Delta COVID-19 variant emerged in mid-2021. These developments demonstrate the precariousness of crisis management success and the caution we should exercise when attributing success to crisis governance.[39]
Crisis recovery and learning
The crisis recovery and learning phase of the crisis management cycle can be especially ambiguous. It can be hard to determine when a crisis has ended, as crisis dissipation is frequently non-linear. Crises may resurge and therefore complicate, interrupt or set back recovery and rebuilding. Nonetheless, once the acute phase of ‘coping through’ has ended, we would normally expect to see forms of debriefing, counselling, rebuilding, inquiry, evaluation, accountability and learning.[40]
At the time of writing (September 2022), the COVID-19 crisis demonstrates ambiguity by clearly not being over, but also clearly no longer being acute either. This complicates any evaluation of the recovery and learning stage of the COVID-19 crisis – put simply, we are still in it. What is offered here is an outline of some of the most prominent policy challenges and developments during the final stages of the COVID-19 crisis in Australia. The recovery stage of the COVID-19 crisis is here defined as the period from February 2021, when the means for COVID-19 recovery – vaccines – first began to be administered.
To begin, the difficulties, controversies and policy failures of the shift to recovery can be seen in the initial vaccine rollout design, heavily reliant as it was on the local manufacturing of AstraZeneca as the cornerstone vaccine. The Commonwealth government’s vaccine acquisition and rollout design was challenged by the perceived efficacy and safety of AstraZeneca, combined with delays in the delivery of vaccines to priority communities, and then the populace at large. There were issues with crisis communication, with the federal government promising AstraZeneca numbers it could not access due to the difficulties with supplying AstraZeneca from Europe, and before local manufacture had begun, in early 2021. The Commonwealth amplified the risks of AstraZeneca, based on advice from the Australian Technical Advisory Group on Immunisation (ATAGI), over the need to get vaccinated. State leaders and chief health officers also talked down AstraZeneca publicly and influenced National Cabinet decision making about the age rules surrounding AstraZeneca access, which had the effect of restricting vaccine access for younger people. All this helped sow AstraZeneca hesitancy and ultimately contributed to a large portion of the population waiting for Pfizer vaccines that were not initially available in the first half of 2021 and making them vulnerable during the Delta wave in the middle of 2021.
Administrative policy to deliver the vaccines was more successful, as demonstrated by the rapid vaccination of the population by state governments in the second half of 2021. But significant shortfalls also existed, with this uptake being slow to start and gaps in vaccine coverage amongst vulnerable and prioritised populations, like the elderly, the disabled and Aboriginal and Torres Strait Islander peoples. These delays and gaps had an outsized effect on the vulnerable during the Delta outbreak of 2021. Relations between the Commonwealth, states and territories also became notably more fractious, and blame games emerged, as Delta spread in New South Wales, and to other states and territories, prominently Victoria and the ACT in mid-2021. Despite these administrative challenges, 91 per cent of the Australian population over 16 had received two doses of COVID-19 vaccine by the end of 2021, and more than 95 per cent of over-16s had received at least two doses by September 2022.[41]
The effect of the arrival of the highly infectious Omicron variant in Australia and the surge of COVID-19 cases across the Australian summer 2021–22, and into 2022, was mediated by this high rate of vaccination amongst the community. With high vaccination rates achieved, and civil unrest and protests against vaccination and authoritative COVID-19 mitigation measures emerging after almost two years of restrictions, governments at both the state and federal level eased restrictions. The international border was progressively opened in stages to vaccinated travellers between 1 November 2021 and 21 February 2022. Borders between states also reopened, with Western Australia’s hard border being the last to be removed on 3 March 2022. While mandates to wear face masks in some high-risk settings remained, they were repealed in most settings. The COVID-19 Disaster Payment, which had been introduced 3 June 2021 for those who had lost work or income as a result of a COVID-19 lockdown, was phased out by the end of 2021. Compulsory reporting of positive tests and quarantine remained in place allowing the tracking of cases, but reporting and compliance, and therefore data, has been questionable.
Omicron and its variants did not cause severe illness in most people, but its virility and ability to evade vaccination ensured that COVID-19 cases and deaths amongst the elderly and the vulnerable surged as the policy response wound down, and almost complete individual freedom returned. A total of 7,386 people died during the Omicron wave from 15 December 2021 to 3 July 2022.[42] But COVID-19 and its management were relatively minor issues for both major parties during the 2022 federal election. The ALP’s election policy website did not mention COVID-19, while the Liberal election policy website only mentioned the crisis in conjunction with health more generally: ‘Better Health (and the Covid-19 Response)’.[43] The ALP did highlight the Coalition’s handling of the Black Summer bushfire crisis and COVID-19 in campaign attack materials,[44] but neither party campaigned on a longer-term policy plan to recover from the pandemic or care for those who would be affected by long COVID. Some commissions of inquiry into the pandemic have reported, like the Senate Select Committee on COVID-19 and Victorian COVID-19 Hotel Quarantine Inquiry. But we are yet to see more detailed inquiry and evaluation of COVID-19 responses and governance from Australian governments, despite a continuing high case load, disability and deaths. Recovery and learning has only been partially undertaken by governments at the time of writing.
Crisis evaluation
How might we evaluate Australia’s policy and governance response to COVID-19? We should remember that crisis evaluation is inherently political, in that the questions we ask, and lens we adopt to answer them, are informed by the competing interests and agendas of the actors involved.[45] McConnell develops a list of questions that any crisis evaluation must answer, a process that cannot avoid these inherently political judgements.
- Where do we set the boundaries of evaluation? Crises inherently draw in multiple actors, across layers of government, political parties, bureaucracies and non-governmental actors in business and the third sector. Choosing to focus on only some of these actors and institutions will sharpen the focus of an evaluation, but will inevitably insulate some actors from accountability, too.
- What success benchmarks do we use and how do we weigh outcomes? Benchmarks for crisis management, and the evaluation of success and failure against them, are difficult to establish objectively and may vary across time or place. Regarding COVID-19, the ‘aggressive suppression’ strategy in Australia has seen the focus on suppressing case numbers as a key measure of success. But others might point to the massive economic and social costs of achieving these low case numbers by lockdowns as a sign of failure. Another example is Victoria’s second wave, which may be viewed as a failure for getting out of hand or conversely as a successful suppression of an outbreak. The choice of which benchmark and outcome to use is informed by the perceptions, values and ideologies of the evaluator.
- How much weight do we give to shortfalls? Crisis management is rarely, if ever, completely successful on all possible measures. Crises lead to people being harmed or dying, test institutions and management processes to the extreme, and frequently cause mass inconvenience for the public. Weighing these shortcomings is another example of the inherently normative and political choices necessary in crisis evaluation.
- How do we address lack of evidence? Crisis evaluations rely on evidence to establish ‘hard facts’, but that evidence may be unavailable, contested or partial. Governments and policy makers may seek to control the terms of any inquiry to questions favourable to themselves and less favourable to political opponents. We would expect this lack of evidence to continue if public inquiries into COVID-19 governance are not established.
- Success for whom? Crises, and crisis responses, have uneven social impacts. For example, there has been ample evidence from the Victorian second wave and Sydney Delta outbreaks that there was an outsized spread of COVID-19 cases, and more punitive lockdowns restrictions and policing, in locations with higher prevalence of socio-economic disadvantage. Another important example is the situation, during the Omicron wave, of disabled people and the clinically vulnerable, who have been exposed to far greater relative risks to their wellbeing than the abled population due to high case numbers, even as the abled enjoy the easing of authoritative measures.
- What period of time to evaluate? The COVID-19 response in Australia neatly demonstrates the difficulty of assessing crisis management across time. Australia was remarkably successful at managing COVID-19 in 2020 and the first half of 2021. This picture has been inverted if we evaluate the period encompassing the Delta and Omicron waves.
As crisis evaluators, our answers to these questions will be inevitably informed by our own values, ideologies, and perceptions, leading to a particular and political assessment. That does not mean our evaluations have no value, but simply that we should be aware of the potentially hugely consequential outcomes of our assessments and the ways they can inform or limit policy learning. While it may be relatively easy to identify ‘first-order’ causes of crisis, like faulty parts that cause a train crash or an illegal gathering attended by COVID-19 positive cases that creates a super-spreader incident in a city, it is rarely satisfactory to a public that demands thorough answers and accountability.[46] But an examination of ‘second-order’ causes – for example, leadership decisions, organisational culture, failure to communicate or budget cuts – is prone to the contestation and politics identified above. As such, learning from crisis may only provide the basis for a wider political debate about how to manage crises, rather than clear-cut answers about who to hold to account and how to respond to similar events in future.[47]
Conclusion
This chapter has highlighted several factors that need to be considered in crisis evaluation and applied them to Australia’s COVID-19 crisis response. It has argued that crisis evaluation is a difficult and inherently political activity, characterised by objective facts and subjective perceptions. It has applied these ideas via the crisis management cycle of prevention, preparation, response, and recovery and learning, and has demonstrated the role of actors, institutions and policy design, and tools in crisis management across these stages.
Australia was successful in planning for, preparing for and managing COVID-19 during 2020 and the first half of 2021, if the metric of success was achieving ‘aggressive suppression’ and comparatively low case numbers and deaths. Australia has been less successful in managing the vaccine rollout in the recovery stage of the COVID-19 crisis, if measured against the ‘aggressive suppression’ strategy and the metric of low case numbers and deaths, plus the aim of rapid deployment of vaccines. This picture of conflicting evidence will complicate the calls to hold leaders and institutions to account and will likely blunt attempts to reform policies and processes to improve crisis responses in future. Students of crisis responses and evaluations should be aware of these dynamics when performing their own evaluations of the Australian COVID-19 response or crises more generally.
References
Aboriginal and Torres Strait Islander Advisory Group on COVID-19, COVID-19 National Incident Room Surveillance Team, and Indigenous and Remote COVID-19 Policy and Implementation Branch (2021). Aboriginal and Torres Strait Islander epidemiology report on COVID-19, 28 February 2021. Communicable Diseases Intelligence 45(21 May). https://doi.org/10.33321/cdi.2021.45.27
Australian Labor Party (2022). Labor’s plan for a better future. https://www.alp.org.au/policies
Bell, Stephen, and Andrew Hindmoor (2009). Rethinking governance: the centrality of the state in modern society. Cambridge, UK: Cambridge University Press.
Boin, Arjen, Allan McConnell and Paul ’t Hart. Governing after crisis: the politics of investigation, accountability and learning. Cambridge, UK: Cambridge University Press, 2008.
Bromfield, Nicholas and Allan McConnell (2021). Two routes to precarious success: Australia, New Zealand, COVID-19 and the politics of crisis governance. International Review of Administrative Sciences 87(3): 518–35. https://doi.org/10.1177/0020852320972465
Bromfield, Nicholas, Alexander Page and Kurt Sengul (2021). Rhetoric, culture, and climate wars: a discursive analysis of Australian political leaders’ responses to the Black Summer bushfire crisis. In Ofer Feldman, ed., When politicians talk, 149–67. Singapore: Springer. https://doi.org/10.1007/978-981-16-3579-3_9
Chodor, Tom, and Shahar Hameiri (2022). COVID-19 and the pathologies of Australia’s regulatory state. Journal of Contemporary Asia (12 August): 1–25. https://doi.org/10.1080/00472336.2022.2106883
COVID-19 National Incident Centre Surveillance Team (2022). COVID-19 Australia: epidemiology report 63: reporting period ending 3 July 2022. Communicable Diseases Intelligence 46. https://doi.org/10.33321/cdi.2022.46.49
COVID-19 National Incident Room Surveillance Team (2021). COVID-19 Australia: epidemiology report 36: reporting period ending 28 February 2021. Communicable Diseases Intelligence 45. https://doi.org/10.33321/cdi.2021.45.14
Crooks, Kristy, Dawn Casey and James S. Ward (2020). First Nations people leading the way in COVID-19 pandemic planning, response and management. Medical Journal of Australia Preprint (29 April 2020): 1.
Department of Health (2019). Australian health management plan for pandemic influenza (AHMPPI). Australian Government. https://www.health.gov.au/resources/publications/australian-health-management-plan-for-pandemic-influenza-ahmppi
Department of Health and Aged Care (2021). COVID-19 vaccine roll-out (31 December). Australian Government. https://bit.ly/3SwK1uX
—— (2022). COVID-19 vaccine roll-out (2 September). Australian Government. https://www.health.gov.au/resources/collections/covid-19-vaccination-daily-rollout-update#september-2022
Donohue, Monica, and Ailie McDowall (2021). A discourse analysis of the Aboriginal and Torres Strait Islander COVID‐19 policy response. Australian and New Zealand Journal of Public Health 45(6): 651–57. https://doi.org/10.1111/1753-6405.13148
Drennan, Lynn T., Allan McConnell and Alastair Stark (2015). Risk and crisis management in the public sector, 2nd edn. Routledge Masters in Public Management. New York: Routledge, Taylor & Francis Group.
Eriksson, Kerstin, and Allan McConnell (2011). Contingency planning for crisis management: recipe for success or political fantasy? Policy and Society 30(2): 89–99. https://doi.org/10.1016/j.polsoc.2011.03.004.
Global Health Security Index (2019). The global health security index. https://www.ghsindex.org/wp-content/uploads/2019/10/2019-Global-Health-Security-Index.pdf
Goldfinch, Shaun, Ross Taplin and Robin Gauld (2021). Trust in government increased during the Covid‐19 pandemic in Australia and New Zealand. Australian Journal of Public Administration 80(1): 3–11. https://doi.org/10.1111/1467-8500.12459
Janssen, Marijn, and Haiko van der Voort (2020). Agile and adaptive governance in crisis response: lessons from the COVID-19 pandemic. International Journal of Information Management 55: 102180. https://doi.org/10.1016/j.ijinfomgt.2020.102180
Kamradt-Scott, Adam (2014). Preparing for the next pandemic. In Garrett W. Brown, Gavin Yamey, and Sarah Wamala, eds, The Handbook of Global Health Policy, 539-554, Malden, MA, Wiley Blackwell.
Liberal Party of Australia (2022). Our plan. Liberal Party of Australia, 2022.
McConnell, Allan (2020). Evaluating success and failure in crisis management. In Oxford Research Encyclopedia of Politics, by William R. Thompson. Oxford University Press. https://doi.org/10.1093/acrefore/9780190228637.013.1633
Patrick and Secretary, Department of Prime Minister and Cabinet (Freedom of Information) [2021]. AATA 2719. https://constitutionwatch.com.au/wp-content/uploads/Patrick-v-Prime-Minister-AAT-Decision-5-August-2021.pdf
Pollitt, Christopher, and Geert Bouckaert (2017). Public management reform: a comparative analysis – into the age of austerity. 4th edition. New York: Oxford University Press.
Ramia, Gaby, and Lisa Perrone (2021). Crisis management, policy reform, and institutions: the social policy response to COVID-19 in Australia. Social Policy and Society (4 October): 1–15. https://doi.org/10.1017/S1474746421000427
Shepherd, Tory (2022). ‘I don’t hold a hose’: do Labor’s attack ads hit hard enough? The Guardian, 28 April, sec. Australia news. https://www.theguardian.com/australia-news/2022/apr/28/i-dont-hold-a-hose-do-labors-attack-ads-hit-hard-enough
Smith, Rodney, Ariadne Vromen and Ian Cook (2006). Keywords in Australian politics. Cambridge, UK: Cambridge University Press.
Tranter, Bruce Keith (2022). Your money or your life? Public support for health initiatives during the COVID‐19 pandemic. Australian Journal of Social Issues 57(3): 544–61. https://doi.org/10.1002/ajs4.220
Van Hecke, Steven, Harald Fuhr and Wouter Wolfs (2021). The politics of crisis management by regional and international organizations in fighting against a global pandemic: the member states at a crossroads. International Review of Administrative Sciences 87(3): 672–90.
Victoria Ombudsman (2020). Investigation into the detention and treatment of public housing residents arising from a COVID-19 ‘hard lockdown’ in July 2020. Report. Melbourne: Victorian Government Printer.
Weible, Christopher M., and Paul A. Sabatier (2018). Theories of the policy process, 4th edn. New York: Routledge.
Welch, Dylan, and Alexandra Blucher (2020). Australia ran its last national pandemic drill the year the iPhone launched. Did that harm our coronavirus response? ABC News, 19 April. https://www.abc.net.au/news/2020-04-20/coronavirus-australia-ran-its-last-pandemic-exercise-in-2008/12157916
Wilkinson, Iain (2010). Risk, vulnerability and everyday life. New York: Routledge.
About the author
Nicholas Bromfield is a lecturer with the Centre of Social Impact at the University of New South Wales, Australia. Nicholas is a public policy, administration and governance researcher with a background from political science. His research agenda diagnoses and provides solutions to issues of crisis, identity and their social impact via public policy from Australian and comparative perspectives.
His recent research projects have focused on Australia and New Zealand and the COVID-19 crisis, with interests in crisis administration, policy evidence, and civil society and third-sector participation. He also researches issues of Australian identity and their effect on policy and rhetoric.
- Revised by the author in 2023. Bromfield, Nicholas (2024). Crisis governance and COVID-19. In Nicholas Barry, Alan Fenna, Zareh Ghazarian, Yvonne Haigh and Diana Perche, eds. Australian politics and policy: 2024. Sydney: Sydney University Press. DOI: 10.30722/sup.9781743329542. ↵
- Drennan, McConnell and Stark 2015, 2. ↵
- Weible and Sabatier 2018. ↵
- Drennan, McConnell, and Stark 2015, 30–2. ↵
- McConnell 2020. ↵
- Bromfield and McConnell 2021, 520. ↵
- Smith, Vromen and Cook 2006, 67. ↵
- Bromfield and McConnell 2021; Chodor and Hameiri 2022. ↵
- Bell and Hindmoor 2009, 1–2. ↵
- Pollitt and Bouckaert 2017. ↵
- Wilkinson 2010, 8–9. ↵
- Drennan, McConnell, and Stark 2015, 103–8. ↵
- Department of Health 2019, 3. ↵
- Department of Health 2019. ↵
- Van Hecke, Fuhr and Wolfs 2021. ↵
- Bromfield and McConnell 2021, 524. ↵
- Drennan, McConnell and Stark 2015; Eriksson and McConnell 2011. ↵
- Janssen and van der Voort 2020. ↵
- Bromfield and McConnell 2021. ↵
- Kamradt-Scott 2014. ↵
- Department of Health 2019, 35. ↵
- Welch and Blucher 2020. ↵
- Global Health Security Index 2019. ↵
- Drennan, McConnell and Stark 2015, 163. ↵
- Bromfield, Page and Sengul 2021. ↵
- Bromfield and McConnell 2021, 524. ↵
- Bromfield and McConnell 2021. ↵
- Patrick and Secretary, Department of Prime Minister and Cabinet (Freedom of Information) 2021. ↵
- Bromfield and McConnell 2021, 524. ↵
- Victoria Ombudsman 2020. ↵
- Crooks, Casey and Ward 2020. ↵
- Aboriginal and Torres Strait Islander Advisory Group on COVID-19, COVID-19 National Incident Room Surveillance Team and Indigenous and Remote COVID-19 Policy and Implementation Branch 2021. ↵
- Donohue and McDowall 2021. ↵
- Chodor and Hameiri 2022. ↵
- Ramia and Perrone 2021. ↵
- COVID-19 National Incident Room Surveillance Team 2021. ↵
- Goldfinch, Taplin and Gauld 2021; Tranter 2022. ↵
- Bromfield and McConnell 2021, 527. ↵
- Bromfield and McConnell 2021. ↵
- Drennan, McConnell and Stark 2015, 31. ↵
- Department of Health and Aged Care 2021, 2022. ↵
- COVID-19 National Incident Centre Surveillance Team 2022. ↵
- Australian Labor Party 2022; Liberal Party of Australia 2022. ↵
- Shepherd 2022. ↵
- McConnell 2020. ↵
- Boin, McConnell and Hart 2008, 309–12. ↵
- Boin, McConnell and Hart 2008, 312. ↵

