Organisation and governance
Implementation of Complex Interventions in Health Services
Hanan Khalil
Introduction
Complex interventions in health services are defined as interventions with multiple interacting components (Greenhalgh and Papoutsi, 2018). They usually include changes to health care professionals’ diagnostics and treatments approaches, and operational systems such as electronic medical records, health technology, and systems in organisations (O’Cathain et al., 2019). Complexity arises from the dynamic nature of the health system and the funding models involved to operate certain activities (O’Cathain et al., 2019). Other sources of complexity may arise from the challenging behaviours of personnel involved, number of groups or organisations targeted, number and types of outcomes, and the degree of adaptability required for the implementation stage of any intervention (Craig et al., 2011).
Simple interventions usually involve drug trials where researchers and clinicians test the efficacy of a particular drug on a condition or a disease; whereas complex interventions usually involve a minimum of three main components, such as what should healthcare workers do, what qualifications should they have, and what should patients do? (Ma et al., 2020). Moreover, Ma et al. (2020) identified five main aspects of complex interventions adopted in the implementation process: psychological support, cognitive support, behavioural support, social support, and environmental support (Wade and Halligan, 2017).
The importance of this topic lies in its applicability to health managers. Health managers face challenges in making decisions about budgeting, staff, resources allocation, and operational management of their units. Understanding the processes involved in implementing complex interventions creates the potential for their successful adoption in the workplace and ensuring that they are feasible and integrated in everyday practice. This chapter covers the components of complex of intervention, and their design, implementation, and evaluations in health services.
Background and context
In 2000, the United Kingdom Medical Research Council published guidelines for the development of complex interventions that highlighted assessing and evaluating the effectiveness of components of complex interventions (M. Campbell et al., 2000). The authors included interventions such as service delivery and organisations (i.e., cardiac units and hospital in the home), interventions directed at health clinicians (i.e., computer decision support systems and implementation of guidelines), community interventions (community programs to prevent stroke and primary care approaches to improve health), group interventions (behavioural change strategies and reduction of smoke in teenage pregnancy), and individual therapy (cognitive therapy for mental health conditions).
In 2008, the new Medical Research Council guidelines were revised in response to the limitations encountered with the framework. (Craig et al., 2008) Examples of these limitations included lack of piloting of interventions at early stages, integration of processes and outcome measures in the evaluation, and understanding the context of where the interventions were being implemented. Since the first guidelines were published, various studies on complex interventions have been conducted, which resulted in some interventions being implemented with various success (Craig et al., 2008).
In 2021, a new framework was devised by the same group of authors. (Skivington et al., 2021) The new framework defines evaluation as going outside complex interventions efficacy and spanning its parameters to include whether the impact of other external factors on its implementation in the real world is significant, hypothesising how it works, taking account of how it interacts with the setting in which it is applied, and how the evidence generated can be used to facilitate decision making in realistic scenarios. Other aspects of interventions, such as cost effectiveness, scalability and transferability across various contexts are all equally important and should be considered when assessing any complex intervention (Skivington et al., 2021).
The shift towards other measures of complex interventions research arises from what decision makers require, as some research questions cannot be answered by addressing efficacy and effectiveness. Examples of various research questions proposed by funders or hospital managers could include the following:
- Is the intervention cost-effective?
- What other changes may happen as a consequence of this intervention?
- Will the intervention work across other settings?
- When there is no evidence generated from robust research methods, such as randomised controlled trials, how feasible is the intervention to be implemented and what its degree of success?
The table below illustrates the four main research questions covered by this new framework, with examples and key considerations for health managers. Skivington et al., 2021) The main research questions include efficacy, effectiveness, theory-based, and systems. The new approach aims to encompass all the potential questions by decision makers in implementing complex interventions.
Research perspectives covered by the new framework (Skivington et al., 2021)
| Research question | Example | Key considerations |
| Efficacy | The efficacy and safety of a particular drug or vaccine in a certain population. | Seeks to understand the extent of an intervention producing a particular outcome in experimental or ideal settings. |
| Effectiveness | The efficacy of a particular program in real life settings. | Seeks to understand the extent of an intervention, that is, immunisation program in a real-world situation in terms of what it is supposed to do (i.e., prevent the spread of a disease). |
| Theory-based | Why the effectiveness of certain interventions varies across contexts, and what might be explored behind effectiveness? | Seeks to understand how changes are brought about. |
| Systems | How is the intervention adapted to the current system? | Explores the dynamic of rolling out an intervention across a system and its impact on other programs, systems, departments, and so on. |
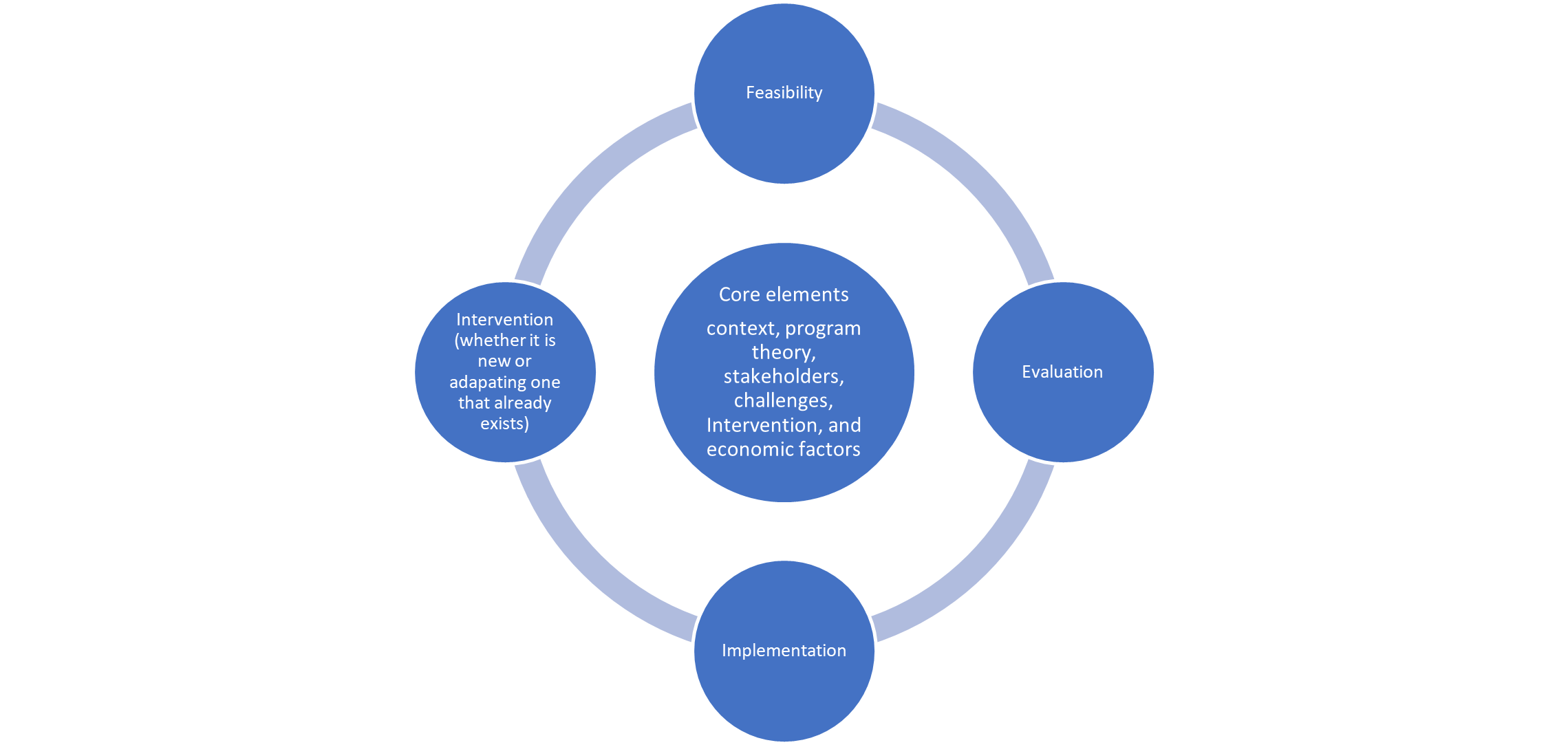
The above framework divides complex intervention into four stages: development of the intervention, feasibility, evaluation and implementation. (Skivington et a., 2021) Each stage has a common set of core elements considering the context, developing program theory, stakeholder involvement, identifying any areas that might seem challenging, refining or adapting the intervention, and economic factors. The figure below shows the core elements of context, program theory, involvement of stakeholders, choice of intervention and economic factors.
Skivington et al., 2021 framework takes into account other factors of interventions success beyond its effectiveness in the complex health care system that we are currently facing. By also including theories of change and other contextual factors, the framework provides a broader picture about how and why certain interventions work and moving beyond one dimension of evaluation of interventions. The next section covers the various theories/models currently used in implementation science for complex interventions.
Theory/models – Current evidence
Various theories, models, and frameworks noted in the literature of implementation science are used by clinicians to implement complex health interventions in any health care setting. Implementation science is about how interventions work in real life and how they are being used (Khalil, 2016). Identification of barriers and facilitators is crucial in this process to ensure the success of the intervention (Bauer and Kirchner, 2020). Before we describe these briefly in this section, it is important to define these terms and differentiate between them. First, a theory is defined as a set of principles or statements to structure observation, understanding, and explain a particular phenomenon. (Frankfort-Nachmias and Nachmias, 1996) A “good” theory provides a clear description of how and why specific relationships lead to certain events (Frankfort-Nachmias and Nachmias, 1996). A model usually involves an explanation of a particular phenomenon (Frankfort-Nachmias and Nachmias, 1996). Models do not have to be completely precise representations of reality to have value. Models and theories are very closely related to each other and are sometimes used interchangeably. Models can be described as theories with a more narrowly defined range of explanation; a model is descriptive, whereas a theory is explanatory, and may also be descriptive, as suggested by Frankfort-Nachmias and Nachmias (1996). On the other hand, a framework denotes a structure, overview and the relationship between each of its components, similar to the one mentioned above.(Khalil et a., 2019) Frameworks do not provide explanations, but describe various phenomena and try to fit them into a structure or categories. (Khalil et al., 2019) The three overarching aims for the use of theories, models and frameworks for complex interventions in health care are as follows:
- Describe and guide the process of evidence translation into practice
- Understanding what influences implementation outcomes
- Evaluation of implementation
Based on the stated aims and descriptions of these theories, models, and frameworks, these approaches are further classified into the following sections, as adapted from Nilsen, 2020.
- Determinants frameworks
- Classic theories
- Implementation theories
The following sections detail some of the models/theories and frameworks discussed in the literature.
Process models
The aim of these models is to facilitate translation of evidence into practice. Various process models are described in the literature, including the Canadian Institute of Health Research Model of Knowledge Translation (Canadian Institutes of Health Research, 2007), the Knowledge to Action model (Rycroft-Malone and Bucknall, 2010), the Iowa model (Collaborative et al., 2017), the Ottawa model (Gifford et al., 2017), and the Quality Implementation framework (Gifford et al., 2017). Most process models consist of steps to guide clinicians in evidence translation. For example, the Canadian Institute of Health Research Model of Knowledge Translation consists of six stages where knowledge translation occurs, including defining research questions, conducting research, publishing research findings, placing research findings into context of various cultures, making decisions and taking actions informed by research findings, and finally, influencing subsequent rounds of research (Sudsawad, 2007).
Determinants frameworks/classic theories/implementation theories
The aim of these models/theories and frameworks is to understand what influences the outcomes of implementation. Examples of these include Promoting Action on Research Implementation in Health Services (PARIHS) framework (Harvey and Kitson, 2015), the consolidated Framework for Implementation Research (CFIR) (Damschroder and Lowery, 2013) , Theoretical Domains framework (Rycroft-Malone, 2004) , and Theory of Diffusion and Normalisation Process theory (Murray et al., 2010), to name a few. The most commonly used model in this list is the PARIHS framework was initiated in 2011, as it has been cited widely in the literature and was updated in 2016 (Stetler et al., 2011, Harvey and Kitson, 2015). The model highlights that successful implementation is specified in terms of goal achievement and usually results from the facilitation of an innovation, with the recipients being an organisation or a health system (Hockley et al., 2019). The core components of this framework include facilitation, innovation, understanding recipients’ needs, and context. Context has previously been defined by Titler (2018) as the physical setting of the implementation; however, in this approach, it includes the characteristics and dynamic nature of the environment likely to have an impact on the implementation of the intervention. Social factors are also included pertaining to the roles, relationship, and dynamics of the individuals with each other (Titler, 2018).
Evaluation frameworks
This is one of the most important frameworks to health managers and clinicians, as these are essential in specifying the various aspects of any intervention to determine its success. One of the most common frameworks is the RE-AIM framework by Glasgow et al., (2001). Other frameworks are also used, such as the PRECEDE-PROCEED by Porter et al. (2016). These are further explained in the evaluating health and social care chapter.
The remainder of this section focusses on a newer model titled the Triple C model (consultation, collaboration, and consolidation) (Khalil and Kynoch, 2021). This model is useful for translating evidence into practice and understanding what influences the outcome of any complex implementation. It also ensures the sustainability of implementing any interventions (Khalil, 2017, Khalil and Kynoch, 2021).
The Triple C model (consultation, collaboration and consolidation)
This model was developed using a two-stage process, including a literature review to map the existing models for implementing complex interventions and investigating their barriers and facilitators using a scoping review methodology, followed by devising the framework using a formal theory building used in sociology. (Sudsawad, 2007) This model has been successfully used by other authors to build theoretical concepts (M. Campbell et al., 2000, S. M. Campbell et al., 2001). It allows researchers to evaluate the generalisability of the framework to other settings and support congruence and reliability in different situations (M. Campbell et al., 2000). The criteria upon which the theory was built are outlined below:
- It must have a precise description.
- It must have a logical explanation.
- It must establish information claims.
- It must be fit for purpose.
The model relies greatly on human resources (Khalil and Kynoch, 2021). Having a robust understanding of human performance, decision-making during significant situations, and recognising challenging issues are key considerations and have the potential to affect the success or failure of a project’s implementation.
The Triple C model represents successful research implementation as a function of the relationships among consultation, collaboration, and consolidation. (Khalil and Kynoch, 2021). The proposal is that for implementation to be successful and sustainable, there needs to be a continuing consultation, collaboration, and consolidation among all stakeholders involved in the project. Consultation should be a continuous process that starts early in the implementation process where continuity is an integral part of the process. Continuity requires ongoing dialogue with the various stakeholders. Collaboration and teamwork are essential to the success of any implementation project. Collaboration involves five main steps: first, identifying any barriers that may impede the implementation process. One of the major barriers to effective collaboration is the conflicting needs, objectives, and priorities of the stakeholders involved in the implementation process. Second, recruiting the right team with the right skills required for the project. Third, identifying an agreed direction for the implementing team. A clear sense of directions helps to turn individuals into teams sharing common goals and objectives. Fourth, clarifying responsibility in the implementation project is crucial for its success; this step relies on matching the right skills of the individuals with corresponding roles in the project. The last step in the collaboration process is the support of the team through relevant resources for the project. The consolidation stage is the most important part of the implementation process, as it ensures the sustainability and longevity of the project. Consolidation is defined as “an action or process of making something stronger or more solid” (Khalil 2017). The key role of consolidation is to incorporate an adaptable process to ensure the viability of the implementation. The success of the consolidation process relies on the development of procedures or processes that can become business as usual following the life of the project. This step also requires consultation and collaboration; hence, the continuing nature of the model is essential to its success.
Efficient teamwork requires cooperation, coordination, and communication between the various team members (Shediac-Rizkallah and Bone, 1998). Effective communication between and within teams enables cooperation and coordination. To support success every member of the team requires an understanding of the purpose, team roles, responsibilities, task requirements and the project plan. Trust in other team members and sharing information are also essential to enable cooperation between teams (Shediac-Rizkallah and Bone, 1998).
Key implications for practice (barriers and facilitators)
Several barriers and facilitators have been recognised in the literature regarding implementation and evaluation of complex interventions. Kormelinck and colleagues (2021) identified five domains that should be considered when planning to implement and evaluate complex interventions. These included intervention characteristics, outer settings, inner setting, characteristics of individuals involved in the intervention, and the process used.
The complexity of the intervention is addressed in various studies as a barrier to successful implementation and evaluation, which is not a surprise, as the perceived easiness of the intervention will contribute to its success or failure in the system. This is especially relevant for interventions that encourage takes to be undertaken as part of individuals’ normal roles on the job (Kormelinck et al., 2021).The notion of adaptability of the intervention aligns well with the complexity issue as a facilitator, as the success of interventions will depend on their integration into normal day to day practice (Kormelinck et al., 2021).
The second domain highlighted in the literature is the outer setting, including patients’ needs, external policy, and accreditation requirements as essential to be considered as main elements for the success of any implementation process, aligning the needs of the external stakeholders with the intervention ensures its uptake and likely success (McAiney et al., 2007, Boersma et al., 2015)
The third domain consists of inner settings, which are related to staff communications and collaborative relationships between the various stakeholders to ensure the success of the intervention. Other characteristics such as the organisational culture have been identified as both facilitators and barriers. (Boersma et al., 2015 and Bourbonnais et al., 2020) Other constructs, such as leadership and management, available resources for staff are essential for the success of this domain. (Boersma et al., 2015 and Bourbonnais et al., 2020)
Individuals’ characteristics and their self-belief about their capacity to undertake the tasks requested by them is also crucial, staff feelings and their validation have been documented in the literature as a factor of success of the process. (Mekki et al., 2017) Other personal attributes such as their knowledge, and willingness to adapt and learn are also key factors for the success of the implementation that should not be undermined (Mekki et al., 2017).
Finally, and most importantly, the process of implementation and engaging with the various stakeholders is a key contributor to enable organisational challenges, such as staff turnover and transfer of information between the various departments. (Bourbonnais et al., 2020).
Engaging champions has also been acknowledged as crucial to the success of any implementation process (Bourbonnais et al., 2020).
Case history vignettes demonstrating the practical application of the topic
This section provides examples of how models such as the Triple C have been used to implement complex interventions in healthcare.
Case Vignette 1
The Triple C model was used in the implementation of an electronic wound care program across several health services to follow would healing and costs in rural Victoria in Australia (Khalil et al., 2016). Khalil et al 2014 used the triple C model to implement an electronic wound care system across 11 organisations across a region to track the types of wounds managed by community nurses in terms of healing times and costs associated with the overall treatment. The program’s implementation led to a substantial enhancement of wound healing times, and reducing dressing usage resulting in better healing and less costs incurred by the health service. (Khalil et al., 2015) The consultation stage was used to prioritise areas of research and plan for the project’s delivery. Adequate resources were made possible by ensuring stakeholders participated early in the project through both in kind and financial resources. The collaboration stage was vital, as this project engaged multiple health services and training programs to support the successful delivery of the project across multiple sites. The consolidation stage included the development of standardising policies and procedures across all sites on management of wounds across the rural region and the initiation of a regional wound consultant role. These approaches ensured the long-term sustainability of the program. The project was supported by a research team to examine data quality across the sites to ensure the uniformity of the implementation plan across the various participating sites. This project led to a program of educational training to clinicians involved on the most frequent wounds they experienced in the region, which was then embedded in several organisations as part of continuous improvement.
Case Vignette 2
The second project where the Triple C model was used was in the implementation of a medication safety program in an Aboriginal health organisation in a large regional area in Australia. (Khalil and Gruis 2019) The aim of the project was to implement a culturally safe and relevant medication safety education program to Aboriginal Health Care workers and build an online resource to ensure its access to all staff at any time (Khalil and Gruis, 2019, Khalil, 2019). The Triple C was used to implement and monitor the research involved with the program. The first stage was consultation, where initial interviews were conducted to understand and examine any medication safety issues in the Aboriginal community. (Khalil, 2019) This led to the formation of a process map about the intervention to inform the implementation of a medication safety program for the organisation. The collaboration stage consisted of identifying and engaging the staff necessary to deliver the medication safety intervention. In this case, the intervention consisted of a medication safety program and formation of policies addressing medication safety issues. The consolidation stage of the project involved data collection to monitor the efficiency of the programs and making the resources and policies available to all staff through an online platform.
Case Vignette 3
Another project where the Triple C model was utilised was the development of a skills matrix to identify areas of need to upskill palliative care nurses (Khalil, Byrne, and Ristevski, 2019, Khalil et al., 2019b). Previous research identified inadequate knowledge in this area of palliative care in rural areas (Khalil et al., 2019b). Several discussions with managers took place focussing on how to best capture the educational needs of staff. Once a plan was devised, a process map addressing the implementation of the project was devised that included the design of a skills matrix for managers to use to identify staff educational needs. The consolidation stage involved the use of this matrix as a standard form for staff assessments and discussion about occasions for future developments. This process led to the development of targeted educational interventions to address the gaps identified by the skills matrix.
Case Vignette 4
A final example of a project using the Triple C model in practice was the implementation of the validated Distress Thermometer to improve detection, evaluation and management of distress in the cancer care inpatient wards (Stephens, 2019). Initially, the project started with discussion with all identified stakeholders to encourage staff encouragement and to identify areas of improvement. This was followed by devising a procedure for patient distress management of patient in partnership with multidisciplinary teams across oncology. The design of strategies to enhance practice, including programmes such as teaching meetings on identifying and managing distress for patients and debrief sessions for staff, were implemented. The consolidation stage, which considered the sustainability, involved changes to current documentation, as well as the availability of a patient information booklet for patients and families to maintain the changes.
Key Takeaways
For leaders – You will know you are successful if…
Successful implementation of complex interventions in health services relies on several factors, including choosing the right model of implementation that clearly articulates the objective of the intervention and the reason for its implementation. This is followed by clear expectations and guidance from all those involved to implement and evaluate the intervention, and engaging champions and leaders to role model and provide guidance as the process unfolds.
You will know you are successful when you succeed in managing the above factors and consider all aspects of a project’s implementation and evaluation. Moreover, identifying any barriers and facilitators at the outset of project implementation will allow a clearer map of the whole process.
References
Bauer, M.S. and Kirchner, J. 2020. Implementation science: What is it and why should I care?. Psychiatry Research, 283, p.112376.
Boersma, P., Van Weert, J. C., Lakerveld, J. and Dröes, R. M. 2015. The art of successful implementation of psychosocial interventions in residential dementia care: a systematic review of the literature based on the RE-AIM framework. International Psychogeriatrics, 27(1), pp.19-35.
Bourbonnais, A., Ducharme, F., Landreville, P., Michaud, C., Gauthier, M. A. and Lavallée, M. H. 2020. An action research to optimize the well-being of older people in nursing homes: challenges and strategies for implementing a complex intervention. Journal of Applied Gerontology, 39(2), pp.119-128.
Canadian Institutes of Health Research. 2007. Knowledge Translation [KT] within the Research Cycle Chart. Ottawa: Canadian Institutes of Health Research. Reproduced with the permission of the Minister of Public Works and Government Services Canada, 2007.
Campbell, M., Fitzpatrick, R., Haines, A., Kinmonth, A. L., Sandercock, P., Spiegelhalter, D. and Tyrer, P. 2000. Framework for design and evaluation of complex interventions to improve health. BMJ, 321(7262), pp.694-696.
Campbell, S. M., Hann, M., Hacker, J., Burns, C., Oliver, D., Thapar, A., Mead, N., Safran, D. G. and Roland, M. O. 2001. Identifying predictors of high quality care in English general practice: observational study. BMJ, 323(7316), p.784.
Craig, P., Dieppe, P., Macintyre, S., Michie, S., Nazareth, I. and Petticrew, M. 2008. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ, 337.
Collaborative, I.M., Buckwalter, K.C., Cullen, L., Hanrahan, K., Kleiber, C., McCarthy, A.M., Rakel, B., Steelman, V., Tripp-Reimer, T. and Tucker, S. 2017. Iowa model of evidence-based practice: Revisions and validation. Worldviews on Evidence-based Nursing, 14(3), pp.175-182.
Damschroder, L.J. and Lowery, J.C. 2013. Evaluation of a large-scale weight management program using the consolidated framework for implementation research (CFIR). Implementation Science, 8, pp.1-17.
Frankfort-Nachmias, C. and Nachmias, D. 1996. Research methods in the social sciences. London: Edward Arnold. Community Watershed Management in Semiarid India, 187.
Gifford, W., Graham, I. D., Ehrhart, M. G., Davies, B. L. and Aarons, G. A. 2017. Ottawa model of implementation leadership and implementation leadership scale: mapping concepts for developing and evaluating theory-based leadership interventions. Journal of Healthcare Leadership, pp.15-23.
Glasgow, R. E., McKay, H. G., Piette, J. D. and Reynolds, K. D. 2001. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management?. Patient Education and Counseling, 44(2), pp.119-127.
Greenhalgh, T. and Papoutsi, C. 2018. Studying complexity in health services research: desperately seeking an overdue paradigm shift. BMC Medicine, 16, pp.1-6.
Harvey, G. and Kitson, A. 2015. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implementation Science, 11(1), pp.1-13.
Hockley, J., Froggatt, K., Van den Block, L., Onwuteaka-Philipsen, B., Kylänen, M., Szczerbińska, K., Gambassi, G., Pautex, S. and Payne, S. A. 2019. A framework for cross-cultural development and implementation of complex interventions to improve palliative care in nursing homes: the PACE steps to success programme. BMC Health Services Research, 19, pp.1-11.
Khalil, H., 2016. Knowledge translation and implementation science: what is the difference?. JBI Evidence Implementation, 14(2), pp.39-40.
Khalil, H., 2017. The triple C (consultation, collaboration and consolidation) model: a way forward to sustainability of evidence into practice. JBI Evidence Implementation, 15(2), pp.40-42.
Khalil, H., 2019. Successful implementation of a medication safety program for Aboriginal Health Practitioners in rural Australia. Australian Journal of Rural Health, 27(2), pp.158-163.
Khalil, H. 2019b. ‘Successful implementation of a medication safety program for Aboriginal Health Practitioners in rural Australia’, Australian Journal of Rural Health, 27(2), pp. 158–163. doi:10.1111/ajr.12494
Khalil, H., Byrne, A. and Ristevski, E. 2019. The development and implementation of a clinical skills matrix to plan and monitor palliative care nurses’ skills. Collegian, 26(6), pp.634-639.
Khalil, H., Cullen, M., Chambers, H., Carroll, M. and Walker, J. 2015. Elements affecting wound healing time: an evidence based analysis. Wound Repair and Regeneration, 23(4), pp.550-556.
Khalil, H., Cullen, M., Chambers, H., Carroll, M. and Walker, J. 2016. Reduction in wound healing times, cost of consumables and number of visits treated through the implementation of an electronic wound care system in rural Australia. International Wound Journal, 13(5), pp.945-950.
Khalil, H., Cullen, M., Chambers, H., Steers, N. and Walker, J. 2014. Implementation of a successful electronic wound documentation system in rural Victoria, Australia: a subject of collaboration and community engagement. International Wound Journal, 11(3), pp.314-318.
Khalil, H. and Gruis, H. 2019. ‘Medication safety challenges in Aboriginal Health Care services’, Australian Journal of Rural Health, 27(6), pp. 542–549. doi:10.1111/ajr.12554.
Khalil, H. and Kynoch, K. 2021. Implementation of sustainable complex interventions in health care services: the triple C model. BMC Health Services Research, 21, pp.1-10.
Khalil, H., Poon, P., Byrne, A. and Ristevski, E. 2019. Medication safety challenges in the palliative care setting: Nurses’ perspectives. Collegian, 26(6), pp.640-644.
Kormelinck, C. M. G., Janus, S.I., Smalbrugge, M., Gerritsen, D. L. and Zuidema, S. U. 2021. Systematic review on barriers and facilitators of complex interventions for residents with dementia in long-term care. International Psychogeriatrics, 33(9), pp.873-889.
Ma, S., Yu, H., Liang, N., Zhu, S., Li, X., Robinson, N. and Liu, J. 2020. Components of complex interventions for healthcare: A narrative synthesis of qualitative studies. Journal of Traditional Chinese Medical Sciences, 7(2), pp.181-188.
McAiney, C. A. Stolee, P., Hillier, L. M. Harris, D., Hamilton, P., Kessler, L., Madsen, V. and Le Clair, J. K. 2007. Evaluation of the sustained implementation of a mental health learning initiative in long-term care. International Psychogeriatrics, 19(5), pp.842-858.
Mekki, T.E., Øye, C., Kristensen, B., Dahl, H., Haaland, A., Nordin, K.A., Strandos, M., Terum, T. M., Ydstebø, A. E. and McCormack, B. 2017. The inter‐play between facilitation and context in the promoting action on research implementation in health services framework: A qualitative exploratory implementation study embedded in a cluster randomized controlled trial to reduce restraint in nursing homes. Journal of Advanced Nursing, 73(11), pp.2622-2632.
Murray, E., Treweek, S., Pope, C., MacFarlane, A., Ballini, L., Dowrick, C., Finch, T., Kennedy, A., Mair, F., O’Donnell, C. and Ong, B.N., 2010. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Medicine, 8, pp.1-11.
Nilsen, P., 2020. Overview of theories, models and frameworks in implementation science. In Handbook on implementation science (pp. 8-31). Edward Elgar Publishing.
Rycroft-Malone J, Bucknall T. 2010. Models and Frameworks for Implementing Evidence-Based Practice: Linking Evidence to Action. Oxford: Wiley-Blackwell;
2010.
O’Cathain, A., Croot, L., Duncan, E., Rousseau, N., Sworn, K., Turner, K.M., Yardley, L. and Hoddinott, P. 2019. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open, 9(8), p.e029954.
Porter, C. M. 2016. Revisiting Precede–Proceed: A leading model for ecological and ethical health promotion. Health Education Journal, 75(6), 753–764. https://doi.org/10.1177/0017896915619645
Rycroft-Malone, J. 2004. The PARIHS framework—a framework for guiding the implementation of evidence-based practice. Journal of Nursing Care Quality, 19(4), pp.297-304.
Shediac-Rizkallah, M. C. and Bone, L. R. 1998. Planning for the sustainability of community-based health programs: conceptual frameworks and future directions for research, practice and policy. Health Education Research, 13(1), pp.87-108.
Skivington, K., Matthews, L., Simpson, S. A., Craig, P., Baird, J., Blazeby, J. M. Boyd, K. A., Craig, N., French, D. P., McIntosh, E. and Petticrew, M. 2021. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ, 374.
Stetler, C. B., Damschroder, L. J., Helfrich, C. D. and Hagedorn, H. J. 2011. A guide for applying a revised version of the PARIHS framework for implementation. Implementation Science, 6(1), pp.1-10.
Sudsawad, P. 2007. Knowledge translation: Introduction to models, strategies and measures. Austin, TX: Southwest Educational Development Laboratory, National Center for the Dissemination of Disability Research.
Titler, M. G. 2018. Translation research in practice: an introduction. Online Journal of Issues in Nursing, 23(2).
Wade, D. T. and Halligan, P. W. 2017. The biopsychosocial model of illness: a model whose time has come. Clinical Rehabilitation, 31(8), pp.995-1004.

