Organisation and governance
Systems Thinking in Health and Social Care Delivery: An Overview
Systems thinking in health and social care delivery: An overview
Ali Lakhani and Hanan Khalil
Introduction
Health is fundamental to a thriving and successful population, community, and economy, and delivering this is contingent upon a strong health and social care system. A health and social care system is made up of a number of components, including, but not limited to: primary, secondary, and emergency care; the health workforce; health information systems; pharmaceutical dispensing systems; and financing and leadership/governance. Inevitably, complexity arises with diverse systems, services, and processes. The complexity of health and social care can be due to several issues, including difficult conditions and circumstances experienced by consumers and patients presenting for care, clinician experience, and knowledge and the structural arrangement of the healthcare organisation (Trbovich, 2014). This has also been complicated by the advancement of medical technologies that require clinicians to be familiar with technology, as well as interacting with the components of a healthcare system and associated workforces. Several methodologies have been used to test, implement, and evaluate interventions in the health system with varying degrees of success, partly due to this complexity and the evolving nature of the current health care system (Wiig et al., 2014).
A system is a connection of variables that result in a behavioural pattern (Meadows, 2008). Systems are not unique to any discipline or field of inquiry. They are generally characterised as involving elements (factors or variables), connections between elements, and a boundary that establishes what resides within the system and what is outside (Williams and Hummelbrunner, 2010). The elements within the system interact and/or are influenced by outside factors that result in outcomes. Thus, systems thinking is a holistic approach to examining the factors and interactions that contribute to outcomes. Systems thinking focuses on the dynamic interaction, harmonisation, and integration of individuals, processes, and technology by addressing the interconnecting factors between the different layers of the health system (Linnéusson et al., 2022). The advantages of applying systems thinking to solve complex problems in healthcare include its ability to apply a holistic approach to problem-solving. The benefits of a systems thinking approach are its advantages of nurturing great leaders committed to positive changes, its proactive approach to identify leverage points and creating a culture, integrating higher thinking, and creativity in the problem-solving of complex issues in health and social care. This chapter covers many aspects of how system thinking can be used to solve complex problems in healthcare.
Background
Healthcare delivery is consistently faced with ‘wicked’ or complex problems. The concept of wicked or complex problems (hereafter described as complex problems) was initiated by Rittel and Webber (1973). Such problems are socially complex, unable to be addressed by a single group or stakeholder, and fit a set of criteria (Australian Public Service Commission, 2007), including being multicausal, being difficult to define, and having multiple interdependencies. They are constantly evolving, and interventions that aim to address the problem usually result in unforeseen consequences (Australian Public Service Commission, 2007, Williams and Hummelbrunner, 2010). Thus, simple solutions are non-existent, and instead, strategies to address rather than solve remain the best option. Examples of society level complex problems include obesity (Frood et al., 2013), climate change (Head, 2014), and homelessness (Norman-Major, 2018). Since the identification of complex problems, such problems have been considered across diverse disciplines, including health administration (Rusoja et al., 2018).
Increasingly, health administration and management problems are recognised as complex. For example, Rozario (2019) described the severity of physician burnout, and particularly highlighted how a combination of interrelated factors, including competition for employment, poor resourcing, increasing caseloads and administrative workloads, alongside a backdrop of a continual threat of litigation contribute to prevalent physician burnout. Rozario (2019) confirmed that effective strategies to manage complex problems must be developed from diverse stakeholders who are impacted by and contribute to the problem. Whilst, in relation to the delivery of health care, Periyakoil (2007) clarified a diversity of palliative health care problems as complex, including end-of-life decision making, aggressive treatments, and communication problems. Additionally, while stigma around mental health issues persist as a complex problem (Henderson and Gronholm, 2018), the provision of high-quality physical care (for example, wound care) amongst those experiencing mental health issues is also characterised as complex (Samuriwo and Hannigan, 2020).
Systems Thinking Approaches: Addressing Wicked Problems in Health Care Delivery
Systems level approaches – informed by systems thinking – have been identified as ideal methods to address complex problems, and particularly, complex problems surrounding the delivery of health care (Samuriwo and Hannigan, 2020). Systems thinking can be characterised as a way of seeing the world. In relation to addressing problems, using a systems thinking perspective involves moving beyond traditional mechanistic, linear methods of understanding and addressing problems reliant on the expectation that problems fall neatly into a cause and effect relationship (Chapman, 2004). Instead, strategies to address problems need to consider diverse perspectives (for example, perspectives from different disciplines and stakeholders with different experiences relating to an issue), and be aware of interrelationships (the notion that diverse factors contributing to a problem impact one another) and boundaries (that distinct elements fit within a problem) (Williams and Hummelbrunner, 2010). Systems thinking methods are approaches that aim to develop understanding around and strategies to address problems, while considering these domains (perspectives, relationships, and boundaries) (Williams and Hummelbrunner, 2010). The application of systems thinking methods as an approach to treat complex problems in health care delivery is increasing (Rusoja et al., 2018), and these methods are expected to continue to have an important role to play, given an ageing demographic living longer with chronic conditions and disability.
Systems thinking is characterised as big picture thinking, and methods aligned with systems thinking attempt to consider the macro-level picture, while also being cognisant of micro elements that are interrelated and contribute to a problem. Systems thinking methods are extensive, with specific methods better suited to particular problems (Williams and Hummelbrunner, 2010). Williams and Hummelbrunner (2010) described several systems thinking methods in their text, including systems dynamics modelling (an approach to understand how resources flow through a system), social network analysis (an approach used to understand relationships and the impact of these relationships), and systemic questioning (an approach used to broaden perspectives and/or identify and mobilise untapped resources). A detailed review of the extent of systems thinking approaches and their application to health administration problems is beyond the scope of this chapter. It is worthwhile to consider the application of widely used approaches in health administration and management, as increasing understanding in these areas can inform how health professionals address complex problems. The following section details some of the approaches used in systems thinking to solve complex problems.
Causal Loop Diagrams
A causal loop diagram (CLD) is a systems thinking method where relationships between diverse factors contributing to a problem are mapped (Williams and Hummelbrunner, 2010). It is a visual methodology, and key aspects of a causal loop diagram include factors (elements contributing to an issue), and the connections between these factors and the overarching problem (these illustrate the direction of a relationship). Connections between factors are denoted with a ‘+’ or ‘S’, which means that factors move in the same direction (an increase in one factor results in an increase in the connected factor); while connections denoted with a ‘-‘ or ‘O’ mean that factors move in the opposite direction (an increase in one factor results in a decrease in the connected factor) (Kim, 2011). Feedback loops are central to CLDs (Kim, 2011), and these can either be reinforcing or balancing. Feedback loops emerge as multiple factors impact upon one another in a circular fashion. Simply put, a change within a single factor has an impact on interrelated factors in such a way that the initial factor is also impacted. Reinforcing feedback loops emerge when the change in a single factor causes changes in interrelated factors, which eventually amplifies the same change in the initial factor (for example, a reinforcing loop would mean that an initial positive change is amplified). Whilst balancing loops are feedback loops where an initial positive change in a factor impacts interrelated factors in a way that produces a reduction in the initial factor (thus, producing a diminishing effect in the initial factor). Feedback and balancing loops are important because they can become leverage points for interventions to produce change.
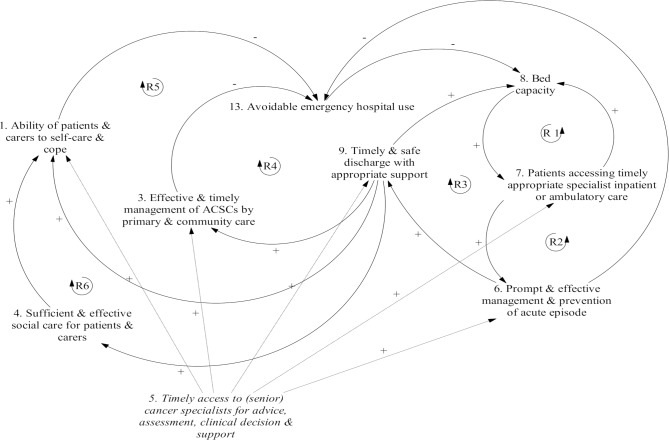
Causal Loop Diagram Application
Increases in emergency department presentations for people with mental health conditions, cancer, or other chronic disease are complex problems. Increased emergency department presentations are due to a variety of factors, including a growing population, a rise in complex health issues among an ageing population, and health and social service pathways that prioritise referrals to emergency departments (Chen et al., 2019). Chen et al. (2019) suggested a poor understanding around contributing factors and the interrelationship between these factors; thus, employing a systems thinking approach could assist in generating knowledge. They interviewed senior clinicians with the aim of developing a CLD to map factors contributing to emergency department presentations. The CLD they developed was used to explain the drivers of emergency cancer care. The figure below, (taken from Chen et al.’s article), illustrates these drivers and their interrelationships. Twelve direct and indirect drivers of avoidable emergency hospital presentations included the ability for patients and carers to self-care, timely and safe discharge with appropriate support, and professionals’ knowledge and skills in accessing services and referring patients (Chen et al., 2019).
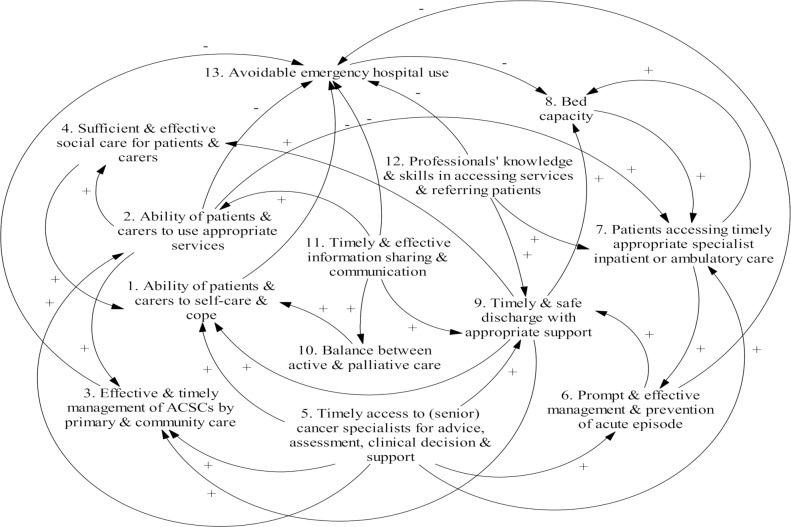
Relationships between drivers were explored and reinforcing loops articulated within the figure shown below (Chen et al., 2019). A review of reinforcing loops assisted in identifying a leverage point for intervention. They concluded that prioritising interventions that affect the eight factors contributing to the five reinforcing loops they identified could best address the issue of increased emergency department presentations. In this respect, they suggested that interventions and/or programs that promote timely access to specialist care could address factors embedded in reinforcing loops and assist in reducing avoidable emergency department presentations. As illustrated below, programs that improve timely access to specialist care can favourably impact: (i) patients and carers’ ability to self-care and cope, (ii) timely management by primary and community care, (iii) timely and safe discharge, (iv) accessing timely appropriate specialist inpatient or ambulatory care, and (v) prompt and effective management and prevention of acute episodes. The impact of such an intervention on the first of these two drivers was suggested to have a direct effect on avoidable emergency hospital use and produce a reduction in avoidable emergency hospital use. The later three were identified to have an indirect effect and also contribute to a reduction in avoidable emergency hospital use (Chen et al., 2019).
Soft Systems Methodology
The soft systems methodology is a qualitative systems thinking approach that aims to identify the impetus for change by exploring tensions between individual lived experiences, and systems perspectives (generated by collating the perspectives of diverse stakeholders). The approach was initiated in response to the inadequacy of problem solving approaches, which assumed that interrelationships are uniformly understood (Checkland and Scholes, 1999). It is a seven-step process where stakeholders: (i) identify the problem requiring response, (ii) develop a description of the problem scenario using rich pictures (or rich picture), (iii) develop root definitions of the problem situation based on diverse perspectives, (iv) develop models of the problem scenario and system informed by definitions, (v) compare rich picture descriptions to modelled descriptions, (vi) establish interventions for change in response to the tension derived from comparing rich picture and modelled descriptions, and (vii) take action to address the problem scenario. Steps 1 and 2 align with the real-world perspectives (individually based), while steps 3 and 4 align with the systems thinking world, which considers and integrates diverse perspectives relating to the issue and/or problem scenario. The soft systems methodology is increasingly being used to address problems in the delivery of healthcare, and in this capacity, is largely used to understand the dynamic perspectives and interpretations of a problem, and potential interventions to address the problem (Augustsson, Churruca, and Braithwaite, 2020).
Soft System Methodology Application
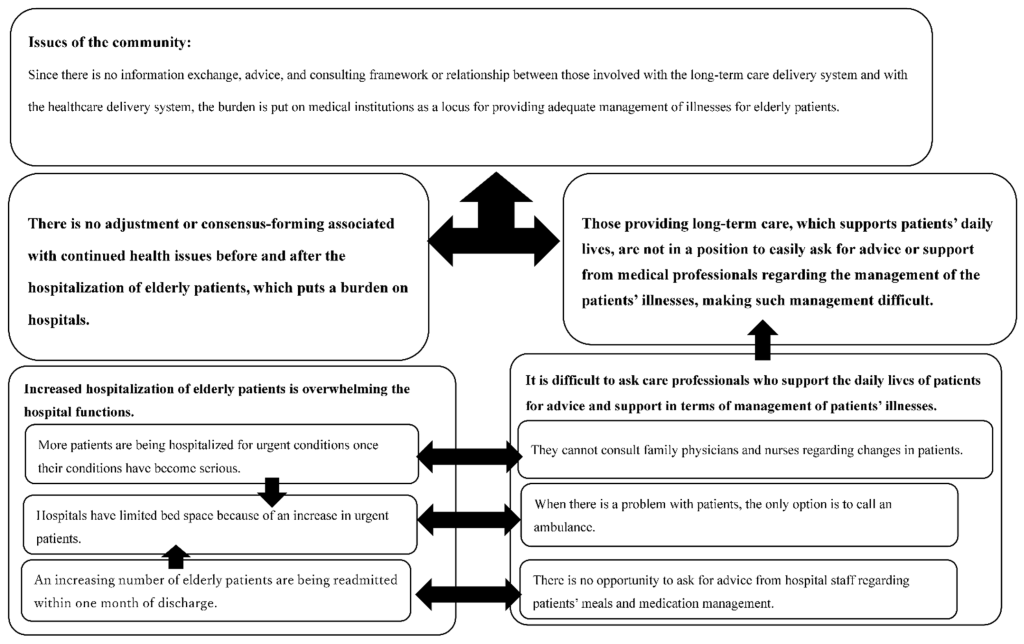
Ageing adults and people with complex disability often find themselves moving between residential and/or supported accommodation and hospital and health service and/or inpatient services (Australia Institute of Health and Welfare, 2020). Such movement can be challenging for end users and providers of care, with challenges around ensuring continuity of care to promote the best health outcomes. Distinct factors make offering responsive, high-quality coordinated residential aged and hospital care challenging, including (i) a general increase in demand for community and clinical services resulting from an ageing demographic, (ii) an increase in repeated hospitalisations due chronic conditions, (iii) a mix of fee-for-service, private health insurance, and public health insurance (for example, Medicare in Australia) payment options, (iv) the support required to ensure that ageing adults are able to make difficult decisions, and (v) differing understandings of the challenges experienced by end users (Goto and Miura, 2022). As a response to challenges in offering high-quality coordinated care, Goto and Miura (2022) utilised the soft systems methodology to ascertain issues and challenges resulting from linking healthcare and residential care delivery, and clarify solutions that could result in high-quality integrated delivery. Over a three-year period, community care coordinators (n=20) – coordinators responsible for ensuring service coordination across residential and hospital services – participated in workshops where group discussions were held to establish coordination challenges and solutions. Drawing on input from three coordinators within a single municipality, Goto and Miura (2022) followed a revised soft systems methodology. Issues identified surrounding the challenges of linking healthcare and residential care delivery contributed to a rich picture, where the dynamic interplay between coordination issues were synthesised, as illustrated in the figure below. As included within the rich picture below, healthcare issues identified include: (i) an increase of admissions based on urgent conditions, (ii) a lack of bed space due to increased urgent admissions, and (iii) and increasing number of inpatients readmitted within one month of discharge. Long-term residential care issues identified include: (i) inability (perhaps due to communication gap) to consult with doctors regarding resident health issues and/or symptoms, (ii) the need for advice around care required for patients post discharge, and (iii) given the expertise of care staff, the best option to support patients in need is to call an ambulance.
Given the rich picture, and further analysis of stakeholder perspectives resulting in the development of root definitions of the overarching issue, a conceptual model where characteristics of coordinated care responsive to the accumulative issues was developed. This model is shown below.
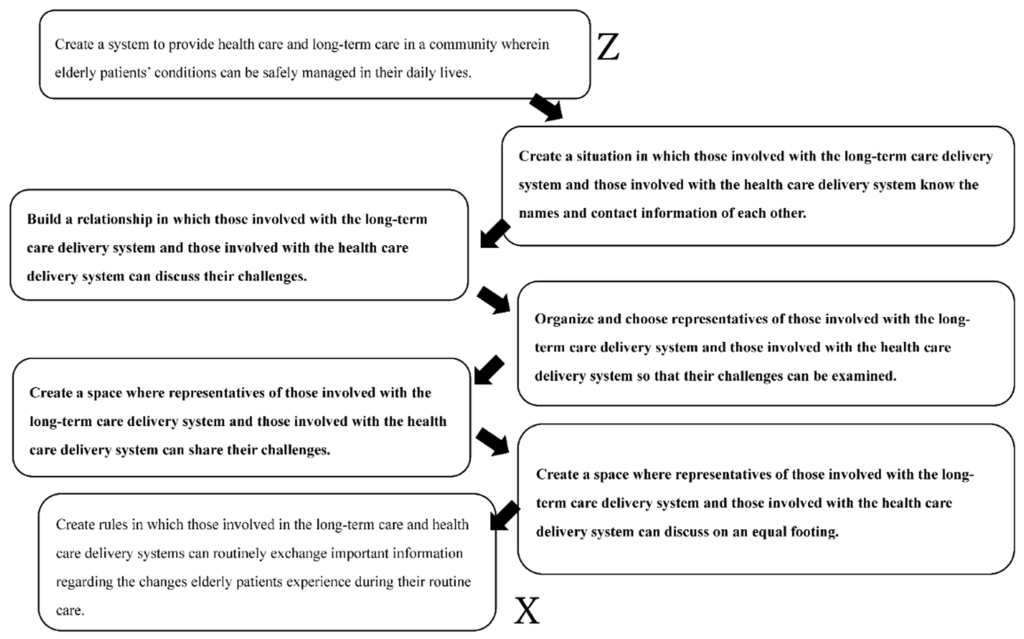
In summary, the model of care proposed involves ensuring that open lines of communication exist between individuals working within long-term care and hospital health services. This would allow for relationships between groups to be established, whereby challenges and opportunities could be discussed, and nominated representatives from both groups could explore challenges as they emerge. An equitable opportunity and space where representatives from both groups can present and discuss challenges is theorised by Goto and Miura (2022) as facilitating high-quality care responsive to the needs of end-users.
Implications for Practice
The case applications provided highlight the value of systems thinking approaches as a method to tackle complex problems in healthcare delivery. The diversity of methods aligning with systems thinking have value in distinct circumstances, and certainly, developing competencies around the implementation of methods. In particular, an understanding around methods best suited to address particular problems is an important and worthwhile endeavour. Initially, it is necessary to shift ways of thinking in healthcare organisations. In this respect, health and social care managers and leaders have a role to play, as they can foster an environment where those in the space are able to become systems thinkers, and value diverse perspectives, interrelationships between factors contributing to an issue, and understand boundaries. Healthcare leaders have a role in developing an environment where professionals can collectively learn and develop strategies to address complex problems (Senge, Hamilton, and Kania, 2015). Senge, Hamilton, and Kania (2015) suggested that systems leaders need to have three core capabilities to foster an environment where professionals can utilise systems thinking and collectively learn. These capabilities can be developed and consist of the ability to: (i) see the larger system, (ii) foster conversations and reflection, and (iii) change focus from reaction to co-creation. Senge, Hamilton, and Kania (2015) clarified a diversity of tools that leaders can engage with to promote their ability to build the three competencies, including the development of systems maps to see the larger system, and peer shadowing to foster conversations and reflection.
Key Takeaways
For Leaders – You Will Know You Are Successful If…….
System thinking approaches can support leaders to develop deeper insights, consider unexpected consequences, develop contingencies, and coordinate actions to manage complex problems in the health system (Hobbs and Midgley, 2020). As leaders, you will know if you are successful if you challenge assumptions, develop critical thinking, and explore wider contexts to solve complex problems. Strategic choices for decision making should include sharing multi-dimensional problems with others, and developing several options for solutions, then comparing them and choosing what it is best for the problem at hand. You will also know that you are successful if you manage to engage others and allow them to share their perspectives of the complex problem at hand, identify possible solutions, reflect on them, and find an appropriate middle ground that can address the problem.
References
Augustsson, H., Churruca, K. and Braithwaite, J. 2020. Change and improvement 50 years in the making: a scoping review of the use of soft systems methodology in healthcare. BMC Health Services Research, 20, pp.1-13.
Australian Institute of Health and Welfare. 2020. Interfaces between the aged care and health systems in Australia— movements between aged care and hospital 2016–17. https://www.aihw.gov.au/reports/aged-care/movements-between-aged-care-and-hospital/contents/summary
Australian Public Health Commission. 2007. Tackling wicked problems : A public policy perspective. https://www.enablingchange.com.au/wickedproblems.pdf
Chapman, J. 2004. System failure: Why governments must learn to think differently, United Kingdom, Demos.
Checkland, P. and Scholes, J. 1999. Soft systems methodology in action. John Wiley & Sons.
Chen, H., Walabyeki, J., Johnson, M., Boland, E., Seymour, J. and Macleod, U. 2019. An integrated understanding of the complex drivers of emergency presentations and admissions in cancer patients: qualitative modelling of secondary-care health professionals’ experiences and views. PLoS One, 14(5), p.e0216430. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6497383/
Frood, S., Johnston, L. M., Matteson, C. L. and Finegood, D. T. 2013. Obesity, complexity, and the role of the health system. Current Obesity Reports, 2, pp.320-326.
Goto, Y. and Miura, H. 2022. Using the soft systems methodology to link healthcare and long-term care delivery systems: A case study of community policy coordinator activities in Japan. International Journal of Environmental Research and Public Health, 19(14), p.8462. https://pubmed.ncbi.nlm.nih.gov/35886316/
Head, B. W. 2014. Evidence, Uncertainty, and Wicked Problems in Climate Change Decision Making in Australia. Environment and Planning C: Government and Policy, 32, 663-679.
Henderson, C. & Gronholm, P. C. 2018. Mental Health Related Stigma as a ‘Wicked Problem’: The Need to Address Stigma and Consider the Consequences. Int J Environ Res Public Health, 15.
Hobbs, C. and Midgley, G. 2020. How systems thinking enhances systems leadership. https://i2insights.org/2021/04/13/systems-thinking-and-leadership/
Kim, D. 2011. Guidelines for Drawing Causal Loop Diagrams. The Systems Thinker 22. https://thesystemsthinker.com/guidelines-for-drawing-causal-loop-diagrams-2/
Linnéusson, G., Andersson, T., Kjellsdotter, A. and Holmén, M. 2022. Using systems thinking to increase understanding of the innovation system of healthcare organisations. Journal of Health Organization and Management, 36(9), pp.179-195.
Meadows, D. 2008. Thinking in Systems: A Primer, London, UK, Earthscan.
Norman-Major, K. 2018. Thinking Outside the Box: Using Multisector Approaches to Address the Wicked Problem of Homelessness Among LGBTQ Youth. Public Integrity, 20, 546-557.
Periyakoil, V. S. 2007. Taming wicked problems in modern health care systems. J Palliat Med, 10, 658-9.
Rittle, H. W. J. & Webber, M. M. 1973. Dilemmas in a general theory of planning. Policy Sciences, 4, 155-169.
Rozario, D. 2019. Burnout, resilience and moral injury: How the wicked problems of health care defy solutions, yet require innovative strategies in the modern era. Can J Surg, 62, E6-e8.
Rusoja, E., Haynie, D., Sievers, J., Mustafee, N., Nelson, F., Reynolds, M., Sarriot, E., Swanson, R.C. and Williams, B. 2018. Thinking about complexity in health: a systematic review of the key systems thinking and complexity ideas in health. Journal of Evaluation in Clinical Practice, 24(3), pp.600-606.
Samuriwo, R. & Hannigan, B. 2020. Wounds in mental health care: The archetype of a ‘wicked problem of many hands’ that needs to be addressed? International Journal of Mental Health, 49, 81-96.
Senge, P., Hamilton, H. and Kania, J. 2015. The dawn of system leadership. Stanford Social Innovation Review, 13(1), pp.27-33.
Trbovich, P. 2014. Five ways to incorporate systems thinking into healthcare organizations. Biomedical Instrumentation & Technology, 48, 31-36.
Wiig, S., Robert, G., Anderson, J.E., Pietikainen, E., Reiman, T., Macchi, L. and Aase, K. 2014. Applying different quality and safety models in healthcare improvement work: boundary objects and system thinking. Reliability Engineering & System Safety, 125, pp.134-144.
Williams, B. and Hummelbrunner, R. 2010. Systems concepts in action: A practitioner’s toolkit. Stanford University Press.

