4 Improving the Participation Gap: Physiotherapy for People Experiencing Long COVID
Improving the Participation Gap: Physiotherapy for People Experiencing Long COVID
By Kate Woodhead, Rita Kinsella, Karen Borschmann, Anne Holland, Janet Bondarenko & Danielle Hitch.
If this is your first visit to the textbook, please take a moment to read the About This Book chapter to get the most out of your experience.
You may find some material in multiple chapters (such as an introduction to common symptoms of Long COVID) because we anticipate some readers will only access certain chapters. Please feel free to skip any material you are already familiar with.
Learning objectives
After reading this chapter and completing the learning activities, you will be able to:
- Recognise the common symptoms of Long COVID
- Describe the assessment methods used in the management of Long COVID
- Demonstrate relevant assessment skills required to assist in the management of Long COVID
- Apply evidence-based exercise rehabilitation principles to design a program for patients presenting with Long COVID
- Plan a strategy for the self-management of a patient experiencing Long COVID
Introduction
The longer-term impacts of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) or more commonly referred to as COVID-19 infection have been described in the literature using varying terms, including “Long COVID”, “Long COVID-19”, “long-haul COVID”, “Post-Acute COVID-19″, “Post-COVID Conditions” and “Post-Acute Sequalae of SARS-CoV-2 infection (PASC)”[1][2]. The term Long COVID was first coined as a hashtag by a patient in Italy early in the pandemic[3] and is now widely recognised in the media, by patients, and in scientific literature[4].
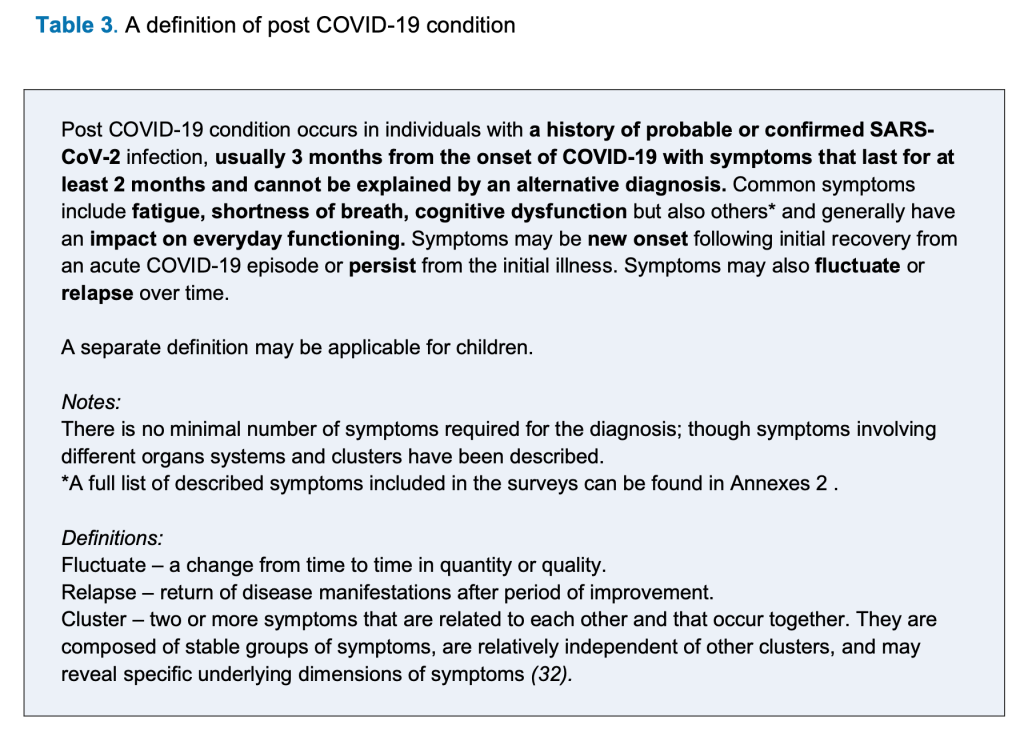
In an Australian context, the Parliamentary enquiry into Long COVID (2023) recommended that at this time the World Health Organization’s (WHO) definition of Long COVID be used clinically[5].
For more information regarding the various definitions existing internationally please visit Chapter 1. What is Long COVID?
As the evidence continues to emerge regarding Long COVID, our understanding of the condition and the impact it has on patients affected by it continues to grow[6][7]. With more than 760 million people having been diagnosed with COVID-19 worldwide since the beginning of the pandemic[8], it stands to reason that we will continue to see an increasing number of people presenting to physiotherapy with symptoms and impairments that may be attributable to Long COVID either as a primary problem or a concurrent associated problem. As physiotherapists, regardless of our area of practice, it is vital we have an understanding of and awareness of Long COVID. This should include how to assess for, treat and manage the presenting impairments and/or limitations on activity participation of people experiencing Long COVID.
Whilst evidence continues to develop regarding the likely duration of the ongoing effects of an acute COVID-19 infection[9][10][11], anecdotal and newer evidence suggests that some patients with impairments attributable to Long COVID improve over time[12][13]. The specific timeline for recovery and symptoms experienced is however unique to each individual[14].
The learning objectives included in this chapter were drawn from the results of a national Australian survey of 104 physiotherapists and physiotherapy students. A Pat Cosh Trust grant (administered by the Australian Physiotherapy Association) has enabled the development of this interactive chapter to support the optimal management of patients presenting with impairments who are recovering after COVID-19 infection: click here for more information about the development of the chapter. The content of the chapter has been drawn from international and national guidelines and peer-reviewed journal publications.
This chapter will cover the following topics:
|
The content has been peer-reviewed and will be updated periodically as new evidence related to the physiotherapy management of Long COVID emerges.
Impairments that may benefit from physiotherapy management
Long COVID is frequently described in the literature as being “multi-dimensional, episodic and unpredictable”[15]. Presenting symptoms can vary widely from patient to patient[16][17]. Patients can present with overlapping or clustered symptoms, which may change or fluctuate over time[18]. Physiotherapists assist patients to improve their quality of life[19] and it has been well documented that the symptoms of Long COVID can have a significant detrimental impact on health and wellbeing[20]. As a result of the wide range of symptoms that may be present, patients with Long COVID may experience varying degrees of impairment that can impact physical, cognitive, mental and emotional health, all of which may impact on their activities of daily living and participation in education and exercise[21].
There is no one test to diagnose Long COVID, rather it is considered a diagnosis of exclusion[22]. It is also important to consider that presenting symptoms may be due to other factors such as underlying or pre-existing health conditions, complications from acute COVID-19 infection (such as DVT or PE), physical deconditioning that may have occurred after a long or complicated acute illness (such as post-intensive care syndrome), or even re-infection of COVID-19[23][24]. As primary contact practitioners, physiotherapists should liaise with other members of the multidisciplinary team to further assist with refining medical diagnosis and differential diagnosis. Care should be adjusted as the team develops a greater understanding of the patient’s presenting clinical signs and symptoms and their response to therapy deepens.
Also, health professionals who possess an understanding of the common presenting symptoms may assist patients with Long COVID to allay any associated fear or frustration that they may experience when interacting with the health system[25][26]. The fears or frustrations that may be expressed by patients with Long COVID include but are not limited to[27]:
- Feeling let down or abandoned by healthcare services
- Feeling forgotten
- Not feeling listened to
- Feeling like symptoms are not believed or dismissed
- Frustration related to symptoms being attributed to other issues such as anxiety
“It has been an awful time and it made it worse when I felt that I wasn’t being believed about the symptoms. They put it down to anxiety disorder.”
(Male, Age unknown)[28]
These fears and frustrations may be reinforced by health professionals, family, friends and employers. Taking time to listen and validate a patient’s experience is an important part of the overall management of patients with Long COVID[29][30].
Common symptoms
Symptoms of Long COVID can affect all body systems. SARS-CoV-2 enters the body via the angiotensin-converting enzyme 2 (ACE-2) receptor[31]. These receptors are located on cells throughout the body, giving the virus the capacity to infect and damage cells within multiple organs, which is reflected in the large variety and differing of symptoms that people with Long COVID may experience[32][33].
For further information related more broadly to Long COVID and the symptoms, please visit Chapter 1. What is Long COVID?
Common symptoms of Long COVID[34][35] that people presenting to physiotherapy may report include, but are not limited to:
A systematic review of studies including over 47,000 patients has identified the three most common symptoms experienced by people with Long COVID as being fatigue, cognitive and concentration impairment and shortness of breath[36][37][38][39].
Further to this, a 2022 meta-analysis[40] including over 1.2 million patients from 22 countries reported on the prevalence of three common Long COVID symptom clusters with these being respiratory symptoms (described as ongoing respiratory problems), fatigue symptoms (described as persistent fatigue with bodily pain or mood swings) and cognitive symptoms (and related cognitive problems).
Key message
Long COVID is a “diagnosis of exclusion”[41]. It is important to consider all presenting symptoms and impairments and the potential or likely underlying cause of these.
The role of the physiotherapist is to assess for and manage the symptoms and impairments, regardless of a formal diagnosis of Long COVID. As primary contact practitioners, physiotherapists may also assist the multidisciplinary team in refining the diagnosis of Long COVID or the diagnosis of other non-Long COVID conditions.
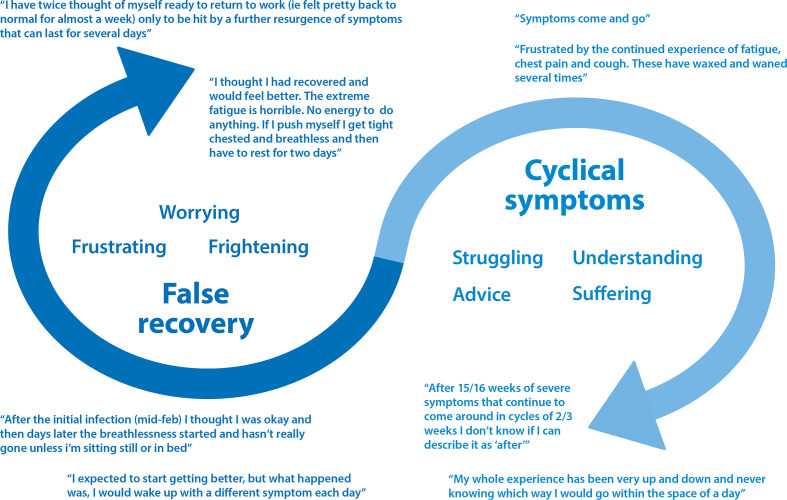
Episodic nature of Long COVID
Symptoms not only vary, but may also fluctuate and people with Long COVID can experience ‘false recovery’[42]. The uncertainty and unpredictability of the future for patients with Long COVID can be a significant source of distress and may manifest in newly diagnosed or exacerbation of pre-existing psychological problems, particularly anxiety[43].
Buttery S, Philip KEJ, Williams P, Fallas A, West B, Cumella A, Cheung C, Walker S, Quint JK, Polkey MI, Hopkinson NS. Patient symptoms and experience following COVID-19: results from a UK-wide survey. BMJ Open Respir Res. 2021 Nov;8(1):e001075. doi: 10.1136/bmjresp-2021-001075. © 2021 by the authors. This is an open-access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
Referrals to other health professionals
Due to the wide variety of possible symptoms and impairments, multiple health professionals or teams may be required to assist in the ongoing management of patients experiencing Long COVID, particularly when symptoms are not related to respiratory or physical function[44]. Best practice management for patients with Long COVID would involve a multidisciplinary team either in a community setting or through Long COVID clinics[45].
Long COVID Multidisciplinary Team.
Photo by Kampus Productions from Pexels.
Learning activity (10 mins)
Complete the following multiple-choice quiz. Check your answer by clicking the blue ‘Check’ box below before clicking the arrow across to go to the next question.

Read the ‘COVID-19’ section of the persona of Jarrod and consider the questions below:
Do you feel Jarrod would require referral to other services?
Which other services might you refer Jarrod to?
Assessment and the use of outcome measures are important to help determine whether a specific physiotherapy intervention is appropriate and its effectiveness, once implemented, as part of the overall management of the patient. Currently there are no tests or tools that have been recommended to confirm the diagnosis of Long COVID[46][47][48]. Patients with concerning red flags, particularly if sinister pathology is suspected, should be referred onwards in a timely fashion. The goal of the patient interview should be to identify the severity of any symptoms and the impact these have on the quality of life and daily activities for the individual[49]. Various screening and assessment tools may be used to assist in this process. In addition, a symptom-based objective assessment should be undertaken where indicated, noting that once again there is no "one size fits all" set of outcome measure or tests for people experiencing Long COVID due to the wide and varying symptoms and their severity[50].
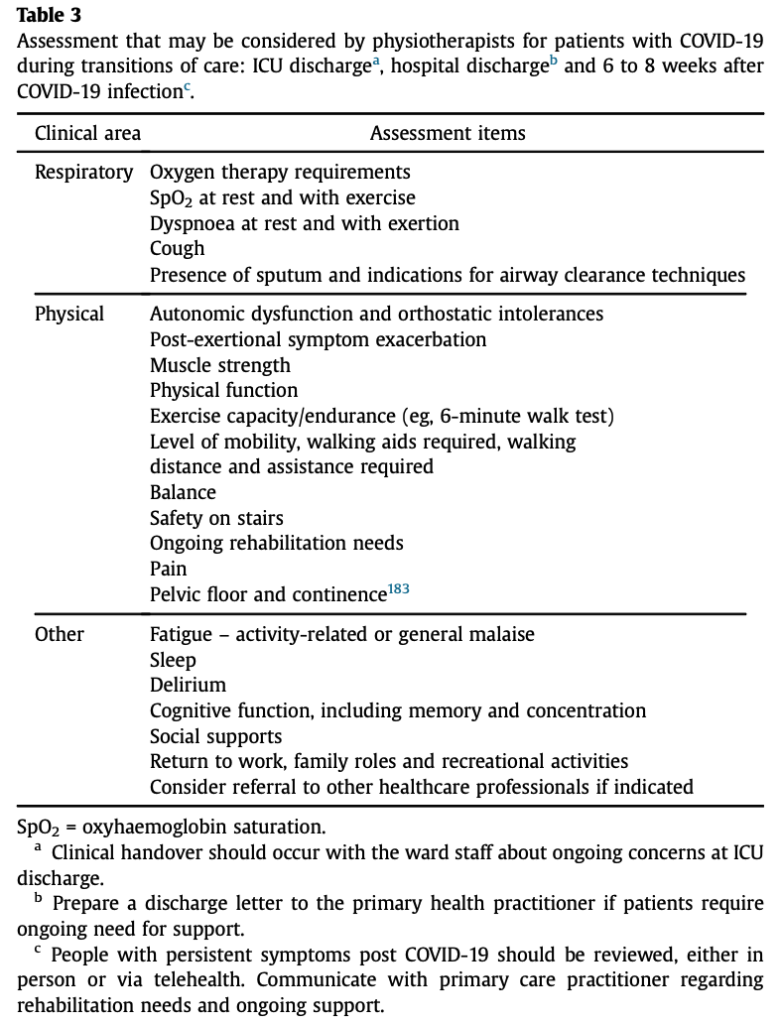
It has been suggested that physiotherapists should screen patients at various time points across the continuum of care (whether they were initially managed in hospital or the community) [51] so that patients with Long COVID may be identified early and referred for appropriate and timely follow-up.
General assessment
General assessment may include the following:
Important - Desaturation
A drop in pulse oximetry saturation of greater than 3-4% from baseline measurement or to 94% or below during exercise testing is considered desaturation[52][53] and may warrant further investigation. This will be determined by the physiotherapist on a case-by-case basis.
There are few Long COVID specific outcome measures and the use of patient-reported outcome measures developed for other conditions may not be applicable or relevant when applied to those with Long COVID[54]. There is a clear need for Long COVID specific tools to be developed and tested. The following tools are currently being used in Long COVID research or within Australian Long COVID clinics.
General screening tools
Cardiorespiratory screening tools
Modified Medical Research Council (mMRC) Dyspnoea Scale
(Brompton) Breathing Pattern Assessment Tool (BPAT)
Nijmegen questionnaire
Functional and exercise capacity tests
It is important to note, when considering functional or exercise capacity tests, that physical exertion may significantly exacerbate symptoms in some people experiencing Long COVID. Clinical judgement should be used as these tests may not be suitable for all but may offer a useful baseline measure[55].
1-minute Sit-To-Stand Test (1STST)
2-Minute Walk Test (2MWT)
Timed Up and Go Test (TUG)
10-Meter Walk Test (10MWT)
6-Minute Walk Test (6MWT)
Cardiopulmonary Exercise Test (CPET)
Tinetti Gait and Balance Assessment Tool
Quality of life
Psychosocial
Generalised Anxiety Disorder-7 (GAD-7)
Depression Anxiety and Stress Scale (DASS-21)
Hospital Anxiety and Depression Scale (HADS)
Other
DePaul Post-Exertional Malaise Questionnaire
Fatigue Scale for Motor and Cognitive Functions
Functional Assessment of Chronic Illness Therapy – Fatigue Scale (FACIT-F)
Brief Questionnaire to Screen for Post-Exertional Symptom Exacerbation (PESE)
Putting it all together
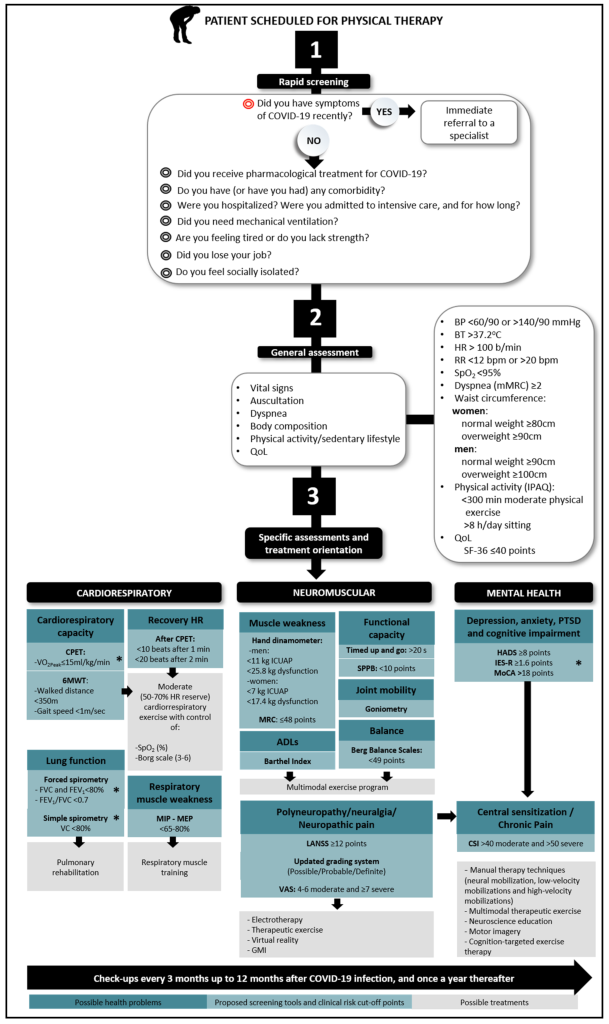
A proposed surveillance model for use by physiotherapists is presented in the figure below and includes three distinct and scaffolded sections to ensure a comprehensive assessment: a rapid screening, a general assessment and specific assessments that recommend various tools and parameters to aid treatment and management planning[56]. Rapid screening is designed to initially exclude new acute infection with SARS-CoV-2, noting that people experiencing Long COVID may otherwise answer yes to this question as they may be experiencing symptoms attributable to COVID-19, but this will not necessarily require onwards referral. It is important that the line of questioning within this section also details the patient's symptoms and how these symptoms behave over time. Most importantly, there must be a clear discussion around the goals of physiotherapy treatment. In regard to general assessment in an outpatient setting, auscultation is unlikely to provide any additional information to the patient's overall picture and thus is generally not necessary to perform. Finally, referral to a pulmonary rehabilitation program is typically based on symptoms and functional limitations rather than solely based on impaired spirometry findings. The suggested treatments shown in the grey shaded boxes are just that - suggestions.
Learning activity (20 mins)
Considering the persona of Jarrod, outline your assessment plan.
Which screening tools might you use for Jarrod and why?
Exercise-based rehabilitation for Long COVID
Physiotherapy and exercise-based rehabilitation are traditionally considered fundamental to recovery following illness[57]. However, the evidence to guide best practice physiotherapy management in people experiencing Long COVID remains unclear[58][59][60].
Physiotherapists, with their known expertise in movement, function, and rehabilitation [61], play a vital role in helping individuals regain physical function, alleviate symptoms, and improve their overall quality of life[62]. People experiencing Long COVID who have a reduced physical capacity and associated symptoms should be considered for referral to exercise-based rehabilitation[63].
Exercise-based rehabilitation for Long COVID should encompass a tailored program of physical activity that addresses the unique needs and limitations of each individual[64][65][66][67]. Rehabilitation programs may include a combination of education[68] (including pacing, pain management, self-management among others), aerobic and resistance training[69][70][71][72].
Physiotherapists play an important role in ensuring the safety and effectiveness of the exercise program, as well as making appropriate modifications based on the individual symptomatology and progress of the patient[73].
Precautions and contraindications to exercise; an overview
Precautions and contraindications to exercise-based rehabilitation in Long COVID should be considered to ensure the safety and well-being of individuals. While exercise is considered to be generally beneficial, people living with Long COVID may experience symptom exacerbation (i.e., if Post Exertional Symptom Exacerbation or PESE is present) or reduction in their current levels of participation if the unique characteristics of Long COVID are not considered[74].
Important - RED flags for rehabilitation
As per the WHO guidelines[75], assessment, further investigation and management of patients with complications related to their COVID-19 acute infection, including significant cardiac impairment (which may present as: chest pain, palpitations or an altered resting heart rate >100bpm[76]), or respiratory desaturation below recommended parameters (<94%), is strongly recommended prior to the commencement of a rehabilitation program to rule out potentially life-threatening complications.
Whilst there is not a set list of tests or investigations for red flags, thorough assessment and an understanding of the person experiencing Long COVID symptoms and their patterns will assist in minimising risk when commencing exercise-based rehabilitation.
Contraindications
Precautions
Symptom monitoring
People with Long COVID may experience fluctuating symptoms resembling those found in other post-viral syndromes such as Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS)[79].
Symptoms and response to exercise should be monitored closely during, immediately after and in the days following exercise therapy[80][81]. A symptom or activity diary may be a useful tool to assist in this process - click here for a downloadable diary template.
If, despite the use of pacing/gradual progression/loading, the exercise consistently exacerbates symptoms and results in prolonged worsening of overall health and wellbeing, it may be necessary to reassess the exercise program and consider alternative approaches.
Exertional oxygen desaturation and breathlessness
Physical activity increases oxygen demand, and when significant exertional oxygen desaturation is present, commencing exercise-based rehabilitation should be undertaken with caution. Whilst rare, some patients may develop long-term cardiac and pulmonary complications after an acute COVID-19 infection[82] which may inhibit their ability to participate in exercise. Referral to a Pulmonary Rehabilitation program and/or a Respiratory Physiotherapist should be considered for patients presenting with symptoms of Post-COVID lung disease as, in these cases, it may not be possible to prevent exertional desaturation.
Symptom titrated physical activity[83] may be considered within a rehabilitation program where exertional oxygen desaturation is present[84].
Breathing Pattern Disorders (BPD) including hyperventilation syndrome may be present for some people experiencing Long COVID even if no exertional desaturation is present[85]. Additionally, many patients may experience breathlessness without desaturation and no evidence of breathing pattern disorders. Breathlessness may result due to prolonged reduced participation and resultant deconditioning. Exercise-based rehabilitation aims to teach people experiencing breathlessness that these sensations are normal, and to give them tools and strategies to assist in self-management.
During exercise rehabilitation sessions, oxygen saturation and dyspnoea symptoms should be monitored throughout using established criteria and outcome measures[86][87].
Important - When to reduce exercise intensity
The criteria for reduction in intensity and/or ceasing exercise[88][89]:
- A drop in SpO2 of > 3-4% from baseline measurement[90]
- SpO2 < 90%
- Modified Borg Dyspnoea Scale ≥ 6
- Shortness of breath with no relief after rest
- Chest pain or tightness
- Dizziness
- Headache
- Blurred vision
- Palpitation
- Tachycardia
- Syncope
Heart rate and exercise
Cardiac impairment following COVID-19 infection has been well documented in the literature[91][92][93][94]. Exercise restrictions are recommended in the presence of acute cardiac conditions (e.g., acute myocarditis) because exercise can increase the risk of mortality and morbidity[95].
There is a potential for the delayed development of cardiac dysfunction in people experiencing Long COVID[96]. Any changes to cardiac signs and symptoms during or after exercise warrants further clinical assessment and/or investigation[97][98].
Important - Signs / symptoms of suspected cardiac impairment [99][100]
- Chest pain
- Difficulty breathing
- High resting or exertional heart rate
- Increased respiratory rate
- Reduced oxygen saturation
- Palpitations
- Reduced exercise tolerance
There is currently no consensus on recommended heart rate parameters for exercise-based rehabilitation in patients living with Long COVID.
Key message
It is important for individuals experiencing Long COVID to work closely with their healthcare team, to determine appropriate exercise guidelines and make necessary adjustments based on their individual circumstances and symptomatology.
Exercise-based rehabilitation should be a slow and careful process respecting patient symptoms and response to the exercise program.
Post-Exertional Symptom Exacerbation (PESE)
PESE is a phenomenon characterized by the triggering or worsening of symptoms following minimal physical, emotional, social or cognitive exertion[101][102]. Symptoms may worsen 12 to 72 hours following activity and may last for days or weeks[103][104]. The severity and duration of PESE can vary widely among individuals. PESE has been associated with other disabling conditions such as Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS)[105]. One international study that surveyed people seven months after a suspected or confirmed COVID-19 infection, found that 89.1% of the respondents reported either physical or mental post-exertional fatigue malaise[106].
“If I don’t get this right, I will crash as soon as I get back to work…”
(Jarrod, 42year old)
PESE can manifest as increased fatigue, exercise intolerance, pain, cognitive dysfunction or ‘brain fog’, sleep disturbances or general malaise[107]. Patients with PESE may report a reduced capacity to work or study, alongside negative effects on physical functioning, exercise tolerance and social activity[108]. Patients may often describe experiencing a ‘crash’ after activity if symptom exacerbation is experienced over a longer timeframe[109].
Symptom stabilisation should be the initial aim[110][111].
Important - Graded exercise
Graded exercise approaches and fixed activity prescription should not be used in patients experiencing PESE[112][113]. Activity and exercise prescription should instead be titrated to the individual’s symptoms. The “Stop. Rest. Pace” activity management message along with heart rate monitoring may assist patients with PESE to self-manage with the support of their healthcare provider/s[114].
Pacing and activity management
Pacing involves employing a range of strategies to avoid both over- and under-exertion, rather than being a form of avoidance behaviour[115][116]. Evidence for the use of pacing and activity modification as a self-management strategy in people experiencing Long COVID and PESE is limited[117][118].
Important - Pacing theories
The spoon theory
The Spoon Theory illustrates the limited energy reserves individuals with chronic conditions possess by using spoons as a metaphorical representation of units of energy. Each activity throughout the day "costs" a certain number of spoons, depleting the available energy pool. Once spoons have been used, the person is more likely to experience fatigue or symptom exacerbation. Managing daily tasks becomes a matter of rationing and carefully prioritising spoon expenditure to prevent overexertion and maintain the ability to participate in activities. This theory was developed by people with chronic disease and disability as a way of describing their experience.
For further information, visit 'The Spoon Theory' written by Christine Miserandino. Christine lives with lupus, and the theory is based on her lived experience of managing this condition.
The energy envelope theory[119]
This theory proposes that individuals with limited energy resources can manage their well-being by recognising their perceived energy limits. By pacing activities, avoiding overexertion, and balancing rest, they aim to stay within their 'energy envelope'. This in turn aims to minimise symptoms and enhance overall functioning.
For further information, visit 'Finding your Envelope' by Bruce Campbell
Pacing strategies may include[120][121]:
Heart Rate (HR) monitoring
In ME/CFS HR during exercise is encouraged to be kept within the 'energy envelope' (i.e., below the anaerobic threshold), as breaching this threshold may trigger PESE)[122]. This may be relevant for those individuals with Long COVID and PESE. HR monitoring can be used to guide working within one’s 'energy envelope', thus ensuring that overall energy expenditure is less likely to result in PESE.
Useful guides to calculate appropriate resting HR and HR that indicates the anaerobic threshold can be found here;
| Emerge Australia |
| Workwell Foundation |
| Physio For Me |
Education and supported self-management
Education regarding self-management strategies is important for patients experiencing PESE[123]. Physiotherapists should support self-care strategies and adaptive coping mechanisms by providing information and resources about PESE. This is an important part of the management as appropriate education empowers individuals to self-monitor and make informed decisions about their ongoing care, health and well-being.
Autonomic dysfunction
Autonomic dysfunction, also known as Autonomic Nervous System (ANS) dysfunction or dysautonomia, refers to disruption or impairment in the normal functioning of the ANS[124]. The ANS is responsible for regulating and controlling involuntary bodily functions, such as heart rate, blood pressure, gastrointestinal motility, respiratory rate and temperature regulation[125][126][127]. It consists of two main branches: the sympathetic nervous system and the parasympathetic nervous system.
When autonomic dysfunction occurs, it can disrupt the balance between these two branches, leading to a range of symptoms and issues. Due to the ANS role in regulating blood flow and therefore oxygen delivery to muscles, individuals with autonomic dysfunction might experience fatigue and exercise intolerance, along with other symptoms such as breathlessness, chest pain, palpitations and presyncope[128].
Autonomic dysfunction encapsulates a broader spectrum of dysregulation within the ANS, affecting various physiological functions[129].
Key message - Autonomic dysfunction
If you suspect either yourself or someone you know is experiencing autonomic dysfunction, it's important to consult a medical professional for an accurate diagnosis and management plan.
Orthostatic intolerance
Orthostatic intolerance occurs due to an abnormal autonomic response to postural change[130]. Patients can present with either resting or postural hypotension and/or tachycardia[131][132]. The term orthostatic intolerance may be used when objective tests have been unable to confirm a diagnosis of the common autonomic disorders[133].
Postural Orthostatic Tachycardia Syndrome (POTS)
POTS is considered a disorder of the ANS that is associated with tachycardia upon standing[134].
It is clinically defined as[135][136]:
- a HR increase of ≥ 30 bpm within 10 minutes of standing up without significant hypotension or
- HR >120 bpm for 10 minutes on standing without significant hypotension
Self-management and exercise
Whilst limited evidence exists to manage autonomic dysfunction for people living with Long COVID, education and exercise have been recommended as part of the management[137][138].
Education should include identification of symptom aggravating and easing factors, as well as including instruction on counterpressure maneuverers such as crossing the legs while standing[139]. Other education for self-management includes (but is not limited to):[140]
Autonomic Conditioning Therapy (ACT)
Autonomic conditioning therapy or ACT is one rehabilitation protocol that has been shown to improve fatigue in people experiencing Long COVID[141].
ACT involves participation in a supervised, gradual, symptom-oriented exercise program consisting of three phases of rehabilitation[142]:
| PHASE 1
Phase 1A: Supine active ROM exercises (over minimum of 2 weeks) Performed bilaterally over 30second intervals at an RPE 2/10 on modified Borg scale Phase 1B: Upright exercise 2x sets of 10 reps each exercise, plank 2x 10sec holds |
| PHASE 2
Phase 2A: Progressive submaximal aerobic exercises (over 4 weeks) Week 1: 5x 1 minute intervals progressing to Week 4: 5x 90second intervals Phase 2B: Continue progression of submaximal aerobic training (over 4 weeks) Week 1: 3x 2minute intervals progressing to Week 4: 6x 2minute intervals |
| PHASE 3
Phase 3/ Levine protocol: Progressive and graded aerobic exercise program (over 6 weeks) Base pace = 75% age predicted maximum HR and RPE of 13-16 |
Importantly, patients participating in an ACT program should be progressively guided through the phases according to their individual symptom responses to the program[144]. Additionally, patients should be closely monitored for PESE throughout the rehabilitation program.
Key messages
- Exercise-based rehabilitation for those experiencing Long COVID should:
- be personalised
- manage expectations
- be psychologically supportive
- avoid symptom exacerbation - Exercise-based rehabilitation should focus on symptom stabilisation in the first instance, as well as strategies to sustain patient function without exacerbating symptoms[145].
- Physiotherapists can guide the rehabilitation pathway of those experiencing Long COVID, by providing carefully designed programs tailored to the individual, that balance activity with adequate rest[146].
- Consistent symptom monitoring is a vital component of exercise-based rehabilitation for patients experiencing Long COVID and should be incorporated before, during and after any exercise or physical activity.
Learning activity (30 mins)
Read the persona of Jarrod.

Jarrod’s goals (in no particular order) are to:
- Return to work as a painter and decorator or in a related job.
- Feel less pain and stiffness in his body.
- Get back to completing all his activities for himself and no longer rely on others.
- Spend more time with his kids, including looking after them on his own.
- Get back into regularly riding, running and hiking to reconnect with nature.
1. Considering Jarrod and his description of symptoms, what are the key safety concerns to consider when prescribing an exercise program for him?
Use the padlet to record your answers. Remember that this is a public board, and please do not include any identifying information. This padlet is best viewed in full-screen mode.
Read the following open-access article - Muscle abnormalities worsen after post-exertional malaise in long COVID by Appelman et al.
2. Write an outline for an exercise program for Jarrod taking into account his goals, symptoms and the potential underlying pathophysiology of his condition. Include how you might modify exercises for him given his presenting symptoms, how exercise may be progressed according to his symptoms and what factors might indicate a need to cease the exercise-based rehabilitation program.
Other physiotherapy treatment/s for Long COVID
In general terms, established symptom management approaches are recommended for people with Long COVID, and as such, physiotherapists should consult existing clinical guidelines to guide their management[147].
Fatigue
Fatigue or exhaustion is commonly reported in those with Long COVID and may be a major barrier to participation to undertaking everyday tasks.
Pacing and energy conservation techniques may be useful tools for those with Long COVID, who experience fatigue.
Symptom titrated physical activity means engaging in physical activities, that may include exercise, only at a level guided by the presence and severity of symptoms, to mitigate exacerbating symptoms.
It is important to exclude the presence of PESE before commencing exercise-based rehabilitation[148].
For further information related to fatigue and its management please refer to the previous section on PESE.
Pain management
Patients with Long COVID may experience arthralgia which presents as inflammatory type pain in one or more joints, commonly the knees, ankles and/or wrists[149] as well as myalgia. Musculoskeletal pain as a symptom of Long COVID can be extremely debilitating and have a significant impact on function[150].
There is currently no evidence supporting specific interventions to manage pain in patients with Long COVID. The WHO[151] recommends pain education, self-management strategies and physical exercise training (in the absence of PESE) to manage arthralgia, i.e., treatment should be as per standard practice.
If chronic/persistent pain is present, or suspected to develop, referral to a Chronic Pain Clinic should be considered.
Breathing Pattern Disorders (BPD)
Breathing Pattern Disorders (BPD), also known as breathing impairment or Dysfunctional Breathing (DB) can be defined as dyspnoea associated with an abnormal pattern of breathing in the absence of significant cardiopulmonary disease or dyspnoea that is out of proportion to an underlying cause[152]. BPD (including hyperventilation and dysfunctional breathing) are common in autonomic dysfunction and POTS.
BPD may be present at rest or during physical activity including activities of daily living and exercise[153][154]. Hyperventilation Syndrome and Periodic Deep Sighing have been described as the more common presentations of BPD in patients with Long COVID[155].
The main physiotherapy intervention for patients experiencing BPD is breathing re-training, focusing on establishing a nose/diaphragm pattern of breathing and reducing overall ventilation.
Referral to a specialist respiratory physiotherapist should be considered, in order to optimise management of BPD.
Learning activity (10 mins)
Read the persona of Jarrod.
What additional physiotherapy treatment options (other than exercise) may be appropriate for Jarrod given his ongoing symptoms?
Are referrals to other health care providers required at this time for Jarrod?
Self-management for Long COVID
It is recommended that self-management for Long COVID be incorporated into the recovery plan[156].
Self-management for Long COVID is a broad topic that is currently not covered in detail in this chapter. Information to include or provide those with Long COVID include, but are not limited to:
- Physical activity and returning to exercise
- Management of more common presenting symptoms such as breathlessness or persistent pain
- Management of activities of daily living including general advice related to pacing and energy conservation
- Returning to work or study
- General advice related to nutrition and sleep hygiene
- Links to resources to support psychological wellbeing
The NHS Your COVID Recovery website is an example of best practice for supporting self-management of those presenting with milder impairments attributable to Long COVID[157].
Conclusion
Physiotherapy plays an important role in optimising the recovery of patients with Long COVID. It is important that clinicians regularly reassess the patient's symptoms, their functional progress, and adherence to the recommended self-management strategies. Modification and adjustment of interventions may be required based on each individual's response to increasing their physical activity and/or exercise load.
It cannot be emphasised enough the importance of individualised management for patients with Long COVID. There is no "one-size fits all" approach to addressing the presenting impairments that may be observed in clinical practice. Working collaboratively with the wider multi-disciplinary healthcare team will result in optimal outcomes for each patient.
Whilst the information contained in this chapter is by no means exhaustive, it is designed to provide an overview and highlight key information for physiotherapists working with people diagnosed with Long COVID. Further reading and resources that may be beneficial for both patients and their families as well as health professionals are provided in the links below.
Further information
The following links will provide you with additional information about Long COVID from credible sources. These listings are not exhaustive, and you are encouraged to seek out locally relevant information.
General resources for people with Long COVID and their families
- Long COVID Physio - Website
- NHS - Your COVID Recovery - I have or may have long COVID
- Royal Australian College for General Practitioners (RACGP) - Patient resource: Managing post-COVID-19 symptoms
- Peer support groups
Long COVID Support Australia
Lung Foundation Australia - COVID recovery support group - Provincial Health Services Authority (PHSA) - Post-COVID-19 Interdisciplinary Clinical Care Network Resources - Living with Post-COVID symptoms (website)
- Scottish Intercollegiate Guidelines Network (SIGN) - Long COVID; A booklet for people who have signs and symptoms that continue or develop after acute COVID-19
- World Health Organization (WHO)Support for rehabilitation: self-management after COVID-19-related illness
Post-COVID-19 Condition (factsheet)
Resources for specific symptoms of Long COVID
- Breathing Pattern Disorders
Would you like to breathe better?
Breathing dysfunction
- Breathlessness
Asthma and Lung UK - Autonomic dysfunction
Dysautonomia International - Long COVID and ME/CFS
Long COVID and ME/CFS are they the same condition? - Post Exertional Symptom Exacerbation (PESE)
Advice on energy and symptom management:
NICE guideline: Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management
Activity and energy management - pacing
Emerge Australia Website: Post-Exertional Malaise (PEM) - Postural Orthostatic Tachycardia Syndrome (POTS)
PoTS UK
Health care professional resources
-
Australian Parliamentary Inquiry into Long COVID
Sick and tired: Casting a long shadow. Inquiry into Long COVID and Repeated COVID Infections.
- National Clinical Evidence Taskforce
Australian guidelines for the clinical care of people with COVID-19
Care of people after COVID-19 (flowchart) - National Institute for Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN) and Royal College of
General Practitioners (RCGP)COVID-19 rapid guideline: managing the long-term effects of COVID-19 - The Lancet
COVID-19 Resource Centre - Long COVID Physio
Resources
Podcast episodes - Royal Australian College for General Practitioners (RACGP)
Caring for patients with pos-COVID-19 conditions - World Health Organization (WHO)
Clinical management of COVID-19: living guideline
Post COVID-19 condition
References
- Centers for Disease Control and Prevention. (2022, December 16). Post-COVID Conditions: Information for Healthcare Providers. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html ↵
- Lopez-Leon, S., Wegman-Ostrosky, T., Perelman, C., Sepulveda, R., Rebolledo, P. A., Cuapio, A., & Villapol, S. (2021). More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Scientific Reports 11, Article 16144. https://doi.org/10.1038/s41598-021-95565-8 ↵
- Callard, F. & Perego, E. (2021). How and why patients made Long Covid. Social Science Medicine 238, 113426. https://doi.org/10.1016/j.socscimed.2020.113426 ↵
- Crook, H., Raza, S., Nowell, J., Young, M., & Edison, P. (2021). Long covid – mechanisms, risk factors, and management. BMJ (Clinical research ed.), 374, n1648. https://doi.org/10.1136/bmj.n1648 ↵
- House of Representatives Standing Committee on Health, Aged Care and Sport (2023). Sick and tired: Casting a long shadow. Inquiry into Long COVID and Repeated COVID Infections. Parliament of Australia. Canberra. Available at: https://parlinfo.aph.gov.au/parlInfo/download/committees/reportrep/RB000006/toc_pdf/SickandtiredCastingalongshadow.pdf ↵
- Centers for Disease Control and Prevention. (2022, December 16). Long COVID or Post-COVID Conditions. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html ↵
- Thomas, P., Baldwin, C., Beach, L., Bissett, B., Boden, I., Cruz, S. M., Gosselink, R., Granger C. L., Hodgson, C., Holland, A. E., Jones, A. YM., Kho, M. E., van der Lee, L., Moses, R., Ntoumenopoulos, G., Parry, S. M., & Patman, S. (2022). Physiotherapy management for COVID-19 in the acute hospital setting and beyond: an update to clinical practice recommendations. Journal of Physiotherapy, 68, 8-25. https://doi.org/10.1016/j.jphys.2021.12.012 ↵
- World Health Organization. (2023). WHO Coronavirus (COVID-19) Dashboard. [Data set]. Retrieved March 7, 2023, from https://covid19.who.int ↵
- Hodgson, C.L., Higgins, A.M, Bailey, M.J., Mather, A.M., Beach, L., Bellomo, R., Bissett, B., Boden, I.J., Bradley, S., Burrell, A., Cooper, D.J., Fulcher, B.J., Haines, K.J., Hopkins, J., Jones, A.Y.M., Lane, S., Lawrence, D., van der Lee, L., Liacos, J., Linke, N.J., Marques Gomes, L., Nickels, M., Ntoumenopoulos, G., Myles, P.S., Patman, S., Paton, M., Pound, G., Rai, S., Rix, A., Rollinson, T.C., Sivasuthan, J., Tipping, C.J., Thomas, P., Trapani, T., Udy, A.A., Whitehead, C., Hodgson, I.T., Anderson, S.A., Neto, A.S. & The COVID-Recovery Study Investigators and the ANZICS Clinical Trials Group. (2021). The impact of COVID-19 critical illness on new disability, functional outcomes and return to work at 6 months: a prospective cohort study. Crit Care, 25, 382. https://doi.org/10.1186/s13054-021-03794-0 ↵
- Lopez-Leon, S., Wegman-Ostrosky, T., Perelman, C., Sepulveda, R., Rebolledo, P. A., Cuapio, A., & Villapol, S. (2021). More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Scientific Reports 11, Article 16144. https://doi.org/10.1038/s41598-021-95565-8 ↵
- National Institute for Health and Care Excellence (NICE), Royal College of General Practitioners (RCGP) & Scottish Intercollegiate Guidelines Network (SIGN). (2022). COVID-19 rapid guideline: managing the long-term effects of COVID-19 (NICE guideline NG188). Retrieved March 7, 2023 from https://www.nice.org.uk/guidance/ng188 ↵
- Centers for Disease Control and Prevention. (2022, December 16). Long COVID or Post-COVID Conditions. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html ↵
- Gerlis, C., Barradell, A., Gardiner, N.Y., Chaplin, E., Goddard, A., Singh, S.J., & Daynes, E. (2022). The Recovery Journey and the Rehabilitation Boat – A qualitative study to explore experiences of COVID-19 rehabilitation. Chronic Respiratory Diseases, 19, 1-9. https://doi.org/10.1177/14799731221114266 ↵
- Gerlis, C., Barradell, A., Gardiner, N.Y., Chaplin, E., Goddard, A., Singh, S.J., & Daynes, E. (2022). The Recovery Journey and the Rehabilitation Boat – A qualitative study to explore experiences of COVID-19 rehabilitation. Chronic Respiratory Diseases, 19, 1-9. https://doi.org/10.1177/14799731221114266 ↵
- Brown, D.A., & O’Brien, K.K. (2021) Conceptualising Long COVID as an episodic health condition. BMJ Global Health, 6, e007004. https://doi.org/10.1136/bmjgh-2021-007004 ↵
- National Institute for Health and Care Excellence (NICE), Royal College of General Practitioners (RCGP) & Scottish Intercollegiate Guidelines Network (SIGN). (2022). COVID-19 rapid guideline: managing the long-term effects of COVID-19 (NICE guideline NG188). Retrieved March 7, 2023 from https://www.nice.org.uk/guidance/ng188 ↵
- Michelen, M., Manoharan, L. Elkheir, N., Cheng, V., Dagens, A., Hastie, C., O’Hara, M., Suett, J., Dahmash, D., Bugaeva, P., Rigby, I., Munblit, D., Harriss, E., Burls, A., Foote, C., Scott, J., Carson, G., Olliara, P., Sigfrid, L., & Stavropoulou, C. (2021). Characterising long COVID: a living systematic review. BMJ Global Health, 6(9), Article e005427. http://dx.doi.org/10.1136/bmjgh-2021-005427 ↵
- National Institute for Health and Care Excellence (NICE), Royal College of General Practitioners (RCGP) & Scottish Intercollegiate Guidelines Network (SIGN). (2022). COVID-19 rapid guideline: managing the long-term effects of COVID-19 (NICE guideline NG188). Retrieved March 7, 2023 from https://www.nice.org.uk/guidance/ng188 ↵
- Australian Physiotherapy Association. (2023) What Is Physio? Retrieved March 21, 2023, from https://choose.physio/what-is-physio ↵
- Bowyer, R. C. E., Huggins, C., Toms, R., Shaw, R. J., Hou, B., Thompson, E. J., Kwong, A. S. F., Williams, D. M., Kibble, M., Ploubidis, G. B., Timpson, N. J., Sterne, J. A. C., Chaturvedi, N., Steves, C. J., Tilling, K. & Silverwood, R. J. (2023). Characterising patterns of COVID‐19 and long COVID symptoms: evidence from nine UK longitudinal studies. European Journal of Epidemiology 38, 199-210. https://doi.org/10.1007/s10654-022-00962-6 ↵
- Brown, D.A., & O’Brien, K.K. (2021) Conceptualising Long COVID as an episodic health condition. BMJ Global Health, 6, e007004. https://doi.org/10.1136/bmjgh-2021-007004 ↵
- Centers for Disease Control and Prevention. (2022, December 16). Post-COVID Conditions: Information for Healthcare Providers. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html ↵
- Centers for Disease Control and Prevention. (2022, December 16). Post-COVID Conditions: Information for Healthcare Providers. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html ↵
- National COVID-19 Clinical Evidence Taskforce. (2023, May 30). Australian guidelines for the clinical care of people with COVID-19 (version 74.1). https://app.magicapp.org/#/guideline/L4Q5An ↵
- National Institute for Health and Care Excellence (NICE), Royal College of General Practitioners (RCGP) & Scottish Intercollegiate Guidelines Network (SIGN). (2022). COVID-19 rapid guideline: managing the long-term effects of COVID-19 (NICE guideline NG188). Retrieved March 7, 2023 from https://www.nice.org.uk/guidance/ng188 ↵
- Buttery, S., Philip, K.E.J., Williams, P., Fallas, A., West, B., Cumella, A., Cheung, C., Walker, S., Quint, J.K., Polkey, M.I., & Hopkinson, N.S. (2021). Patient symptoms and experience following COVID-19: results from a UK-wide survey. BMJ Open Resp Res, 8, e0001075. https://org/10.1136/ bmjresp-2021-001075 ↵
- Buttery, S., Philip, K.E.J., Williams, P., Fallas, A., West, B., Cumella, A., Cheung, C., Walker, S., Quint, J.K., Polkey, M.I., & Hopkinson, N.S. (2021). Patient symptoms and experience following COVID-19: results from a UK-wide survey. BMJ Open Resp Res, 8, e0001075. https://org/10.1136/ bmjresp-2021-001075 ↵
- Buttery, S., Philip, K.E.J., Williams, P., Fallas, A., West, B., Cumella, A., Cheung, C., Walker, S., Quint, J.K., Polkey, M.I., & Hopkinson, N.S. (2021). Patient symptoms and experience following COVID-19: results from a UK-wide survey. BMJ Open Resp Res, 8, e0001075. https://doi.org/10.1136/bmjresp-2021-001075 ↵
- National COVID-19 Clinical Evidence Taskforce. (2023, May 30). Australian guidelines for the clinical care of people with COVID-19 (version 74.1). https://app.magicapp.org/#/guideline/L4Q5An ↵
- National Institute for Health and Care Excellence (NICE), Royal College of General Practitioners (RCGP) & Scottish Intercollegiate Guidelines Network (SIGN). (2022). COVID-19 rapid guideline: managing the long-term effects of COVID-19 (NICE guideline NG188). Retrieved March 7, 2023 from https://www.nice.org.uk/guidance/ng188 ↵
- Crook, H., Raza, S., Nowell, J., Young, M., & Edison, P. (2021). Long covid – mechanisms, risk factors, and management. BMJ (Clinical research ed.), 374, n1648. https://doi.org/10.1136/bmj.n1648 ↵
- Bowyer, R. C. E., Huggins, C., Toms, R., Shaw, R. J., Hou, B., Thompson, E. J., Kwong, A. S. F., Williams, D. M., Kibble, M., Ploubidis, G. B., Timpson, N. J., Sterne, J. A. C., Chaturvedi, N., Steves, C. J., Tilling, K. & Silverwood, R. J. (2023). Characterising patterns of COVID‐19 and long COVID symptoms: evidence from nine UK longitudinal studies. European Journal of Epidemiology 38, 199-210. https://doi.org/10.1007/s10654-022-00962-6 ↵
- Crook, H., Raza, S., Nowell, J., Young, M., & Edison, P. (2021). Long covid – mechanisms, risk factors, and management. BMJ (Clinical research ed.), 374, n1648. https://doi.org/10.1136/bmj.n1648 ↵
- Centers for Disease Control and Prevention. (2022, December 16). Post-COVID Conditions: Information for Healthcare Providers. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html ↵
- National COVID-19 Clinical Evidence Taskforce. (2023, May 30). Australian guidelines for the clinical care of people with COVID-19 (version 74.1). https://app.magicapp.org/#/guideline/L4Q5An ↵
- Lopez-Leon, S., Wegman-Ostrosky, T., Perelman, C., Sepulveda, R., Rebolledo, P. A., Cuapio, A., & Villapol, S. (2021). More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Scientific Reports 11, Article 16144. https://doi.org/10.1038/s41598-021-95565-8 ↵
- Michelen, M., Manoharan, L. Elkheir, N., Cheng, V., Dagens, A., Hastie, C., O’Hara, M., Suett, J., Dahmash, D., Bugaeva, P., Rigby, I., Munblit, D., Harriss, E., Burls, A., Foote, C., Scott, J., Carson, G., Olliara, P., Sigfrid, L., & Stavropoulou, C. (2021). Characterising long COVID: a living systematic review. BMJ Global Health, 6(9), Article e005427. http://dx.doi.org/10.1136/bmjgh-2021-005427 ↵
- Reyes Domingo, F., Waddell, L., Cheung, A., Cooper, C., Belcourt, V., Zuckerman, A., Corrin, T., Ahmad, R., Boland, L., Laprise, C., Idzerda, L., Khan, A., Morissette, K., & Garcia, A. (2021). Prevalence of long-term effects in individuals diagnosed with COVID-19: an updated living systematic review. MedRxiv. https://doi.org/10.1101/2021.06.03.21258317 ↵
- Fernández-de-las-Peñas, C., Palacios-Ceña, D., Gómez-Mayordomo, V., Florencio, L.L., Cuadrado, M.L., Plaza-Manzano, G., and Navarro-Santana, M. (2021). Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. European Journal of Internal Medicine, 92, 55-70. https://doi.org/10.1016/j.ejim.2021.06.009 ↵
- Global Burden of Disease Long COVID Collaborators. Estimated Global Proportions of Individuals With Persistent Fatigue, Cognitive, and Respiratory Symptom Clusters Following Symptomatic COVID-19 in 2020 and 2021. JAMA. 2022;328(16):1604–1615. https://doi:10.1001/jama.2022.18931 ↵
- National Institute for Health and Care Excellence (NICE), Royal College of General Practitioners (RCGP) & Scottish Intercollegiate Guidelines Network (SIGN). (2022). COVID-19 rapid guideline: managing the long-term effects of COVID-19 (NICE guideline NG188). Retrieved March 7, 2023 from https://www.nice.org.uk/guidance/ng188 . Pg 42. ↵
- Buttery, S., Philip, K.E.J., Williams, P., Fallas, A., West, B., Cumella, A., Cheung, C., Walker, S., Quint, J.K., Polkey, M.I., & Hopkinson, N.S. (2021). Patient symptoms and experience following COVID-19: results from a UK-wide survey. BMJ Open Resp Res,8, e0001075. https://doi.org/10.1136/bmjresp-2021-001075 ↵
- Buttery, S., Philip, K.E.J., Williams, P., Fallas, A., West, B., Cumella, A., Cheung, C., Walker, S., Quint, J.K., Polkey, M.I., & Hopkinson, N.S. (2021). Patient symptoms and experience following COVID-19: results from a UK-wide survey. BMJ Open Resp Res, 8, e0001075. https://doi.org/10.1136/bmjresp-2021-001075 ↵
- Thomas, P., Baldwin, C., Beach, L., Bissett, B., Boden, I., Cruz, S. M., Gosselink, R., Granger C. L., Hodgson, C., Holland, A. E., Jones, A. YM., Kho, M. E., van der Lee, L., Moses, R., Ntoumenopoulos, G., Parry, S. M., & Patman, S. (2022). Physiotherapy management for COVID-19 in the acute hospital setting and beyond: an update to clinical practice recommendations. Journal of Physiotherapy, 68, 8-25. https://doi.org/10.1016/j.jphys.2021.12.012 ↵
- National COVID-19 Clinical Evidence Taskforce. (2023, May 30). Australian guidelines for the clinical care of people with COVID-19 (version 74.1). https://app.magicapp.org/#/guideline/L4Q5An ↵
- Allard, N., Miller, A., Morgan, M., & Chakraborty, S., (2022). Post-COVID -19 syndrome/condition or long COVID: Persistent illness after acute SARS CoV-2 infection. AJGP, 51 (12). Pp 952-957. https://doi.ord/10.31128/AJGP-05-22-6429 ↵
- House of Representatives Standing Committee on Health, Aged Care and Sport (2023). Sick and tired: Casting a long shadow. Inquiry into Long COVID and Repeated COVID Infections. Parliament of Australia. Canberra. Available at: https://parlinfo.aph.gov.au/parlInfo/download/committees/reportrep/RB000006/toc_pdf/SickandtiredCastingalongshadow.pdf[/footnote Physiotherapy assessment in the patient with symptoms suggestive of Long COVID should include a comprehensive history, including screening for the presence of any red flags (e.g., prior overlooked conditions such as malignancy, or complications of acute COVID-19 such as thromboembolic events, myopericarditis, dysrhythmias, seizures or encephalitis)[footnote]Yelin, D., Moschopoulos, C.D., Margalit, I., Gkrania-Klotsas, E., Landi, F., Stahl, J-P., & Yahav, D. (2022). ESCMID rapid guidelines for assessment and management of long COVID. Clinical Microbiology and Infection, 28 (7), 955-972. https://doi.org/10.1016/j.cmi.2022.02.018 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- Yelin, D., Moschopoulos, C.D., Margalit, I., Gkrania-Klotsas, E., Landi, F., Stahl, J-P., & Yahav, D. (2022). ESCMID rapid guidelines for assessment and management of long COVID. Clinical Microbiology and Infection, 28 (7), 955-972. https://doi.org/10.1016/j.cmi.2022.02.018 ↵
- National Institute for Health and Care Excellence (NICE), Royal College of General Practitioners (RCGP) & Scottish Intercollegiate Guidelines Network (SIGN). (2022). COVID-19 rapid guideline: managing the long-term effects of COVID-19 (NICE guideline NG188). Retrieved April 18, 2023 from https://www.nice.org.uk/guidance/ng188 ↵
- Thomas, P., Baldwin, C., Beach, L., Bissett, B., Boden, I., Cruz, S. M., Gosselink, R., Granger C. L., Hodgson, C., Holland, A. E., Jones, A. YM., Kho, M. E., van der Lee, L., Moses, R., Ntoumenopoulos, G., Parry, S. M., & Patman, S. (2022). Physiotherapy management for COVID-19 in the acute hospital setting and beyond: an update to clinical practice recommendations. Journal of Physiotherapy, 68, 8-25. https://doi.org/10.1016/j.jphys.2021.12.012 ↵
- Postigo-Martin P, Cantarero-Villanueva I, Lista-Paz A, Castro-Martín E, Arroyo-Morales M, Seco-Calvo J. A COVID-19 Rehabilitation Prospective Surveillance Model for Use by Physiotherapists. Journal of Clinical Medicine. 2021; 10(8):1691. https://doi.org/10.3390/jcm10081691 ↵
- World Health Organization. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline.https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- National Institute for Health and Care Excellence (NICE), Royal College of General Practitioners (RCGP) & Scottish Intercollegiate Guidelines Network (SIGN). (2022). COVID-19 rapid guideline: managing the long-term effects of COVID-19 (NICE guideline NG188). Retrieved April 18, 2023 from https://www.nice.org.uk/guidance/ng188 ↵
- Postigo-Martin P, Cantarero-Villanueva I, Lista-Paz A, Castro-Martín E, Arroyo-Morales M, Seco-Calvo J. A COVID-19 Rehabilitation Prospective Surveillance Model for Use by Physiotherapists. Journal of Clinical Medicine. 2021; 10(8):1691. https://doi.org/10.3390/jcm10081691 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Kortianou E.A., Mavronasou A., & Sapouna, V. (2022). Practicalities for Exercise Prescription in Long-COVID- 19 Rehabilitation. A Narrative Review. Medical Research Archives, 10(5), June 2022. https://doi.org/10.18103/mra.v10i5.2801 ↵
- Dillen, H., Bekkering, G., Gijsbers, S., Weygaerde, Y.V., Van Herck, M., Haesevoets, S., Bos, D.A.G., Li, A., Janssens, W., Gosselink, R., Troosters, T., and Verbakel, J.Y. (2023). Clinical effectiveness of rehabilitation in ambulatory care for patients with persisting symptoms after COVID-19: a systematic review. BMC Infectious Diseases, 23, 419. https://doi.org/10.1186/s12879-023-08374-x ↵
- Allied Health Professions Australia. (2023) Physiotherapy. Retrieved July 14, 2023, from https://ahpa.com.au/allied-health-professions/physiotherapy/ ↵
- Australian Physiotherapy Association. (2023) What Is Physio? Retrieved March 21, 2023, from https://choose.physio/what-is-physio ↵
- Kortianou E.A., Mavronasou A., & Sapouna, V. (2022). Practicalities for Exercise Prescription in Long-COVID- 19 Rehabilitation. A Narrative Review. Medical Research Archives, 10(5), June 2022. https://doi.org/10.18103/mra.v10i5.2801 ↵
- DeMars, J., Brown, D.A., Angelidis, I., Jones, F., McGuire, F., O’Brien, K.K., Oller, D., Pemberton, S., Tarrant, R., Verduzco-Gutierrez, M., & Gross, D.P. (2022). What is Safe Long COVID Rehabilitation? Journal of Occupational Rehabilitation 33, 227–230 (2023). https://doi.org/10.1007/s10926-022-10075-2 ↵
- Nopp, S., Moik, F., Klok, F.A., Gattinger, D., Petrovic, M., Vonbank, K., Koczulla, A.R., Ay, C., & Zwick, R.H. (2022). Outpatient Pulmonary Rehabilitation in Patients with Long COVID Improves Exercise Capacity, Functional Status, Dyspnea, Fatigue, and Quality of Life. Respiration, 101 (6), 593-601. https://doi.org/10.1159/000522118 ↵
- Thomas, P., Baldwin, C., Beach, L., Bissett, B., Boden, I., Cruz, S. M., Gosselink, R., Granger C. L., Hodgson, C., Holland, A. E., Jones, A. YM., Kho, M. E., van der Lee, L., Moses, R., Ntoumenopoulos, G., Parry, S. M., & Patman, S. (2022). Physiotherapy management for COVID-19 in the acute hospital setting and beyond: an update to clinical practice recommendations. Journal of Physiotherapy, 68, 8-25. https://doi.org/10.1016/j.jphys.2021.12.012 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline.https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Barbara, C., Clavario, P., De Marzo, V., Lotti, R., Guglielmi, G., Porcile, A., Russo, C., Griffo, R., Mäkikallio, T., Hautala, A.J., & Porto, I., (2022). Effects of exercise rehabilitation in patients with long coronavirus disease 2019. European Journal of Preventive Cardiology, 29, e258-e260. https://doi.org/10.1093/eurjpc/zwac019 ↵
- Nopp, S., Moik, F., Klok, F.A., Gattinger, D., Petrovic, M., Vonbank, K., Koczulla, A.R., Ay, C., & Zwick, R.H. (2022). Outpatient Pulmonary Rehabilitation in Patients with Long COVID Improves Exercise Capacity, Functional Status, Dyspnea, Fatigue, and Quality of Life. Respiration, 101 (6), 593-601. https://doi.org/10.1159/000522118 ↵
- Smith, J.L., Deighton, K., Innes, A.Q., Holl, M., Mould, L., Liao, Z., Doherty, P., Whyte, G., King, J.A., Deniszczyc, D. & Kelly, B.M. (2023). Improved clinical outcomes in response to a 12-week blended digital and community-based long-COVID-19 rehabilitation programme. Front. Med. 10:1149922. https://doi.org/10.3389/fmed.2023.1149922 ↵
- Kortianou E.A., Mavronasou A., & Sapouna, V. (2022). Practicalities for Exercise Prescription in Long-COVID- 19 Rehabilitation. A Narrative Review. Medical Research Archives, 10(5), June 2022. https://doi.org/10.18103/mra.v10i5.2801 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- DeMars, J., Brown, D.A., Angelidis, I., Jones, F., McGuire, F., O’Brien, K.K., Oller, D., Pemberton, S., Tarrant, R., Verduzco-Gutierrez, M., & Gross, D.P. (2022). What is Safe Long COVID Rehabilitation? Journal of Occupational Rehabilitation 33, 227–230 (2023). https://doi.org/10.1007/s10926-022-10075-2 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- Postigo-Martin P, Cantarero-Villanueva I, Lista-Paz A, Castro-Martín E, Arroyo-Morales M, Seco-Calvo J. A COVID-19 Rehabilitation Prospective Surveillance Model for Use by Physiotherapists. Journal of Clinical Medicine. 2021; 10(8):1691. https://doi.org/10.3390/jcm10081691 ↵
- Kortianou E.A., Mavronasou A., & Sapouna, V. (2022). Practicalities for Exercise Prescription in Long-COVID- 19 Rehabilitation. A Narrative Review. Medical Research Archives, 10(5), June 2022. https://doi.org/10.18103/mra.v10i5.2801 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- DeMars, J., Brown, D.A., Angelidis, I., Jones, F., McGuire, F., O’Brien, K.K., Oller, D., Pemberton, S., Tarrant, R., Verduzco-Gutierrez, M., & Gross, D.P. (2022). What is Safe Long COVID Rehabilitation? Journal of Occupational Rehabilitation 33, 227–230 (2023). https://doi.org/10.1007/s10926-022-10075-2 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- DeMars, J., Brown, D.A., Angelidis, I., Jones, F., McGuire, F., O’Brien, K.K., Oller, D., Pemberton, S., Tarrant, R., Verduzco-Gutierrez, M., & Gross, D.P. (2022). What is Safe Long COVID Rehabilitation? Journal of Occupational Rehabilitation 33, 227–230 (2023). https://doi.org/10.1007/s10926-022-10075-2 ↵
- Postigo-Martin P, Cantarero-Villanueva I, Lista-Paz A, Castro-Martín E, Arroyo-Morales M, Seco-Calvo J. A COVID-19 Rehabilitation Prospective Surveillance Model for Use by Physiotherapists. Journal of Clinical Medicine. 2021; 10(8):1691. https://doi.org/10.3390/jcm10081691 ↵
- NIHR Themed Review: Living with Covid19 - Second review; March 2021; doi:10.3310/themedreview_45225 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Kortianou E.A., Mavronasou A., & Sapouna, V. (2022). Practicalities for Exercise Prescription in Long-COVID- 19 Rehabilitation. A Narrative Review. Medical Research Archives, 10(5), June 2022. https://doi.org/10.18103/mra.v10i5.2801 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Kortianou E.A., Mavronasou A., & Sapouna, V. (2022). Practicalities for Exercise Prescription in Long-COVID- 19 Rehabilitation. A Narrative Review. Medical Research Archives, 10(5), June 2022. https://doi.org/10.18103/mra.v10i5.2801 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- Kotecha, T., Knight, D. S., Razvi, Y., Kumar, K., Vimalesvaran, K., Thornton, G., Patel, R., Chacko, L., Brown, J. T., Coyle, C., Leith, D., Shetye, A., Ariff, B., Bell, R., Captur, G., Coleman, M., Goldring, J., Gopalan, D., Heightman, M., Hillman, T., … Fontana, M. (2021). Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. European heart journal, 42(19), 1866–1878. https://doi.org/10.1093/eurheartj/ehab075 ↵
- Yan Z, Yang M, Lai C-L. Long COVID-19 Syndrome: A Comprehensive Review of Its Effect on Various Organ Systems and Recommendation on Rehabilitation Plans. Biomedicines. 2021; 9(8):966. https://doi.org/10.3390/biomedicines9080966 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- Thomas, P., Baldwin, C., Beach, L., Bissett, B., Boden, I., Cruz, S. M., Gosselink, R., Granger C. L., Hodgson, C., Holland, A. E., Jones, A. YM., Kho, M. E., van der Lee, L., Moses, R., Ntoumenopoulos, G., Parry, S. M., & Patman, S. (2022). Physiotherapy management for COVID-19 in the acute hospital setting and beyond: an update to clinical practice recommendations. Journal of Physiotherapy, 68, 8-25. https://doi.org/10.1016/j.jphys.2021.12.012 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Twomey, R., DeMars, J., Franklin, K., Culos-Reed, S. N., Weatherald, J., & Wrightson, J. G. (2022). Chronic Fatigue and Postexertional Malaise in People Living With Long COVID: An Observational Study. Physical therapy, 102(4), pzac005. https://doi.org/10.1093/ptj/pzac005 ↵
- Davis, H.E., Assaf, G.S., McCorkell, L., Wei, H., Low, R.J., Re’em, Y., Redfield, S., Austin, J.P., & Akrami, A. (2021). Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine, 38 (101019). https://doi.org/10.1016/j.eclinm.2021.101019 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Twomey, R., DeMars, J., Franklin, K., Culos-Reed, S. N., Weatherald, J., & Wrightson, J. G. (2022). Chronic Fatigue and Postexertional Malaise in People Living With Long COVID: An Observational Study. Physical therapy, 102(4), pzac005. https://doi.org/10.1093/ptj/pzac005 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Twomey, R., DeMars, J., Franklin, K., Culos-Reed, S. N., Weatherald, J., & Wrightson, J. G. (2022). Chronic Fatigue and Postexertional Malaise in People Living With Long COVID: An Observational Study. Physical therapy, 102(4), pzac005. https://doi.org/10.1093/ptj/pzac005 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Décary, S., Gaboury, I., Poirier, S., Garcia, C., Simpson, S., Bull, M., Brown, D., & Daigle, F. (2021)[Editorial]. Humility and Acceptance: Working Within Our Limits With Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Journal of Orthopaedic & Sports Physical Therapy, 51 (5); 197-200. https://doi.org/10.2519/jospt.2021.0106 ↵
- Ghali, A., Lacombe, V., Ravaiau, C., Delattre, E., Ghali, M., Urbanski, G., & Lavigne, C. (2023). The relevance of pacing strategies in managing symptoms of post-COVID-19 syndrome. Journal of Translational Medicine, 21 (375). https://doi.org/10.1186/s12967-023-04229-w ↵
- Décary, S., Gaboury, I., Poirier, S., Garcia, C., Simpson, S., Bull, M., Brown, D., & Daigle, F. (2021)[Editorial]. Humility and Acceptance: Working Within Our Limits With Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Journal of Orthopaedic & Sports Physical Therapy, 51 (5); 197-200. https://doi.org/10.2519/jospt.2021.0106 ↵
- Ghali, A., Lacombe, V., Ravaiau, C., Delattre, E., Ghali, M., Urbanski, G., & Lavigne, C. (2023). The relevance of pacing strategies in managing symptoms of post-COVID-19 syndrome. Journal of Translational Medicine, 21 (375). https://doi.org/10.1186/s12967-023-04229-w ↵
- Jason, Leonard A., Melrose, Harriet, Lerman, Allison, Burroughs, Veronica, Lewis, Kelly, King, Caroline P., & Frankenberry, Erin L. (1999). Managing Chronic Fatigue Syndrome: Overview and Case Study. AAOHN Journal, 47(1), 17–21. https://doi.org/10.1177/216507999904700104 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Ghali, A., Lacombe, V., Ravaiau, C., Delattre, E., Ghali, M., Urbanski, G., & Lavigne, C. (2023). The relevance of pacing strategies in managing symptoms of post-COVID-19 syndrome. Journal of Translational Medicine, 21 (375). https://doi.org/10.1186/s12967-023-04229-w ↵
- Campbell, B. (2021, October 4). Pacing by Numbers: Using your heart rate to stay inside the energy envelope. ME/CFS & Fibromyalgia Self-Help. https://www.cfsselfhelp.org/library/pacing-numbers-using-your-heart-rate-to-stay-inside-energy-envelope ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- Blitshteyn S., Whiteson, J.H., Abramoff, B., Azola, A., Bartels, M.N., Bhavaraju-Sanka, R., Chung, T., Fleming, T.K., Henning, E., Miglis, M.G., Sampsel, S., Silver, J.K., Tosto, J., Verduzco-Gutierrez, M., & Putrino, D. (2022). Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM&R. 2022;14(10):1270‐1291. https://doi.org/10.1002/pmrj.12894 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Blitshteyn S., Whiteson, J.H., Abramoff, B., Azola, A., Bartels, M.N., Bhavaraju-Sanka, R., Chung, T., Fleming, T.K., Henning, E., Miglis, M.G., Sampsel, S., Silver, J.K., Tosto, J., Verduzco-Gutierrez, M., & Putrino, D. (2022). Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM&R. 2022;14(10):1270‐1291. https://doi.org/10.1002/pmrj.12894 ↵
- Espinosa-Gonzalez A B, Master H, Gall N, Halpin S, Rogers N, Greenhalgh T et al. Orthostatic tachycardia after covid-19 BMJ 2023; 380 :e073488 https://doi.org/10.1136/bmj-2022-073488 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- Blitshteyn S., Whiteson, J.H., Abramoff, B., Azola, A., Bartels, M.N., Bhavaraju-Sanka, R., Chung, T., Fleming, T.K., Henning, E., Miglis, M.G., Sampsel, S., Silver, J.K., Tosto, J., Verduzco-Gutierrez, M., & Putrino, D. (2022). Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM&R. 2022;14(10):1270‐1291. https://doi.org/10.1002/pmrj.12894 ↵
- Dani M, Dirksen A, Taraborrelli P, Torocastro M, Panagopoulos D, Sutton R, Lim PB. Autonomic dysfunction in 'long COVID': rationale, physiology and management strategies. Clin Med (Lond). 2021 Jan;21(1):e63-e67. https://doi.org/10.7861/clinmed.2020-0896 ↵
- Dani M, Dirksen A, Taraborrelli P, Torocastro M, Panagopoulos D, Sutton R, Lim PB. Autonomic dysfunction in 'long COVID': rationale, physiology and management strategies. Clin Med (Lond). 2021 Jan;21(1):e63-e67. https://doi.org/10.7861/clinmed.2020-0896 ↵
- Blitshteyn S., Whiteson, J.H., Abramoff, B., Azola, A., Bartels, M.N., Bhavaraju-Sanka, R., Chung, T., Fleming, T.K., Henning, E., Miglis, M.G., Sampsel, S., Silver, J.K., Tosto, J., Verduzco-Gutierrez, M., & Putrino, D. (2022). Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM&R. 2022;14(10):1270‐1291. https://doi.org/10.1002/pmrj.12894 ↵
- Blitshteyn S., Whiteson, J.H., Abramoff, B., Azola, A., Bartels, M.N., Bhavaraju-Sanka, R., Chung, T., Fleming, T.K., Henning, E., Miglis, M.G., Sampsel, S., Silver, J.K., Tosto, J., Verduzco-Gutierrez, M., & Putrino, D. (2022). Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM&R. 2022;14(10):1270‐1291. https://doi.org/10.1002/pmrj.12894 ↵
- Espinosa-Gonzalez A., Master H., Gall N., Halpin S., Rogers N., & Greenhalgh T. (2023). Orthostatic tachycardia after covid-19. BMJ; 380 :e073488 https://doi.org/10.1136/bmj-2022-073488 ↵
- Blitshteyn S., Whiteson, J.H., Abramoff, B., Azola, A., Bartels, M.N., Bhavaraju-Sanka, R., Chung, T., Fleming, T.K., Henning, E., Miglis, M.G., Sampsel, S., Silver, J.K., Tosto, J., Verduzco-Gutierrez, M., & Putrino, D. (2022). Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM&R. 2022;14(10):1270‐1291. https://doi.org/10.1002/pmrj.12894 ↵
- Espinosa-Gonzalez A., Master H., Gall N., Halpin S., Rogers N., & Greenhalgh T. (2023). Orthostatic tachycardia after covid-19. BMJ; 380 :e073488 https://doi.org/10.1136/bmj-2022-073488 ↵
- Dani M, Dirksen A, Taraborrelli P, Torocastro M, Panagopoulos D, Sutton R, Lim PB. Autonomic dysfunction in 'long COVID': rationale, physiology and management strategies. Clin Med (Lond). 2021 Jan;21(1):e63-e67.https://doi.org/10.7861/clinmed.2020-0896 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- Blitshteyn S., Whiteson, J.H., Abramoff, B., Azola, A., Bartels, M.N., Bhavaraju-Sanka, R., Chung, T., Fleming, T.K., Henning, E., Miglis, M.G., Sampsel, S., Silver, J.K., Tosto, J., Verduzco-Gutierrez, M., & Putrino, D. (2022). Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM&R. 2022;14(10):1270‐1291. https://doi.org/10.1002/pmrj.12894 ↵
- Kavi, L. (2022). Postural tachycardia syndrome and long COVID: an update. British Journal of General Practice, 72, (714), 8-9. https://doi.org/10.3399/bjgp22X718037 ↵
- Putrino, D., Tabacof, L., Tosto-Mancuso, J., Wood, J., Cortes, M., Kontorovich, A., McCarthy, D., Breyman, E., Nasr, A., Duntz, J., Bunt, A., Herrera, J., & Kellner, C. (2021). Autonomic conditioning therapy reduces fatigue and improves global impression of change in individuals with post-acute COVID-19 syndrome. Research Square. https://doi.org/10.21203/rs.3.rs-440909/v1 ↵
- Putrino, D., Tabacof, L., Tosto-Mancuso, J., Wood, J., Cortes, M., Kontorovich, A., McCarthy, D., Breyman, E., Nasr, A., Duntz, J., Bunt, A., Herrera, J., & Kellner, C. (2021). Autonomic conditioning therapy reduces fatigue and improves global impression of change in individuals with post-acute COVID-19 syndrome. Research Square. https://doi.org/10.21203/rs.3.rs-440909/v1 ↵
- Putrino, D., Tabacof, L., Tosto-Mancuso, J., Wood, J., Cortes, M., Kontorovich, A., McCarthy, D., Breyman, E., Nasr, A., Duntz, J., Bunt, A., Herrera, J., & Kellner, C. (2021). Autonomic conditioning therapy reduces fatigue and improves global impression of change in individuals with post-acute COVID-19 syndrome. Research Square. https://doi.org/10.21203/rs.3.rs-440909/v1 ↵
- Putrino, D., Tabacof, L., Tosto-Mancuso, J., Wood, J., Cortes, M., Kontorovich, A., McCarthy, D., Breyman, E., Nasr, A., Duntz, J., Bunt, A., Herrera, J., & Kellner, C. (2021). Autonomic conditioning therapy reduces fatigue and improves global impression of change in individuals with post-acute COVID-19 syndrome. Research Square. https://doi.org/10.21203/rs.3.rs-440909/v1 ↵
- DeMars, J., Brown, D.A., Angelidis, I., Jones, F., McGuire, F., O’Brien, K.K., Oller, D., Pemberton, S., Tarrant, R., Verduzco-Gutierrez, M., & Gross, D.P. (2022). What is Safe Long COVID Rehabilitation? Journal of Occupational Rehabilitation 33, 227–230 (2023). https://doi.org/10.1007/s10926-022-10075-2 ↵
- World Physiotherapy. (2021). World Physiotherapy Response to COVID-19 Briefing Paper 9. Safe rehabilitation approaches for people living with Long COVID: physical activity and exercise. London, UK: World Physiotherapy; 2021. Available from https://world.physio/sites/default/files/2021-07/Briefing-Paper-9-Long-Covid-FINAL-English-202107.pdf?logged_in=true ↵
- National COVID-19 Clinical Evidence Taskforce. (2023, May 30). Australian guidelines for the clinical care of people with COVID-19 (version 74.1). https://app.magicapp.org/#/guideline/L4Q5An ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- Khoja, O., Passadouro, B.S., Mulvey, M., Delis, I., Astill, S., Tan, A.L., and Sivan, M. (2022). Clinical Characteristics and Mechanisms of Musculoskeletal Pain in Long COVID. Journal of Pain Research. 15:1729-1748 https://doi.org/10.2147/JPR.S365026 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- Genecand, L., Altarelli, M., Binkova, A., Loew, S., Vaudan, S., Gex, G., Bridevaux, P-O., & Frésard, I. (2023). Dysfunctional breathing symptoms, functional impact and quality of life in patients with long COVID-19: a prospective case series. BMJ Open Respir Res. 10:e001770. https://doi.org/10.1136/bmjresp-2023-001770 ↵
- Genecand, L., Altarelli, M., Binkova, A., Loew, S., Vaudan, S., Gex, G., Bridevaux, P-O., & Frésard, I. (2023). Dysfunctional breathing symptoms, functional impact and quality of life in patients with long COVID-19: a prospective case series. BMJ Open Respir Res. 10:e001770. https://doi.org/10.1136/bmjresp-2023-001770 ↵
- World Health Organisation. (2023, August 18). Clinical management of COVID-19: living guideline. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 ↵
- Genecand, L., Altarelli, M., Binkova, A., Loew, S., Vaudan, S., Gex, G., Bridevaux, P-O., & Frésard, I. (2023). Dysfunctional breathing symptoms, functional impact and quality of life in patients with long COVID-19: a prospective case series. BMJ Open Respir Res. 10:e001770. https://doi.org/10.1136/bmjresp-2023-001770 ↵
- House of Representatives Standing Committee on Health, Aged Care and Sport (2023). Sick and tired: Casting a long shadow. Inquiry into Long COVID and Repeated COVID Infections. Parliament of Australia. Canberra. Available at: https://parlinfo.aph.gov.au/parlInfo/download/committees/reportrep/RB000006/toc_pdf/SickandtiredCastingalongshadow.pdf ↵
- House of Representatives Standing Committee on Health, Aged Care and Sport (2023). Sick and tired: Casting a long shadow. Inquiry into Long COVID and Repeated COVID Infections. Parliament of Australia. Canberra. Available at: https://parlinfo.aph.gov.au/parlInfo/download/committees/reportrep/RB000006/toc_pdf/SickandtiredCastingalongshadow.pdf ↵
Severe Acute Respiratory Syndrome CoronaVirus 2
Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus (World Health Organisation)
Deep Vein Thrombosis
Pulmonary Embolus
A drop in blood oxygen level
Any muscle movement that works skeletal muscles and requires the production of energy
Planned, structured and repetitive physical activity with the goal to improve strength and/or fitness
Myalgic Encephalomyelitis / Chronic Fatigue Syndrome is a complex and disabling neurological condition
A drop in blood oxygen level
Whereby all physical activity is monitored continuously and then adjusted according to symptoms
A pattern of breathing where you breathe more quickly and deeply than normal
shortness of breath
Reading on a pulse oximeter that shows the percentage of oxygen in the blood
A scale from 0-10 that is used to rate how breathless you are during physical activity
A sensation that the heart is beating faster than usual, fluttering, pounding or skipping a beat.
A heart rate of more than 100 beats per minute
A loss of consciousness for a short period of time
Inflammation of the heart muscle
Post-Exertion Symptom Exacerbation
A general feeling of being ill or having no energy
Involves incremental increases in activity
is an approach to balancing activities with rest
Heart Rate
Autonomic Nervous System
The sensation of feeling like you are about to faint
Postural Orthostatic Tachycardia Syndrome
Autonomic Conditioning Therapy
Range Of Motion
Active Range of Motion
Straight Leg Raise
Rating of Perceived Exertion
Involvement in a life situation (ICF, WHO)
Pain in a joint
Pain in a muscle or group of muscles
Breathing Pattern Disorders
Dysfunctional Breathing
Pain persisting for more than three months

