Chapter 13: Evidence-Based Practice
Bethany Howard and Basia Diug
Uncertainty in Evidence-Based Practice
An evidence-based approach, through the adoption of evidence-based practice, is essential to all health professions and to the delivery of quality healthcare (Howard et al., 2022). Evidence-based practice is a framework that integrates best available evidence, clinical expertise, and patient values and preferences (Figure 13.1: click on each aspect to find out more). Each of these aspects informs clinical decision-making, yet junior practitioners tend to rely more heavily on evidence (Howard et al., 2022).
|
Figure 13.1 Evidence-Based Practice as the Intersection of Clinical Expertise, Best Available Evidence, and Patient Values and Preferences (Sackett et al., 1996, p. 71-72) |
The types of evidence that predominantly inform decision-making are systematic reviews and clinical guidelines. Systematic reviews, such as those developed by Cochrane collaboration (https://www.cochrane.org), utilise robust research methods to assess and integrate the published research on a topic. Clinical guidelines, informed by systematic reviews and primary research, aim to ensure appropriate patient care. However, these resources can be limited in their ability to support clinical decision-making. Despite evidence often being perceived as objective and certain, many systematic reviews conclude that there is insufficient, inconclusive, or even conflicting evidence on a topic. This can be the result of a lack of evidence, variable quality of evidence, conflicting findings, or restrictions in the nature of the evidence that can be collected (e.g., randomised controlled trials are not always feasible or ethical). Simultaneously, the proliferation and ongoing nature of medical and health research lead to systematic reviews and clinical guidelines being regularly updated. Therefore, ascertaining the best available evidence on a given topic is fraught with uncertainty and requires evidence-based practice skills that must be explicitly taught and developed as part of health professions curricula.
Priorities to Prepare Learners for Uncertainty in Evidence-Based Practice
To effectively adopt evidence-based practice, health professions learners must embrace the facts that there are many remaining gaps in the evidence base and that evidence is constantly evolving. Learners also need to integrate uncertainties in the evidence base with potential further uncertainties introduced by a patient’s values and preferences. Therefore, learners must be able to critically engage and appraise evidence and research. The five As of evidence-based practice (Ask, Acquire, Appraise, Apply, and Assess; Howard et al., 2022) are helpful in this area, providing a way to navigate the uncertainty in evidence and to inform healthcare decision-making. Across the five As, 68 evidence-based practice core competencies have been identified, such as generating answerable clinical questions using the population, intervention, comparator, and outcome (PICO) framework; searching the literature; and interpreting the risk of bias (Albarqouni et al., 2018). All of the core competencies can be acquired through designated and authentic evidence-based practice teaching and learning.
Fostering Uncertainty Tolerance in Evidence-Based Practice Learners
Authentic assessments, where learners apply their knowledge and skills in real life scenarios or settings, facilitate learners’ application of complex problem-solving skills and knowledge to real-world tasks (Ashford-Rowe et al., 2014). The use of complementary and alternative medicines – therapeutic and diagnostic approaches that complement and differ from mainstream medicine – is the context of the authentic assessment described in this chapter. Two in three Australians engage with complementary and alternative medicines, indicating that it is a predominant patient value and preference, but the limitations of its ‘light-touch’ regulation require further exploration (von Conrady & Bonney, 2017). Learners need to understand the limited regulation of these products and be able to initiate conversations about their evidence base, risks and benefits.
The Whack-A-Mole project was devised to enable learners to apply evidence-based practice skills to investigate the promotion and regulation of complementary medicines in Australia and to help guide their use. It was named after the arcade game which requires players to hit (whack) toy moles as they pop up at random, sometimes simultaneously. In this case, the ‘moles’ are the claims made by makers of complementary and alternative medicines, and ‘whacking’ is achieved by students’ investigations of the claims and identification of a discrepancy. The project includes elements of unpredictability, complexity, and creativity: areas that are important when teaching evidence-based practice and fostering uncertainty tolerance among health professions learners.
Exemplar Activity: Evidence-Based Practice
Activity Origin
The Whack-A-Mole project was developed and implemented in a biomedical science capstone unit at Monash University, Melbourne, that incorporated biomedical and epidemiological bases of disease. The bachelor of biomedical science is a three-year pre-medical degree that incorporates study in anatomy, biochemistry, biology, genetics, immunology, pharmacology, physiology, and public health.
Sources of Uncertainty
Sources of uncertainty in the Whack-A-Mole project are found across the five As of evidence-based practice (Ask, Acquire, Appraise, Apply, and Assess). Further uncertainty may arise through the teamwork required for the project, with learners needing to manage differing opinions and preferences within their peer group. These uncertainties are detailed below.
Facilitator Guide
The Whack-A-Mole project was a key component of a biomedical science capstone unit delivered across a 12-week semester to approximately 500 students in the years 2016–2022. The unit integrated understanding of human disease from a biomedical and epidemiological perspective via lectures, in-class learning, and online resources.
The project requires learners to select a complementary or alternative medicine product, investigate it or advertising claims about it, and report on any breaches of the Therapeutic Goods Act 1989 (see Activity). Tasks are completed in self-selected teams of three to five learners (moderator: diverse teamwork). The project is assessed via a written report submitted in Week 8 and creative output submitted in Week 11.
Learners are supported through engagement with pre-class and in-class resources (moderator: setting clear expectations) on the core principles of evidence-based practice and other requisite skills (Table 13.1). Students also work with their peers outside class to complete the tasks required.
Table 13.1 Facilitation of the Whack-A-Mole Project and Requisite Knowledge and Skill Development in Relation to Evidence-Based Practice
| Knowledge/Skill | Before Class | In Class |
|---|---|---|
| Ask Define the research question and scope using the PICO framework |
Week 1, Online module • Introduction to five As of evidence-based practice • Importance of focussed questions • Different question types • Use of PICO framework (Includes interactive examples for learners to apply knowledge and skills) |
Week 1, Tutorial • Reiteration of concepts covered in the online module • Guided examples (clinical scenarios), firstly as a class, then in groups, and then individually |
| Acquire Search the literature using advanced searching techniques |
Week 2, Online module • Converting PICO to search strategy • Developing a search plan • Introduction to database searching |
Week 2, Session run by librarians • Use of OVID Medline (Includes subject headings, synonyms, keywords, truncation, and Boolean operators) |
| Healthcare regulation: Reviewing the regulatory framework and context |
Week 2, Lecture recording • How complementary and alternative medicines are regulated in Australia (Includes numerous examples) |
Weeks 2–3, Tutorial • Regulation of healthcare workforce and products in Australia |
| Acquire Select the best available evidence through the establishment of inclusion and exclusion criteria and screening techniques |
Week 4, Online module • Use of Covidence for screening |
Week 4, Tutorial • Learners apply online module to their assessments • Learners establish their inclusion and exclusion criteria • Facilitators support learners in their assessment work |
| Appraise Critically appraise the literature by understanding the hierarchy of evidence, strengths and weaknesses of different study designs, risk of bias, and statistical and clinical significance |
Weeks 5–7, Online module • Epidemiological study design • Sources of error in epidemiology (Used in earlier unit; provided as revision material) • Assessing the risk of bias in studies |
Weeks 5–7, Test of learners’ knowledge • Principles learned in an earlier unit reviewed with Kahoot! and trivia questions |
| Apply Translate evidence to address misinformation and account for varied health literacy |
- | Week 8, Tutorial • Health literacy (Includes what it is, why it is important, who is affected, and how it can be assessed using the Patient Education Materials Assessment Tool*) |
| Apply Visually communicate findings |
Week 9, Online module • Use of typography, colour, layout, symbols, and icons (Includes a mix of YouTube videos and text) |
Week 9, Tutorial • Learners apply online module to their assessments (Facilitators are available to answer queries) |
| Effective teamwork Devising a team project plan that includes approaches to team communication and collaboration |
Week 3, Online module • Why good teamwork is important • Professional interactions (including handling conflict) • Learners individually complete a teamwork evaluation form |
Week 8, Teamwork feedback session • Using the teamwork evaluation forms, team members have facilitated discussions about their teamwork (Includes addressing concerns about and building upon their teamwork) |
* Agency for Research and Healthcare Quality, 2020
To adequately deliver the tutorials and support learners through the activity, educators need a strong understanding of evidence-based practice and research skills (moderator: workforce performance standards). In the authors’ context, the teaching team, which delivered the in-class learning, included current PhD candidates, clinical researchers, and trained experts in public health (e.g., master of public health graduates) or clinical disciplines (e.g., physiotherapists, doctors, nurses, paramedics, exercise physiologists) (moderator: educator diversity). Classes had a ratio of one educator to 30 learners.
Facilitators were supported in delivering the content through the provision of all resources (e.g., slides for classes) and weekly meetings to review and preview the preceding and upcoming classes (moderator: communities of practice). They could navigate their own uncertainties in discussions with their peers and the lead educator (unit coordinator) during the weekly meetings and via the team communications channel (moderators: communicating uncertainty; psychological safety). Learners had access to the unit coordinator through the learning management system forum and two live question-and-answer sessions during the unit (one for each assessment task) (moderator: expert guidance).
Activity
The assessment description below is provided to learners at the start of the semester. The steps require application of the five As of evidence-based practice during navigation of various forms of uncertainty. Learners identify a complementary and alternative medicine product that they consider worthy of investigation and develop a research question that is sufficiently broad, yet specific enough to encompass all the relevant literature. They are encouraged to work together on each step, critically analysing their choices and the evidence.
Whack-A-Mole Project
Recently, you have noticed several people using a particular complementary or alternative medicine product to address their health concerns. This is concerning, as the claims made by the product’s manufacturer and sponsors seem questionable. To determine whether the claims about the product are evidence based, you gather a team of health experts trained in evidence-based medicine. As a team, you investigate the claims and write a report to share with other health experts (moderator: diverse teamwork). To ensure your report is useful to others, you pay attention to being succinct and transparent in describing your investigation (moderator: scaffolding uncertainty).
Choose Your Product
As a team, make a list of potential complementary and alternative medicine products, discuss each one, and select one to investigate further. When selecting your product, check whether it is listed on the Australian Register of Therapeutic Goods (Therapeutic Goods Administration, 2024). If it isn’t, it may not be sold in Australia or may be considered a food or beverage product. You can still investigate it but be mindful of which organisation is responsible for regulating it. In addition, do a basic background search to see what evidence may be available relating to the product claims. Finally, choose the product you are most interested in further investigating!
Once you have chosen your product, continue with the five As of evidence-based practice: Ask, Acquire, Appraise, Apply, and Assess.
Ask - Refine Your Question
Keep your question focussed, using the PICO framework. Some pointers for this are listed below:
Population Most complementary and alternative medicine products do not have a specific target population, though some may be aimed at children, men, or women, for example.
Intervention Only examine the ingredients in your product that relate to the claim you are disputing.
Comparison Many products may not have a comparator. If your chosen product does, focus on the active ingredient that is different.
Outcomes Address the main claims related to the product. Be specific: pick one or two claims (the most fanciful) and focus on those.
Acquire - Search for and Collect the Best Available Evidence
For a comprehensive search to acquire the best available evidence, firstly, use a reproducible search strategy in relevant databases (e.g., Medline, Cochrane) and check the Australian and New Zealand Clinical Trials Registry (2024) (moderators: scaffolding uncertainty, expert guidance). Read any studies cited by the company that makes or sponsors the product, and, if necessary (e.g., if you cannot find a reference cited in advertisements or if the company claims, ‘Data on file’), contact the sponsor and/or manufacturer via email and ask if they have conducted any relevant studies. Ensure you uphold the research principles that we value by being transparent (e.g., be honest about who you are and why you are enquiring) in any communications with industry. Do not use fake names or emails, and please be polite. If the company does not respond, just note this in your report.
To identify the best available evidence, use screening processes. Only one person needs to screen each article, and you are looking for the best available evidence. This means you should not use a randomised controlled trial filter, as you are interested in all studies in the area and need to look at all the evidence, including observational studies (cross-sectional, case-control, and cohort). This means digging a little deeper: investigate further, use Google to search the grey literature, and check the references on any evidence you find. An old study may be all that exists. Also, product sponsors may cherry-pick an old, poorly conducted study and ignore a more recent, better conducted study that contradicts their claims. In addition, do not put a time limit on your search, as you might miss something.
If you are getting too many search results to screen (i.e., over 3000), consider whether your claim or your search terms are too broad, and what your PICO is. Focus on the key ingredient.
If you don’t find any significant results and there are no human trials on record, animal studies may provide some (but insufficient) evidence to support the product claims. Sometimes, the literature simply doesn’t exist. If you have exhausted all possible options, congratulations! You have found a mole to whack!
Appraise - Critically Evaluate the Evidence
For those that have found the evidence it is time to appraise. For those who have no evidence please go to the next step. In order to appraise use your knowledge of bias and confounding rather than a specific risk-of-bias tool. The following considerations provide a guide:
- Are any clinical trials registered and/or published?
- Could you retrieve the full publication or just the abstract? (The latter often lacks important details, such as conflict of interest statements.)
- In what journal was the evidence published? Is it reputable? Is it predatory? (Conference proceedings are often positive but never published as full papers.)
- When was the trial conducted? (Old trial results may have been superseded by newer, better conducted trials.)
- What institution was the study conducted at?
- Was ethics approval obtained?
- Is there a conflict-of-interest statement?
- What was the study design? How many participants were there? Were there any forms of bias?
It is important to ascertain whether the product studied in any trials you find was identical to that in the advertised claim – that is, were the ingredients or extracts in the advertised product identical to those shown to be efficacious in the clinical trials? While Australia’s Pharmaceutical Benefits Scheme prescription medicines are assessed for generic equivalence by the Therapeutic Goods Administration, one cannot assume that a generic ingredient in a complementary medicine, such as glucosamine or ginkgo biloba, has equal efficacy to a specific trialled ingredient.
You can also refer to the Therapeutic Goods Administration’s Evidence Guidelines to discover what evidence you need to support your scientific indication. If the product claims there is evidence of traditional use (e.g., as occurs with some homeopathic medicines) but modern scientific evidence contradicts a traditional claim, the claim can be whacked (refuted) (Therapeutic Goods Administration, 2022).
If the studies found evidence to support the claims made by the manufacturer of your product, this is great! Ultimately, we want all products that make health claims in Australia to be evidence based like this.
Apply - Summarise Findings in a Written Report for Healthcare Professionals
Introduction
In the opening section, describe the product you have selected, including its accessibility (e.g., cost, availability), and the claims you have investigated. Supply images of the product advertisements. Also, clearly document your PICO question in this section. Additional relevant inclusions will cover the following aspects:
Biomedical plausibility Is there any biological plausibility for the use of the product? You may recall that biological plausibility is one of the Bradford Hill criteria for establishing causality. ‘Hill’s criterion of plausibility is satisfied if the relationship is consistent with the current body of knowledge regarding the etiology and mechanism of disease’ (Fedak et al., 2015). You do not need to go into great detail here, but state (with references) whether there is plausibility or not.
Epidemiological significance What is the burden of disease for the health condition(s) that the claims relate to? For instance, why would it be important to have a product that is evidence-based and that supports the claims to improve health outcomes? What would it mean if the product did work as advertised?
Commercial interests How does the product sponsor benefit financially from selling the product? This information will be on the company’s website, in annual reports, if it is publicly traded. If the information is not available, then you can base this aspect generally around complementary medicine.
Methods
This section should outline the steps taken to investigate the product claims and must be documented such that it can be reproduced. Descriptions of the search strategy and selection criteria are important inclusions.
Results
Describe and depict your search results using a Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram (PRISMA, 2020). The results that you include should also be described and appraised, and they need to be presented as tables and/or graphs when relevant. If you have extensive tables, display them in landscape format while leaving the remainder of the document in portrait format.
Synthesise the results (i.e., write about them collectively rather than individually). For example, ‘X, y, and z studies had detection bias’. Follow up syntheses by using one or more individual results as an example, providing more specific details.
Discussion
The discussion section should provide summaries and interpretations of the results and report on the limitations and directions for further research. Some recommendations for possible actions based on the findings of your team’s investigation also need to appear in this section. The recommendations could relate to the following contexts:
Health experts What would you advise health experts to communicate to the community about the product?
Commercial interests What advice would you give to the manufacturer of the product to ensure that their product claims meet the regulation standards?
Research Is any research needed to enhance the product’s evidence base? If so, make recommendations for the research required.
Regulation What would you advise the regulator of the product to do? For example, should the product by removed from the market or can the claims be amended only on the product.
Provide details on how your recommendations could be realistically implemented, including consideration of the practical aspects (e.g., costs, time, resources).
Conclusion
The final section provides a summary of the entirety of the report. No new information should be provided.
Apply - Communicate Findings to Members of the Community
After writing up your report for health professionals, you realise that the findings also need to be communicated to members of your community. The patient values and preferences component of evidence-based practice is particularly relevant for this step. Consider your target audience and how best to communicate and connect with them.
(In the authors’ context, the communication format for this component has been an oral presentation, a video, and a health promotion campaign during the course’s lifetime. See below for further details.)
Impact
This activity was evaluated formally at a stage when the final component was delivered as a video. Four hundred and sixty-three final-year undergraduate biomedical science learners in 119 teams completed the project. Of the 116 learners (25%) who completed the online feedback questionnaire, 98 per cent found that their chosen product lacked evidence to support its manufacturer’s or sponsor’s claims. From these, a number of de-identified reports were submitted to the relevant regulators as 30 formal complaints, all of which were upheld. Some advertisers also changed their promotional material when learners asked them for evidence for the claims they were making about a product. Therefore, the activity has the potential to impact the broader community as well as learners.
Change in Perceptions
Most learners (92%, n=103) indicated that the Whack-A-Mole project changed their perceptions of complementary medicine and/or the regulation of goods and services in Australia, suggesting that the activity generated uncertainty by challenging learners’ preconceptions (stimulus) about the topic. The most frequently reported reasons for changed perceptions related to regulation (n=46), evidence for claims (n=39), use of complementary and alternative medicines (n=34), and scepticism (n=23).
Comments made by learners in the online feedback questionnaire are quoted within parentheses from hereon. Those comments relating to scepticism highlighted a shift towards a more evidence-based approach and likely greater questioning of information in future practice, as a result of completing the project (‘It’s made me realize I cannot trust all of the advice given to me’, ‘I will definitely be more skeptical in the future’, ‘I question everything now’). This could be attributed to questioning the evidence for claims (‘Just because they say it is clinically tested, it does not mean they have clinically significant results to support the claims they make’). As a result, many learners’ approaches to complementary and alternative medicine use changed (‘I now know how to search for whether a product works or not, especially with regards to safety, rather than spending the money and potentially harming myself. I’ve stopped using supplements and so has my family – encouraging everyone to just eat well and exercise and visit the doctor when sick. Life-changing assignment!’).
Of the learners who indicated the project didn’t change their perceptions (n=9), the reasons identified were prior knowledge (n=5) (‘I was relatively aware of the nature/state of complementary medicine prior to undertaking the whack-a-mole project’) and existing scepticism (n=4) (‘Already was sceptical of many complementary medicines’).
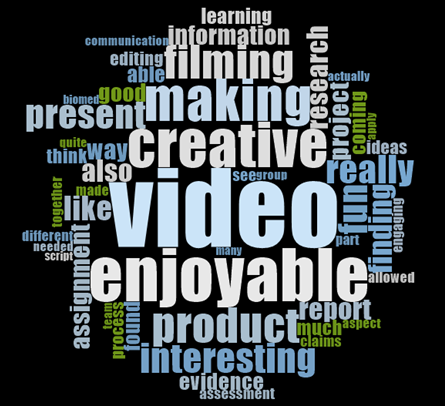
Most Enjoyable and Interesting Aspects
The most frequent responses (n=107) for the most enjoyable and interesting aspects of the Whack-A-Mole project were as follows:
- making the video (n=51)
- being creative (n=44)
- investigating the claims (n=25)
- teamwork (n=16)
- real-world application (n=15)
- selecting the product (n=12)
- watching the videos (n=12).
The most frequently used words were video (n=74), making (n=61), enjoy (n=52), and creative (n=42) (Figure 13.2). Taken together, these responses suggest that while the activity stimulated uncertainty, the mechanisms for moderating it may have reduced learners’ perceived risk, thereby enhancing the positive outcomes linked with uncertainty.
Of the learners who highlighted being creative, 28 linked this to the video task specifically (‘I really enjoyed the video making process. This is mainly because it has been the first creative assessment in a long time’). Learners also frequently (n=13) linked the creative aspect to fun (‘The opportunity for us to be creative because we don’t always get a chance to showcase our creativity … This has been the most fun project in biomed so far. So thank you!’). This suggests that the open pedagogy (moderator) helped support learners’ uncertainty tolerance by orienting them towards the freedom that came with the uncertainty in this activity rather than towards the rules and guidelines they needed to follow to complete the assignment.
Enjoyment of investigating the claims was found in ‘doing real research into a product to prove its inefficacy’, the real-world application, and selecting the product (‘I really enjoyed getting to pick our own product and doing an assignment that was actually relevant to a real life issue that we could apply to our own lives’). Again, this highlights the transformative nature of integrating uncertainty tolerance teaching and learning opportunities based on real-world data with opportunities to reflect (moderator: critical reflection) on these experiences in supporting uncertainty tolerance development in learners.
Adaptations and Summary
The use of assessments with less prescriptive guidelines (moderator: flexible assessments) can foster uncertainty tolerance. However, such assessments may be perceived negatively by learners who are most familiar with more heavily criterion-based or single-correct answer assessments. These types of activities challenge learners to develop their approaches to work through the task rather than ticking off criteria in a lockstep fashion.
As a means of navigating the uncertainty in the Whack-A-Mole project, learners responded with lists of frequently asked questions and requests for clearer instructions, educator-derived structured timelines, and examples of ‘good work’. We took note of this feedback and attempted to improve the clarity of the facilitation and instructions and to balance the knowns and unknowns for the learners each year the project was delivered. The guide and activity descriptions here are edited versions of the most recent, accounting for the lessons learned through iterative development.
In the course’s third year of delivery, the assessment instructions and marking criteria were identified as requiring improvement. This included ensuring the marking criteria was open enough for learners to express their creativity but not so ambiguous or uncertain that they didn’t know what was expected of them (‘The video could have benefited from a less strict rubric to allow for more creativity’). Consequently, in the following year we made a less strict rubric (moderator: flexible assessments) that encouraged creativity (‘I … loved the creative freedom we were given for our WAM [Whack-A-Mole] videos’). However, it was reported to exacerbate uncertainty (‘The WAM task was great for developing key skills and qualities but the video component was somewhat daunting because of how little direction was provided. I understand that this was supposed to encourage creativity but a little bit more of a structure or some more guidance would make it really great’). We also had an issue with the workload of creating a video (average time 18 hours, ranging from 2 hours - 96 hours, particularly in workload distribution (‘For a video, it’s extremely hard to distribute work evenly’). This was largely attributable to the difficulty in sharing the task of video editing: usually, one team member completed it, but it was the most time-intensive task.
Given persistent issues with the video assessment, we opted to make a change, and learners were subsequently required to create a health promotion campaign, including development of a user profile, advertisement, educational material, and pitch (see below).
The change in the communication format reduced the inequity of the workload driven by video editing but still allowed for creativity (‘I enjoyed … where we were able to creatively present our results, I think the health literacy skills we learned will be important in future’). While learners commented that it was preferable to a video assignment, there were difficulties in establishing the meaningfulness of the task, as it was not strictly scientific (e.g., a lab report). However, including a variety of assessment modes is important, to account for the different strengths and skills of learners and the variety of tasks they could be given in their future careers.
Apply - Communicate Findings to Members of the Community (Health Promotion Campaign Version)
After writing up your report for health experts, you realise that the findings also need to be communicated to members of your community. To do so, as a team, you develop a health promotion campaign for your community targeting the use of your chosen product’s ingredients. In this campaign, you need to identify the target audience, through the development of a user or patient profile, then create educational material and an advertisement that engages the target audience.
Funding for the dissemination of the campaign is tight, so you’ll need to pitch it to the funders to convince them that this is worthwhile budget expenditure, explaining how and why you developed the materials and how you plan to distribute them.
The individual components necessary for your campaign are described in more detail below.
User / Patient Profile
Generating a user or patient profile is a key step in translation of information, but it is often missed. To communicate effectively, we need to know who we are translating the information for; a group you aim to communicate with is often referred to as the target audience. While there are likely many consumers of your complementary or alternative medicine product, for this task, choose just one person to describe for the user profile, who will be representative of the target audience. Information that may be relevant includes the person’s demographics; employment and education; hobbies and interests; and family, friends, and relationships. You may also provide a visual image to represent the user or patient.
Educational Material
In this component, your aim is to transparently communicate the evidence you have found. You can do this for the product as a whole, but concentrating on its key ingredient(s) will avoid defamation of the product’s manufacturer or sponsor and make your campaign relevant to multiple products that contain the same ingredient. The material may take the form of an infographic, fact sheet, or flyer/poster, depending on your identified user or patient and what would be most relevant for them. Make sure you consider their health literacy when developing the material.
Advertisement
Advertising is one of the best ways to ensure your educational materials are seen. Develop one post (including a caption) for a social media platform or one advertisement (e.g., billboard) that could be used to capture the attention of your target audience. The advertisement can be static or dynamic, but it has to be appropriate for your user and the platform.
Pitch
In your final scheduled tutorial class, you will have five minutes plus question time to present your user or patient profile, educational material, and advertisement, and to pitch your campaign. In your pitch, you should do the following:
- Introduce your team and project.
- Show and describe the thinking behind the final products and how they will be disseminated.
- Use visuals, facial expression, pitch, and tone thoughtfully.
As this is a collaborative teamwork project, not all team members need to present the pitch, but the full team can contribute if you prefer. Play to the strengths of all team members when deciding how you will work together on this. The group will need to demonstrate teamwork in responding to questions from peers and facilitators.
Finally, produce a visual representation (e.g., slide), rather like credits in a movie, to show at the end of your pitch identifying what each team member has contributed to the project.
Conclusion
Biomedical science learners applied the principles of evidence-based practice to the Whack-A-Mole project and in doing so altered their perceptions of complementary and alternative medicines and their regulation while navigating many points of uncertainty through the use of creativity and support from facilitators. We found that video provides an exciting platform for assessment, overcoming the limitations of traditional oral presentations, being scalable and sharable, and necessitating the application of creativity, communication, and teamwork skills. However, the requisite skills, the marking of the final product, and the assessment context need to be considered in the adoption and design of video assessments. This project could be used in various healthcare disciplines to teach evidence-based practice.
References
Agency for Healthcare Research and Quality. (2020, November). The patient education materials assessment tool (PEMAT) and user’s guide. https://www.ahrq.gov/health-literacy/patient-education/pemat.html
Albarqouni, L., Hoffmann, T., Straus, S., Olsen, N., Young, T., Ilic, D., Shaneyfelt, T., Haynes, R., Guyatt, G., & Glasziou, P. (2018). Core competencies in evidence-based practice for health professionals: Consensus statement based on a systematic review and Delphi survey. JAMA Network Open, 1(2), Article e180281. https://doi.org/10.1001/jamanetworkopen.2018.0281
Ashford-Rowe, K., Herrington, J., & Brown, C. (2014) Establishing the critical elements that determine authentic assessment. Assessment & Evaluation in Higher Education, 39(2), 205–222. https://doi.org/10.1080/02602938.2013.819566
Australian and New Zealand Clinical Trials Registry. (2024, July 1). Trial search. https://www.anzctr.org.au/TrialSearch.aspx
Fedak, K. M., Bernal, A., Capshaw, Z. A., & Gross, S. (2015). Applying the Bradford Hill criteria in the 21st century: How data integration has changed causal inference in molecular epidemiology. Emerging Themes in Epidemiology, 12, Article 14. https://doi.org/10.1186/s12982-015-0037-4
Howard, B., Diug, B., & Ilic, D. (2022). Methods of teaching evidence-based practice: A systematic review. BMC Medical Education, 22, Article 742. https://doi.org/10.1186/s12909-022-03812-x
PRISMA. (2020). PRISMA flow diagram. https://www.prisma-statement.org/prisma-2020-flow-diagram
Sackett, D. L., Rosenberg, W. M., Gray, J. A., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: What it is and what it isn’t. BMJ, 312, 71–72. https://doi.org/10.1136/bmj.312.7023.71
Therapeutic Goods Act 1989 (Cwlth)
Therapeutic Goods Administration. (2022, June). Listed medicines evidence guidelines: How to demonstrate the efficacy of listed medicines is acceptable (Version 4.0). Department of Health. https://www.tga.gov.au/sites/default/files/evidence-guidelines.pdf
Therapeutic Goods Administration. (2024, July 1). Australian register of therapeutic goods (ARTG). Department of Health and Aged Care. https://www.tga.gov.au/resources/artg
von Conrady, D. M., & Bonney, A. (2017). Patterns of complementary and alternative medicine use and health literacy in general practice patients in urban and regional Australia. Australian Family Physician, 46(5), 315–320.
Media Attributions
- Figure 13.2 Whack-A-Mole project word cloud © Bethany Howard and Basia Diug is licensed under a All Rights Reserved license
An assessment that focusses on the learner applying their knowledge and skills in real-life scenarios or settings.



