6.4 Underpinning theory
Actions required in response to climate change in healthcare are guided by several intertwined theories and models. Overall, these actions follow the basic principles of mitigation, adaptation and resilience in response to climate change. Health systems can undertake mitigation efforts to reduce emissions, adaptation measures for climate change health hazards of, as well as resilience actions (Dresser et al., 2024). These principles must be embedded in health system building, addressing social determinants of health through a complex systems lens (WHO, 2022a, 2022b).
Health system building
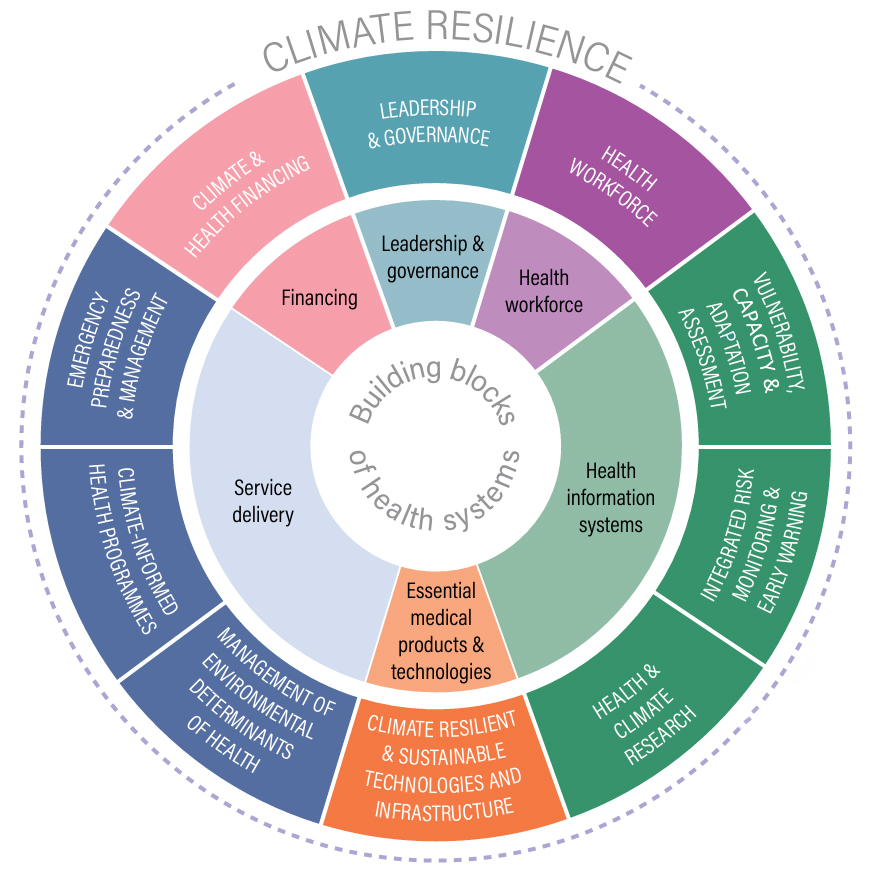
A health system comprises multiple building blocks. According to the World Health Organization (WHO, 2010), these encompass service delivery, health workforce, health information systems, access to essential medicines, and financing and leadership/governance. None should be treated in isolation because they are inherently interconnected. A climate-resilient health system should address all the building blocks (WHO, 2020b, 2022b) (see Figure 6.1).
International system comparisons show that a primary care dominated health system performs better than a hospital-dominated one in population health outcomes (Lawn et al., 2008). From the perspective of climate change, developing a primary care dominated health system is also critical. Hospitals are much larger contributors to greenhouse gas emissions than primary care institutions. In Austria, for example, hospitals account for 32 per cent of CO2 emissions in healthcare, compared to 18 per cent from ambulatory care (Weisz et al., 2020), highlighting the value of primary care dominated systems. Many hospital admissions can be prevented through strengthening primary care. The UK health system has been widely recognised as one of the best in the world: it has one of the lowest hospital discharge rates in OECD countries at 107 per 1,000 of population, compared with 177 in Australia and 209 in Austria (OECD, 2023). The health system in the UK accounts for only 3 per cent of the UK’s carbon emissions (Pichler et al., 2019).
ACTIVITY
Identify one strength and one weakness of your local health system, respectively, in response to climate change regarding each of the five system building blocks:
- Service delivery
- Health workforce
- Health information systems
- Access to essential medicines
- Financing and leadership/governance
Social determinants of health
A range of actions can be taken to mitigate the health risks of climate change, including improving housing conditions (e.g. implementing air conditioning and air filtering systems), enhancing the community environment (by increasing green spaces), optimising service planning and delivery (through early warning systems, resource allocation and ensuring equity in access to care) and fostering cross-sector collaboration (Ebi & Hess, 2024). Many health actions, such as promoting physical activities and encouraging healthy low-carbon diets through green prescribing, can also help reduce emissions (Romanello et al., 2023). These actions align with the social determinants of health framework (Andermann, 2016).
Complex systems theory
A systems approach is needed to ensure the effectiveness of climate actions in healthcare, in which health system and service managers need to champion bold changes and work in partnership with other sectors (Andermann, 2016; Jagals & Ebi, 2021). Health outcomes are considered as a result of ‘a multitude of interdependent elements within a connected whole’ (Rutter et al., 2017). Jagals and Ebi (2021) propose a six-domain framework to guide the development of cross-sectoral sub-competencies and learning content for health workers:
- Climate and environment sciences: factual knowledge about climate change and its key elements
- Drivers of climate change: factual knowledge about the magnitude and pattern of risks
- Evidence, projections and assessments: assessing and using evidence to support decisions
- Iterative risk management: developing comprehensive risk management strategies and plans collaboratively
- Mitigation, adaptation and health co-benefits: advocating actions
- Collective strategies: harnessing international/regional/local agreements and frameworks
This six-domain framework aims to address the gap in existing education and training systems for health professionals. It is deemed essential to prepare health professionals, both those with a clinical-focused role and those with a population/environment-focused role, to ensure that healthcare services can adapt and function effectively, such as ‘to anticipate, respond to, cope with, recover from, and adapt to shocks and stresses’ caused by extreme weather and climate events (Jagals & Ebi, 2021).
ACTIVITY
- Do you know any climate change scientists?
- What conversations have been initiated between the climate change scientists and your local health professionals?
- Do you feel confident that your organisation understands the risks of climate change impacts and is able to conduct proper assessment on the vulnerability of your health facilities?

