Chapter 7 – Align Implementation Strategies
Learning Goals
Use these learning goals to focus your attention, connect new ideas to your own context, and identify practical ways to apply what you learn. In this chapter you can:
- Describe implementation strategies
- Utilise the Behaviour Change Wheel to match intervention functions
- Co-design implementation strategies with stakeholders.
Select the Strategies
Welcome to the second of two chapters designed to help you select implementation strategies to support the planned improvement.
The focus of this chapter is to is to match individuals’ barriers and enablers to theoretically appropriate implementation strategies.
This chapter continues the systematic process of mapping and analysis to generate implementation strategies to support the proposed change.
You will be guided to use your behavioural analysis of individuals’ barriers and enablers for change to identify and map appropriate implementation strategies. This continues the structured process to help influence and support individuals to change their habits, in order to support the proposed improvement.
Introducing Implementation Strategies
When designing for behaviour change, an understanding of how people think, and act can inform strategies that guide people towards better decision making. Further, the systems in which individuals are located actually support their current habits and routines. Therefore, stakeholders within a system are best positioned to understand and influence individuals’ behaviour within their local organisations.
What are Implementation Strategies
Implementation strategies represent the ‘how’ element of change initiatives. They include specific actions that address barriers and leverage enablers, to enhance the application of the evidence and/or the innovation, so that the desired improvements can be achieved. They are designed to facilitate changes in the behaviour of impacted individuals within complex healthcare systems.
Implementation strategies represent the practical application of implementation science. Traditionally, the passive adoption of research evidence took so long that the underlying research was not always up to date. Implementation scientists have demonstrated that when implementation strategies address organisational and individual barriers, they can improve the time and success of integrating research evidence and innovations into clinical practice.
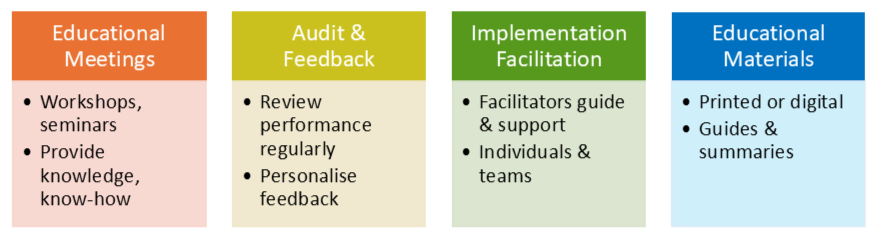
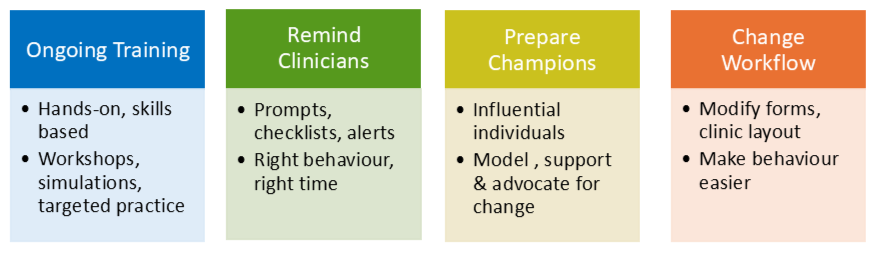
We have already established that knowledge of an innovation or research evidence is insufficient for change. We have acknowledged that health systems influence plans for behavioural change. Therefore, implementation strategies provide the ‘extras’ to directly and practically support behaviour change within dynamic healthcare systems. Several common implementation strategies are described below.
Implementation frameworks and taxonomies
Implementation science researchers have developed many implementation frameworks to address organisational barriers. These frameworks highlight important aspects of organisations for researchers to investigate. Taxonomies of implementation strategies have been developed to match key barriers within organisations. Together, these frameworks and taxonomies provide a range of suggestions for researchers to review.
In this book, a pragmatic approach, informed by systems thinking, behavioural science and stakeholder engagement is proposed. On the one hand, stakeholders’ awareness of their organisational context and its readiness to change, coupled with process and journey maps of the proposed change is important. Ideally, this can be complemented by a deep understanding of key individuals’ barriers and enablers for change. Together, both perspectives can be integrated to identify barriers and enablers to change at organisational and individual levels. These insights provide the basis for choosing appropriate implementation strategies.
A pragmatic approach
The aim of designing implementation strategies is to target barriers and leverage enablers across multiple levels of the healthcare system. Conversations with different stakeholders around process and journey maps can highlight systemic bottlenecks and identify leverage points for change. These broader organisational contextual considerations can be coupled with individuals’ behavioural determinants to facilitate change.
There is both an art and a skill to match behavioural determinants with implementation strategies that are feasible. Every innovation or improvement has unique characteristics that reflect and interact with components of the health system, as well as the individuals who will be administering or receiving the innovation.

-
- Clarify Behavioural Focus
-
- Analyse Behavioural Determinants
-
- Match to Intervention Functions
-
- Select Specific Implementation Strategies
-
- Plan to Monitor and Adapt
Choosing matched implementation strategies brings together all earlier analyses, including identification of key stakeholders, exploration of a specific organisational context and readiness for change and key behavioural barriers and enablers to change. Next, it is useful to utilise the Behaviour Change Wheel to connect behavioural factors with specific implementation strategies.
Introducing the Behaviour Change Wheel
The Behaviour Change Wheel was developed by Susan Michie, Robert West and colleagues at University College, London, from a systematic review of 19 behaviour change frameworks across multiple disciplines in 2011 (see Additional Resources). This tool provides a systematic way of matching implementation strategies to design for behaviour change. The Wheel provides a common language to describe behaviour change across different contexts and health systems.
The Behaviour Change Wheel consists of three layers. The hub of the wheel represents the COM-B model, as previously introduced, as an individual’s Capability, Opportunity and Motivation to do something. [1]
Surrounding this hub is a layer of nine intervention functions: Education, Training, Persuasion, Incentivisation, Modelling, Environmental Restructuring, Restriction, Coercion and Enablement. Each of these represents categories of implementation strategies that influence behaviour. Each intervention function can guide the choice of implementation strategies to support specific behaviour change, based on the underlying determinants of behaviour. Previously identified barriers and enablers to change represent the determinants or factors that affect whether a change occurs. This will be the focus of the remainder of this chapter.
The outer layer of the Behaviour Change Wheel highlights seven policy categories that represent broader elements of healthcare systems. They also represent categories of implementation strategies that focus on change beyond individual organisations. While these categories are seldom the focus for change for small implementation projects within specific healthcare organisations, they can inform community and population health projects.
Nine Intervention Functions
Each intervention function is unique and represents ways to directly target specific barriers and leverage enablers. They are explained, with examples in the following table.
Function |
Description |
Examples |
|
Education |
Increase knowledge, understanding of change |
Briefings, workshops |
|
Training |
Develop skills, competencies, enable practice |
Skills, simulation labs |
|
Persuasion |
Communicate to influence emotions & attitudes to stimulate action |
Testimonials, stories of impact, endorsement |
|
Incentivisation |
Create expectations of reward, acknowledge effort, enhance motivation |
Recognition programs, bonuses, awards |
|
Enablement |
Provide practical support to reduce barriers and increase capability or opportunity |
More staff, simplify, redesign documents & workflows |
|
Modelling |
Provide an example of doing the behaviour for others to aspire to or imitate |
Peer demonstrations, clinical champions, mentoring |
|
Environmental Restructuring |
Change the physical or social context, to make the behaviour easier to do |
Signage, change routines, adjust rosters, prompts |
|
Restriction |
Use rules to reduce opportunity to engage in the target and competing behaviours |
Remove old forms, lock options in, restrict access |
|
Coercion |
Create expectation of punishment or cost Use cautiously and only when required |
Mandatory reporting, compliance checks |
Match Behavioural Determinants to Implementation Strategies
The COM-B model and the Behaviour Change Wheel together provide a matching process from behavioural determinants to implementation strategies. Matching is efficient when barries and enablers are summarised across the 6 components of the COM-B model. This structured approach ensures your implementation strategies are theoretically consistent. There are also common underlying mechanisms of change, which represent the working processes, pathways and events that describe how behaviours change.
Revisit your summary of stakeholders’ perspectives of their barriers and enablers to the proposed change, completed in the previous chapter. Ideally, you have a structured summary of the most important behavioural determinants, organised across the six components of the COM-B model, for each specific group of stakeholders.
From these summaries, map the components of the COM-B model to one or more of the intervention functions from the Behaviour Change Wheel, using the table below.
Behavioural Determinants |
Matching Intervention Functions |
|
|
Physical CAPABILITY Skills, strength, stamina |
Education Training |
Enablement |
|
Psychological CAPABILITY Knowledge, understanding, mental skills |
Training Enablement |
Education |
|
Reflective MOTIVATION Beliefs, intentions, plans, goals |
Education Persuasion Enablement |
Incentivisation Coercion |
|
Automatic MOTIVATION Habits, emotional responses, impulses |
Training Modelling Environmental restructuring |
Persuasion Enablement Coercion Incentivisation |
|
Physical OPPORTUNITY Resources, environment, time |
Training Environmental restructuring |
Enablement Restriction |
|
Social OPPORTUNITY Social norms, supports, influences |
Modelling Persuasion Enablement |
|
This helps narrow the selection of matching implementation strategies. Instead of considering dozens of possible actions, this matching process provides a shortlist of functions that can influence the proposed improvement.
Recognise that some intervention functions map across several COM-B components. It may seem overwhelming to recognise a large number of matched functions. Highlight which intervention functions are recurring. Thus far, this process has happened theoretically, without real consideration of the organisational context within the health system. It is time to bring the theory and practice together!
Reconvene stakeholder groups
It’s time to share these tables and summaries with wider groups of stakeholders, to engage their working knowledge of the local health system. Consider facilitating a session where stakeholders review the COM-B-informed behavioural determinants and check how they match to appropriate intervention functions from the Behaviour Change Wheel. Use visual tools to build shared understanding and allow stakeholders to explore why a particular intervention function fits a given behavioural issue.
Once the matching intervention functions are mutually understood, work with stakeholders to brainstorm and suggest practical implementation strategies. Identify as many strategies as possible, that address the important intervention functions. Specifically, look for implementation strategies to address (remove/reduce) barriers and to leverage enablers. This structured approach ensures your implementation strategies are theoretically matched to the determinants of behaviour. They are more likely to effectively and efficiently influence change.
For example:
- If clinicians aren’t using a new protocol because they don’t understand it → target psychological capability → use education and training.
- If people don’t have time or space to perform a task → target physical opportunity → use environmental restructuring or enablement.
- If motivation is low because clinicians don’t believe the change matters → target reflective motivation → use persuasion and education.
The following table shows how the implementation strategies identified earlier in this chapter, can be developed from behavioural determinants, using COM-B components, which are matched to intervention functions, from the Behaviour Change Wheel. This table offers broad matching sequences, which may vary in different organisational systems.
Ideally, similar tables will be constructed in local health systems to explain how implementation strategies address barriers and leverage enablers to change. It is important for stakeholders to be able to discuss the nuances of behaviour in context, in order to select from the range of intervention functions. Often, a single implementation strategy can incorporate several intervention functions.
Behavioural Determinants |
Intervention Functions |
Implementation Strategy |
|
Psychological Capability (knowledge, understanding) |
Education, Training, Enablement |
Conduct educational meetings |
|
Reflective Motivation (self-efficacy, intentions) |
Persuasion, Incentivisation, Enablement, Education |
Audit and provide feedback |
|
Social Opportunity (peer supports) |
Enablement, Persuasion, Modelling, |
Implementation facilitation |
|
Psychological Capability (knowledge) |
Education, Enablement, |
Distribute educational materials |
|
Physical & Psychological Capability (skills, confidence) |
Training, Enablement |
Provide ongoing training |
|
Automatic Motivation (memory, cues) |
Environmental Restructuring, Training, Modelling |
Remind clinicians |
|
Social Opportunity (peer influence) Reflective Motivation (beliefs) |
Modelling, Enablement, Persuasion, Education |
Identify and prepare champions |
|
Physical Opportunity (resources) |
Enablement, Environmental Restructuring, Restriction |
Change physical structure or workflow |
Identify suitable implementation strategies
Implementation strategies vary in their complexity, from single component strategies to multi-component bundles of approaches. Typically, the complex challenges in healthcare systems require the use of several complementary strategies that address different levels of the healthcare system. Ideally, a range of implementation strategies that focus on individuals, teams and the service or organisation should be identified. However, not all issues can be tackled at once.
Discussion with stakeholders are required to move from having many broadly suitable strategies to selecting bundles of complementary implementation strategies. Systems thinking, together with practical criteria are required. A process of prioritisation is required to identify which behavioural determinants are most important to address, and which implementation strategies are most feasible to actually integrate into regular practice.
It can be helpful to revisit process and journey maps and highlight bottlenecks and leverage points. Encourage discussion around how different barriers and enablers are connected. Enable reflective discussion about what is reinforcing barriers and blocking enablers. Make connections back to key components of the organisational culture and readiness for change.
Stakeholders have a working knowledge of their systems and are able to imagine changes and their possible repercussions. They will be able to suggest practical strategies that are linked with current practice that will target specific barriers. When identifying relevant implementation strategies, discuss and determine ideal patterns and sequences of interactions. Often people focus on removing and reducing barriers, but when enablers are utilised concurrently, the impact can be magnified.
For example, an educational session may backfire if trust is low and the new workflow is uncertain. Empowering local champions to demonstrate how the new workflow fits in can make a difference, especially if the benefits are clear to all involved!
Selection of implementation strategies
When selecting implementation strategies, it is helpful to use the nine intervention functions of the Behaviour Change Wheel as a guide. Each has a place, but their impact is not always equal. There is also an informal hierarchy of effectiveness.
Strategies that rely mainly on education and persuasion, such as information campaigns, can raise knowledge and motivation but often produce only short-lived effects if used alone. In contrast, strategies that reshape the context in which people act, such as environmental restructuring, tend to be more powerful and enduring. These approaches work by changing the default conditions, removing friction from desired behaviours, or making undesirable behaviours harder.
Alongside the intervention functions of the Behaviour Change Wheel, there are other ways of thinking about how to design effective implementation strategies. Three influential approaches have gained traction in healthcare improvement, offering valuable insights.
- Design thinking encourages user-centred, iterative problem-solving, helping strategies to be both practical and acceptable.
- Human factors provides a scientific lens on safety and reliability, reminding us to align systems and environments with human capabilities and limitations.
- Behavioural economics highlights how subtle changes in choice architecture, such as incentives or friction, can nudge behaviour in powerful ways.
Together, these perspectives amplify the functions that go beyond knowledge, making behaviour change more practical within the specific healthcare system. They provide more details about restructuring the environment in which behaviour occurs. Consider that while education can start the conversation about change, design and system-level strategies are usually necessary to make the change ‘easier to do’.
Case Scenario – Encouraging appropriate imaging requests in Emergency Departments
Leaders try to reduce unnecessary imaging by running educational sessions about guideline recommendations. While doctors initially report awareness, behaviour doesn’t shift much. Applying design thinking, the team co-designs a new electronic request form with frontline clinicians. The form includes built-in prompts for guideline criteria, a quick “why not?” option for exceptions, and a hard stop for duplicate requests. This choice architecture nudges clinicians to pause and consider appropriateness, while still leaving flexibility. Education set the stage, but system-level restructuring of the order form makes the right decision easier in the clinical moment.
Co-design bundles of implementation strategies
As implementation strategies are selected, work with stakeholders to combine them into bundles that target different levels of the organisation. Implementation strategies can be designed to dynamically interact within the organisation to capitalise on local priorities and initiatives. A key principle of co-design is that when people contribute to shaping the direction and design of change, they are more likely to support and sustain it.
For example, training to boost capability can be paired with modelling by high power stakeholders (social opportunity) and environmental restructuring of clinical pathways (opportunity) to shift norms and build new workflows.
For each bundle of implementation strategies, ensure there is a clear explanation of how barriers and enablers are being addressed. Practically, it is important to confirm the stakeholders who will authorise and support these strategies. Ensure that there are explicit pathways and processes to underpin this improvement. Use clear language to explain the benefits of using these implementation strategies to address the important problem.
When implementation strategies are carefully documented, their introduction and application can be monitored. Over time, engaged stakeholders design shared ownership of change and communicate with clarity about how and why the chosen implementation strategies will work. This process transforms detailed analysis into action.
When future changes in the system require plans to be altered, an understanding of why the implementation strategies were introduced can be used to make meaningful adaptations to the original plan. Without this detailed justification, problem solving can become random and promised outcomes can be lost. This will be discussed in the next chapter.
Navigate the Paradox Between Fidelity and Flexibility
When planning to implement change, it’s tempting to look for the “best” strategy, for something that has been shown to work and is backed by strong evidence. This is consistent with the concept of fidelity, which refers to maintaining consistency in the core components that make a strategy effective. We have emphasised the importance of fidelity by choosing from theoretically consistent implementation strategies. However, we know that these strategies on their own are not sufficient to drive lasting change. Their success depends on adapting them to fit the local context.
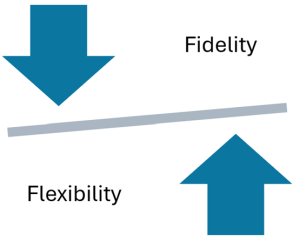
This implementation paradox represents the tension between using proven implementation strategies while adapting them to fit the local context and culture.
The challenge to balance fidelity with flexibility is assisted by engaging stakeholders to co-design feasible bundles of implementation strategies.
Case Scenario: “We introduced the digital platform, but it didn’t help”
Setting:
A community mental health service was struggling to meet the needs of its users.
Challenge:
There were high waiting lists for all services and many users had started to disconnect. Some were heading straight to the emergency department in distress.
Opportunity:
The service was selected to pilot a new digital patient engagement platform designed to support users in managing their mental health. The platform includes practical self-help resources, service information, and access to online coaching. It was developed by a local company in partnership with a regional university and includes strong evidence supporting patient engagement and digital delivery. Maintaining fidelity to its core features is considered crucial for demonstrating impact to users.
Initial Action:
A team leader in the community mental health service was asked to oversee the rollout, using an implementation plan provided by the technology company. She followed the plan, as it had been successful in another similar service. Staff received training, and a simple description was integrated into relevant client files. Many users showed interest and were invited to sign up for a digital orientation process.
One month later, the technology company contacted the team leader to report that very few users had actually engaged with the new platform.
Emerging Tension:
This scenario illustrated the Fidelity vs. Flexibility paradox.
The team leader had focused her time on addressing a litany of staff issues. Several clinicians expressed concern that the platform would replace therapeutic conversations with generic online content. Others worried that many users lacked digital literacy or stable internet access. Some staff were concerned about privacy issues and the use of language that they considered may not feel culturally safe for all service users.
While the digital platform was grounded in research, the local reality didn’t match the original setting. It was time to engage closely with the users to understand their perspective of this platform. Many had picked up on staff concerns, and others were not confident that a digital platform would address their needs. These motivational barriers demanded careful analysis and co-design of suitable implementation strategies.
Turning Point:
A series of co-design workshops with clinicians, staff and users were conducted to discuss barriers and enablers and to flexibly adapt implementation strategies. Together, they navigated the introduction of flexible strategies to inform and onboard users, while also setting up complementary support strategies for staff. They maintained the fidelity of the digital platform while flexibly designing their own implementation strategies.
They shared these experiences with the technology company, which adapted the way they presented implementation plans for other services.
Reflection Questions
- When have you felt tension between following the evidence and meeting the needs of your context?
- Who could help you identify which parts of an implementation strategy are essential, and which can be adapted?
Key Takeaways
1. Implementation strategies are purposeful actions that support behaviour change in context.
Strategies like education, reminders, feedback, and restructuring workflows can be used individually or in combination to address barriers and reinforce enablers. The most effective strategies are selected intentionally, based on a clear understanding of what needs to change and why.
2. The Behaviour Change Wheel helps link behavioural determinants to suitable intervention functions.
Combine the COM-B model to identify what influences behaviour, with the Behaviour Change Wheel to select intervention functions. This creates a logical connection between why change is difficult and how to support it.
3. Co-design implementation strategies with stakeholders to ensure they fit the local organisational context.
Engage stakeholders in prioritising and adapting strategies to ensure they reflect the realities of local practice. Balance maintaining fidelity to the purpose of each implementation strategy with flexible adaptation to the local context.
Additional Resources & Templates
Understanding Implementation Strategies
- This article discusses the importance of implementation strategies in integrating clinical innovations into healthcare settings. It highlights what implementation strategies are, how they are applied to address barriers, and how their impact is evaluated in research.
- This large document provides analyses and findings from a review of implementation strategies for evidence-based practice conducted for the Patient-Centered Outcomes Research Institute (PCORI). It also provides detailed analyses for 20 common implementation strategies.
Understanding the Behaviour Change Wheel
- This 15-minute YouTube video explains how to use COM-B together with a range of intervention options.
The Behaviour Change Wheel website offers clear definitions and examples of all components, alongside a link to buy a source book.
- Come back to this complex and seminal article. Read from the section titled ‘Development of a new framework’ and review Tables 1 and 2. Table 2 describes how the COM-B model has been mapped to the nine functions of the Behaviour Change Wheel. Thankfully, the same researchers have developed both models.
Michie, S., van Stralen, M.M. & West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Sci 6, 42 (2011). https://doi.org/10.1186/1748-5908-6-42. Distributed under the terms of the Creative Commons Attribution Licence (http://creativecommons.org/licenses/by/2.0).
- The Centre for Behaviour Change at University College London also provides many useful resources.
- An integrated approach to using COM-B and the Behaviour Change Wheel
This academic summary walks through the Behaviour Change Wheel and includes 2 useful tables that map intervention functions back to the COM-B (Table 1) and provides examples of behaviour change activities(Table 2) that can inform implementation strategies.
Find out more about design thinking
Find out more about Human Factors
Find out more about Behavioural Economics
Practical case scenarios
- Revisit the article suggested in the previous chapter where researchers developed a mapping guide to link identified barriers to behaviour change theory. See how table 3 summarises barriers to behaviour change organised by capability, opportunity and motivation and suggests appropriate implementation strategies.
- The following editorial in the Journal of Emergency Nursing provides a short summary of how nurses used the COM-B model to understand behaviour, and then identified intervention functions from the Behaviour Change Wheel to create implementation strategies, in busy emergency departments.
Available Templates
Access the templates on the author’s From Research to Reality webpage on the Mosaic website:
- Choose Implementation Strategies
- Co-design Implementation Strategies
- Image source: Michie, S., van Stralen, M.M. & West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Sci 6, 42 (2011). https://doi.org/10.1186/1748-5908-6-42 Available under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0). ↵
Theory-based methods and interventions designed to address barriers and facilitate the adoption and integration of clinical innovations into healthcare settings.
Obstacles or challenges that prevent or hinder successful implementation.
Factors that support or facilitate implementation. Also called Facilitators.
The study of how individuals think, act, and make decisions, especially in social and environmental contexts.
The underlying working processes, pathways, or events that describe how behaviours change.
A participatory and collaborative approach where end users and stakeholders actively shape solutions and ensure they are relevant and feasible.
The degree to which an intervention is delivered as intended by the original developer.

