Thermoregulation
Key Concepts
- Thermoregulation and neutral thermal environment
- Cold stress
- Mechanisms of heat loss and heat production
Temperature Control In-Utero and Transition to Extrauterine Life
In-utero, the fetal temperature is maintained between 37.8- 37.9°C and adapts to the mother’s temperature (Poikilothermic), remaining about 0.3- 0.5°C higher than the maternal temperature as the fetus does not thermoregulate whilst in utero (Todurkar 2022, Kain & Mannix 2003).
Upon birth, the infant’s central and peripheral temperatures begin to vary with the environment, stimulating the infant’s thermoregulatory system to transition from ‘acting’ poikilothermic (relying on the mother’s temperature) (Todurkar 2022, Robins 1997) to homeothermic (self-regulating) (Lyon 2008) typically within hours but possibly up to three days.
If heat loss is not managed at birth an infant’s temperature can drop rapidly by as much as 2-4°C within the first minute (Todurkar 2022), it is important to note that infants are unlike adults and are less able to regulate temperature, thus requiring protection from extremes of heat and cold.
Thermoregulation in the neonate
Management of thermal status is a major aspect of neonatal care as it is critical for survival for both the haemodynamically unstable (unwell) or premature infant in the neonatal nursery, even the healthy term infant is vulnerable to heat loss. The World Health Organization (WHO) recommends that the temperature of newborn infant should be maintained between 36.5–37.5oC after birth (as cited in Dunne et al 2024, Kain & Mannix 2023). Infants that are small or are particularly premature, are at a greater risk of heat loss.
Thermoregulation is the physiological process controlling the balance between heat production and heat loss in the body to maintain “normal” body temperature (Parsons 2014). The maintenance of a “normal” body temperature (normothermia) is balanced by the amount of heat lost from the body with the amount of heat generated from within the body. This process is very limited in the infant and improves with increasing gestational age. Research suggests that hypothermia has been linked to poor outcomes for preterm infants (Dunne et al 2024).
Management should be directed at minimising heat loss to avoid cold stress (discussed further below) response in the infant. Hypothermia can set off a chain of events including increased oxygen requirements (leading to hypoxia if unmanaged) and hypoglycaemia.
Signs & Symptoms of Hypothermia:
- Pale or mottled skin, cool to touch
- Cyanosis of the extremities (acrocyanosis) and or central cyanosis
- Increased oxygen consumption, respiratory distress, apnoea
- Hypoglycaemia
- Poor feeding
- Bradycardia
- Irritability followed by lethargy
- Failure to thrive
(Todurkar 2022)
Cold Stress
Cold Stress is where the infant raises their metabolism in response to hypothermia, this causes vasoconstriction, increased oxygen consumption, which in turn leads to metabolic acidosis from continued vasoconstriction and poor tissue perfusion and oxygenation. Furthermore, pulmonary vasoconstriction and hypoxia from reduced pulmonary perfusion, with compensatory rise in metabolic rate to produce heat (utilises glucose) leading to hypoglycemia. In the pre-term infant, glycogen stores are depleted, oxygen consumption rises with the reliance on anaerobic metabolism to produce heat, this incites metabolic acidosis, pulmonary vasoconstriction, decreasing surfactant secretion and furthering hypoxia (Kain and Mannix 2023, Kyokan et al 2023).
Cold stress triggers a series of responses, such as increase in oxygenation and metabolism, to boost heat production and reduce heat loss, and this can have a significant impact on premature or hemodynamically unstable infant. Two key changes in thermogenesis occur in infants experiencing cold stress: vasoconstriction in the extremities, which helps retain heat in the core, and the activation of brown adipose tissue (BAT) metabolism. BAT (also referred to as brown fat) is concentrated in areas such as the nape and axillae and develops between 26-30 weeks of gestation, making up 2-7% of body weight, the amount of BAT is directly proportional to gestational age (Kain and Mannix 2023). BAT continues to mature for several weeks postnatally, diminishing as the infant grows. Its main role is to undergo oxidisation to generate heat, aiding thermoregulation. In the following image, the brown areas illustrate where brown fat is predominately stored on an infant (Gardner et al 2021, Kain and Mannix 2023). The metabolism of BAT, a process known as non-shivering thermogenesis (NST), sets off a chain of metabolic and chemical reactions, leading to various harmful physiological effects.
Infants generate heat through NST, not shivering thermogenesis, using brown adipose tissue (BAT). This process starts in the hypothalamus and requires glucose and oxygen, however high oxygen demand can lead to complications of hypoxia and metabolic acidosis. Additionally, hypoglycaemia may arise due to the rapid depletion of carbohydrate stores utilised for brown fat metabolism. Heat produced is conducted to the skin via body tissues and blood vessels. Its main role is to undergo oxidization to generate heat, aiding thermoregulation. In the following image, the brown areas illustrate where brown fat is predominately stored on an infant:
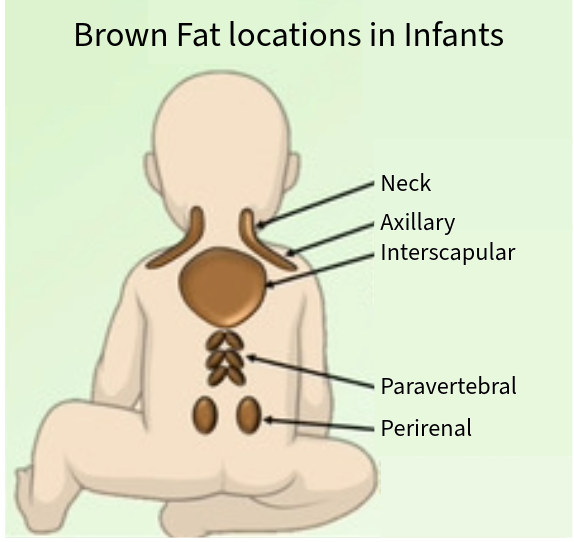 Image adapted from “Figure 1. Adipose tissue function and location” in Nutritional Regulation of Human Brown Adipose Tissue by Karla J. Suchacki and Roland H. Stimson CC BY 4.0
Image adapted from “Figure 1. Adipose tissue function and location” in Nutritional Regulation of Human Brown Adipose Tissue by Karla J. Suchacki and Roland H. Stimson CC BY 4.0
An infant’s responds to cold and metabolic stress occurs through several mechanisms:
- Peripheral Vasoconstriction: to reduce heat loss, causing pallor and cool skin due to decreased blood flow. Increasing respiratory rate, due to pulmonary vasoconstriction related to metabolic acidosis.
- Respiratory Distress Syndrome (RDS): due to decreased surfactant production, leading to hypoxia and acidosis.
- Altered Sleep Patterns and Restlessness: this behaviour prompts muscle movement to generate heat.
- Alternately Lethargy: resulting from reduced cerebral blood flow (CBF), hypoxemia, and hypoglycaemia.
- An initial increase in heart rate: to compensate for central blood volume but later decreases.
- And finally, the skin hardens: primarily on the back and limbs this is known as sclerema.
(Kyokan et al 2023, Dunne et al 2024, Gardner et al 2021, Kain and Mannix 2023).
Metabolic Response to Cold Stress is depicted in the diagram below:
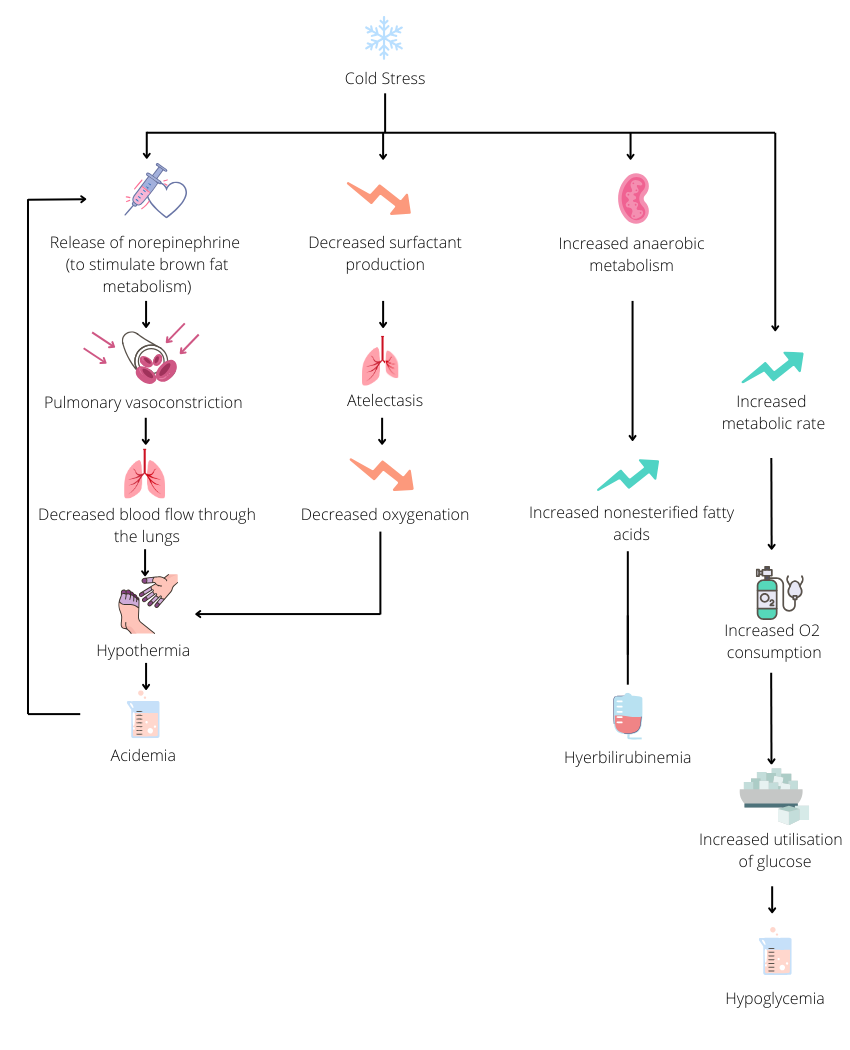
Text Version of Image
Physically infants can react to cold stress by:
- Releasing norepinephrine to stimulate brown fat metabolism leading to pulmonary vasoconstriction, decreased blood flow through the lungs which can result in hypothermia and acidemia cycling back to releasing noropinephrine
- Decreasing surfactant production leading to atelectasis and decreased oxygenation which can result in hypothermia and acidemia cycling back to releasing noropinephrine
- Increased anaerobic metabolism leading to increased nonesterified fatty acids leading to hyperbilirubinemia
- Increased metabolic rate leading to increased oxygen consumption and increased utilisation of glucose leading to hypoglycemia.
End of Text version
Trans-Epidermal Water Loss (TEWL)
TEWL is the insensible loss of water via the from the skin (integumentary) and respiratory systems via diffusion and perspiration. High TEWL results in increased fluid and heat loss in the premature infant, however this can be managed by increasing environmental humidity within the incubator (Lyons 2008, Kain and Mannix 2023).
Key factors influencing TEWL include:
- The water gradient between the skin and the environment.
- Skin permeability.
- Body temperature.
Gestational age is the most critical determinant of TEWL. Research shows that TEWL can decrease by half within the first 13 days of life. Infants born before 25 weeks gestation have more porous skin, making them up to 15 times more susceptible to water loss compared to term infants, which also leads to increased heat loss through evaporation (Dunne et al 2024, Gardner et al 2021, Kain and Mannix 2023).
Goal of Thermoregulation
The primary goal of thermoregulation is to maintain the infants core body temperature around 36.5 – 37.5°C to ensure optimal metabolic and physiological functioning.
Neutral Thermal Environment (NTE)
NTE refers to is the range of ambient temperatures within which the infant can maintain normothermia (36.5 – 37.5oC) with minimal metabolic rate and therefore a minimal oxygen consumption The Neutral Thermal Range (NTR) is a temperature range that is predetermined and dependent on weight, gestation and postnatal age (Lyon 2008, Gardner et al 2021).
Mechanisms of heat loss
There are four mechanisms of heat loss in pre-term infants. These are conduction, convection, evaporation and radiation as shown below:
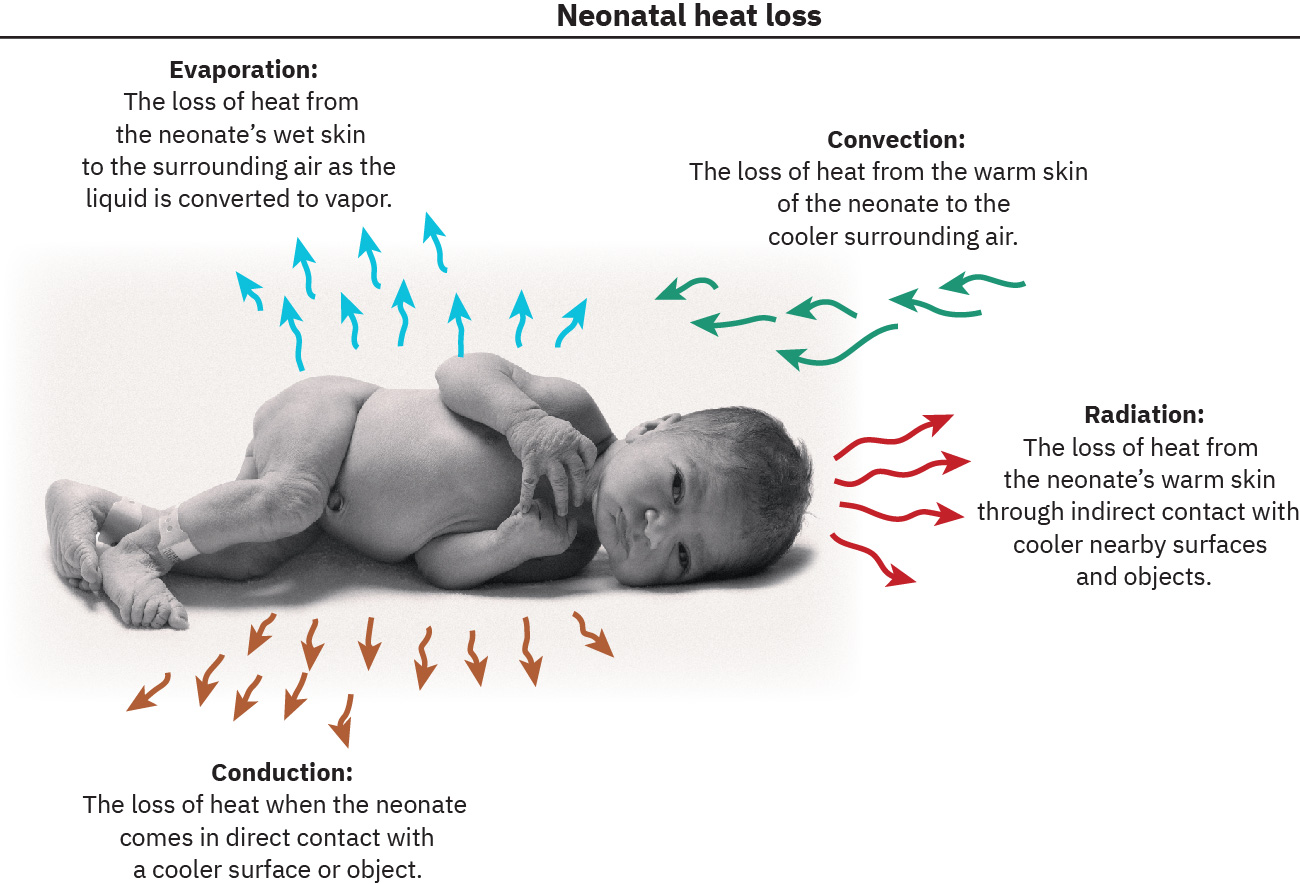
Image Attribution
Neonatal Heat Loss from Maternal-Newborn Nursing by Amy Giles, Regina Prusinski, Laura Wallace OpenStax is licenced under CC BY 4.0
End of Image Attribution
Conduction
Definition: Heat transfer occurs via direct contact between the body and a surface.
Examples of how this occurs: When an infant is placed on cold scales or when a cold stethoscope is applied
Interventions to prevent this:
- Pre-warm incubators and radiant warmers (including gel mattresses)
- Ensure surfaces in contact with the infant (stethoscopes, scales, x-ray plates) are warmed
Convection
Definition: Heat is transferred from the body surface to the surrounding air, with the rate of transfer influenced by the temperature gradient.
Examples of how this occurs: Heat loss occurs in the presence of cool drafts or heat gain occurs when ambient air is warmer than the infant
Interventions to prevent this:
- Cover exposed skin to reduce surface area for heat loss
- Eliminate drafts
- Maintain a warm environment (appropriate nursery or incubator temperature, warm bathwater)
Evaporation
Definition: Heat loss results from the evaporation of moisture on the infant’s body surface. This process is affected by the water vapor gradient between the skin and the surrounding environment.
Examples of how this occurs: The evaporation of amniotic fluid after delivery can lead to significant heat loss or the use of certain forms of respiratory support can increase moisture loss through the respiratory tract.
Interventions to prevent this:
- Utilise a humidification in incubators
- Administer humidified air/oxygen: ensure that any air or oxygen provided is humidified to reduce moisture loss from the respiratory tract.
- Wrap the premature & LBW in a polyethylene bag immediately after delivery
- Place a hat on the infant promptly after birth
Radiation
Definition: Heat is lost through the transfer of radiant energy from the body to surrounding cooler surfaces that are not in direct contact with the infant.
Examples of how this occurs: Nursing the infant in a single-walled incubator in a cooler ambient temperature.
Interventions to prevent this:
- Position the incubator away from walls
- Use double-walled incubators
- Employ radiant warmers as heat sources
(Dunne et al 2024, Todurkar 2022)
In Summary
- Infants can lose heat about four (4) times faster than adults due to their body mass ratio. Large surface area to body mass ratios means there is an imbalance between heat generation (body mass) and heat loss (surface area) Additionally preterm infants have decreased subcutaneous fat, greater body water content and a poorly developed metabolic responses to low temperatures (Todurkar 2022)
- Metabolic response to temperature changes starts developing around 28-30 weeks gestation and thermogenic capacity improves significantly in the initial postnatal days
- Infants in particular preterm infants cannot initiate muscle tone or shiver for heat production. Infants are only able to generate limited heat through activity, often showing restlessness or crying, with non-shivering thermogenesis being the main heat production mechanism (Kain and Mannix 2023)
- Full-term infants tend to adopt a more flexed posture reducing surface area and therefore reducing heat loss, while premature infants struggle to maintain this position and are more vulnerable and are more prone to heat loss due to a higher surface area-to-body mass ratio and minimal subcutaneous fat (Todurkar 2022)
- Conditions like hypoxia or hypoglycaemia can further impair thermogenesis
The aim of maintaining the body temperature between 36.5–37.5oC is to:
- Maximize metabolic efficiency
- Reduce oxygen use
- Reduce calorie expenditure
Test your understanding
References
Çınar, N., and Filiz. T. (2006) Neonatal thermoregulation. Journal of Neonatal Nursing 12(2) 69-74 https://doi.org/10.1016/j.jnn.2006.01.006
Dunne, E., O’Donnell, C., Nakstad, B., and McCarthy, L. (2024) Thermoregulation for the very preterm infants in the delivery room: a narrative review. Paediatric Research. 95(6):1448-1454. https://doi:+10.1038/s41390-023-02902-w.
Gardner, S., Carter, B., Enzman-Hines, M. and Niermeyer, S. (2021) Merenstein and Gardner’s Handbook of Neonatal Intensive Care. 9th Edition. Elsevier.
Kain, V., and Mannix, T. (2023). Neonatal Care for Nurses and Midwives. Principles for Practice. 2nd Edition. Elsevier.
Kyokan, M., Bochaton, N., Jirapaet, V. and Pfister, R. (2023) Early detection of cold stress to prevent hypothermia: A narrative review. SAGE Open Med. doi: 10.1177/20503121231172866
Lyon. A. (2008) Temperature control and the neonate. Paediatrics and Child Health Vol18(4) pages 155-160 https://doi.org/10.1016/j.paed.2007.12.016
Parsons. K. (2014). Human thermal environments: the effects of hot, moderate, and cold environments on human health, comfort and performance. CRC Press. London.
Robins. M (1997) Carbon monoxide and the embryo. PubMed, National Library of medicine https://pubmed.ncbi.nlm.nih.gov/9184336/
Todurkar, N. (2022). Neonatal thermoregulation. Canadian premature baby foundation. https://www.cpbf-fbpc.org/post/neonatal-thermoregulation
Waldron, S., and Mackinnon, R. (2007) Neonatal thermoregulation. Infant 3(3) 101-104 https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=d3de5467d1d0132a9153d3fe0182522b12891ae4
Brown adipose tissue
Trans-epidermal water loss
Neutral thermal environment
Neutral thermal range

