Nutrition and Feeding
Key Concepts
- Feeding options
- Enteral Feeding
- Parenteral Feeding
Infant Feeding
Infant Feeding is critical to their growth, development, and overall health. Feeding choices depend on a variety of reasons such as the gestation of the infant, the feeding tolerance of the infant, and parental choice. Feeding options include breastfeeding, expressed breast milk (EBM), donor breast milk, formula feeding and parental nutrition where is oral feeding in not an option or not able to meet the infants’ nutritional needs.
Infant feeding is important as it provide adequate nutrition to support growth and development while accommodating the infant’s feeding tolerance.
Ensuring proper nutrition is crucial for the growth and development particularly for the premature infant. It is vital for immune function, and recovery, particularly in infants with increased caloric needs. Low blood sugar levels can be indicative of increased metabolic demands (e.g., from hypothermia or hypoxia). Hydration is also a key component of an infant’s overall wellbeing. Whilst IVT provides necessary nutrients if enteral feeding is not possible, however as soon as feasible enteral feeding should be initiated to support gastrointestinal development and function (Gardner et al 2021, Kain and Mannix 2023 Sinha et a 2017)
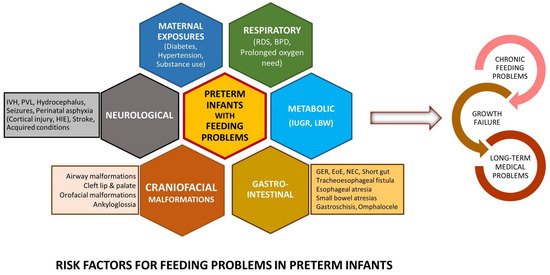
Image Attribution and text description
Image is Figure 1 from Kamity, R., Kapavarapu, P. K., & Chandel, A. (2021). Feeding Problems and Long-Term Outcomes in Preterm Infants—A Systematic Approach to Evaluation and Management. Children, 8(12), 1158. https://doi.org/10.3390/children8121158 licenced CC BY 4.0
Image text description: Image shows risk factors: Common clinical conditions associated with feeding problems in preterm infants. These can be Neurological (IVH: intraventricular hemorrhage, Hydrocephalus, Seizures, Perinatal asphyxia, Cortical injury, HIE, Stroke or acquired conditions), Craniofacial (Airway malformations, cleft lip and palate, Orofacial malformations, Ankyloglossia), Gastrointestinal (GER: gastroesophageal reflux, EoE: eosinophilic esophagitis, NEC, Short gut, Tracheoesophageal fistula, Esophageal atresia, Small bowel atresias, Gastroschisis, Omphalocele), Metabolic (IUGR, Low birth weight), Respiratory (RDS, bronchopulmonary dysplasia, Prolonged oxygen need), or Maternal Exposures (Diabetes, Hypertension, Substance use).
End of Image Attribution and text description
Enteral Feeding
Introduced as tolerated in a hemodynamically stable infant, preterm infants may begin with small volumes of breast milk or formula via nasogastric tube (NGT) or orogastric tube (OGT), gradually increasing as tolerated as per medical advice. Enteral feeding enables the infant to receive optimal nourishment & growth as breastmilk or formula provides the calories needed for the infants to grow and to reach milestones, cell growth, brain growth etc. However, the premature infant less than 34 weeks is still learning to suck, swallow and breathe in a co-ordinated fashion, which follows onto oral fixation, putting hand to mouth and oral exploration. Oral feeding is also a time to interact and bond with the mother, father and other family members, as well as providing emotional development and joy (Gardner et al 2021, Kain and Mannix 2023 Sinha et a 2017)
Research has shown that early and low volume (trophic) feeding can aid in intestinal maturity, and therefore to earlier feed tolerance. It can also lead to earlier full oral feeds (as opposed to IV). Trophic feeding prepares the infant for the next phase in nutrition. The infant develops gastrointestinal sensations of full tummy, leads to being satisfied (hopefully), wake sleep cycles. It aids to prevents allergies (if breast fed), assists in immune system development and prevents later infant and adult diseases, like coeliac disease and diabetes (Gardner et al 2021, Kain and Mannix 2023 Sinha et a 2017)

Baby breastfeeding by David Veksler used under Unsplash licence
Parenteral Feeding
Total Parenteral Nutrition (TPN) is the intravenous delivery of nutrients directly into the bloodstream, bypassing the digestive system. It is typically used when an infant cannot receive adequate nutrition through oral or enteral (tube) feeding.
TPN is used if enteral feeding contraindicated or not tolerated in a hemodynamically unstable infant, adjusting based on laboratory results and clinical needs. Intra venous therapy provides necessary nutrients if enteral feeding is not feasible, while enteral feeding supports gastrointestinal development and function. The administration of total parenteral nutrition, will be prescribed by medical team; mls/kg/day and will depend on infants postnatal age (number of days old). A starting volume on day one is generally 60mg/kg/day to provided adequate calories for an already compromised infant. This will be adjusted based on laboratory results and clinical needs. (Elhassan and Kaiser,2011, Gardner et al 2021, Kain and Mannix 2023 Sinha et a 2017)
Parenteral feeding is usually a temporary solution until the infant can transition to enteral or oral feeding. TPN contains amino acids, glucose, water, electrolytes, trace elements, fats and vitamins for nourishment and growth.
TPN is used :
- If the infant cannot tolerate enteral feeding, administer total parenteral nutrition, adjusting based on laboratory results and clinical needs
- Whenever the enteral route is impossible, inadequate or hazardous because of malformation, disease or immaturity or in the following instances:
- Prematurity: preterm infants (less than 32 weeks) may not have the ability to coordinate/sustain the suck swallow breathe, also may lack the ability digest or absorb nutrients properly.
- Gastrointestinal Disorders: Conditions like necrotizing enterocolitis (NEC), gastroschisis, or intestinal atresia, where the digestive system is compromised.
- Surgical Conditions: Post-operative care for surgeries involving the digestive tract.
- Severe Feeding Intolerance: Inability to tolerate enteral feeding due to severe reflux, vomiting, or other issues.
- Low Birth Weight (LBW) or Very Low Birth Weight (VLBW): These infants may require additional nutritional support to grow adequately.
(Elhassan and Kaiser,2011, Gardner et al 2021, Kain and Mannix 2023 Sinha et a 2017)
In Summary – Nutrition
In the Special Care Nursery (SCN), parenteral feeding provides nutrition intravenously when premature or unwell infants cannot tolerate milk feeds, ensuring essential nutrients are delivered directly into the bloodstream. Enteral feeding, via nasogastric or orogastric tube, begins when the infant’s gut is ready and can include expressed breast milk or formula. Breast milk is preferred due to its immunological and developmental benefits, especially for preterm infants. Feeding is carefully advanced based on the infant’s tolerance, growth, and medical stability. How do we measure the success of feeding – Weight gain (approximately 15-30 grams per day) as well as weekly measuring and plotting of head circumference and length on centile charts.
Infant Feeding Options
Feeding options include breastfeeding, expressed breast milk (EBM), donor breast milk, formula feeding and parental nutrition where is oral feeding in not an option or not able to meet the infants’ nutritional needs.
Explore the various methods of infant feeding below by clicking on the feeding types:

Breast milk by JillWellington used under Pixabay Licence
References
Elhassan, N., and Kaiser, J. (2011). Parenteral Nutrition in the Neonatal Intensive Care Unit. NeoReviews; Vol. 12(3). https://doi.org/10.1542/neo.12-3-e130
Gardner, S., Carter, B., Enzman-Hines, M. and Niermeyer, S. (2021) Merenstein and Gardner’s Handbook of Neonatal Intensive Care. 9th Edition. Elsevier.
Kain, V., and Mannix, T. (2023). Neonatal Care for Nurses and Midwives. Principles for Practice. 2nd Edition. Elsevier.
Sinha, M., Miall, L., and Jardine, L. (2017) Essential Neonatal Medicine. Sixth edition. Wiley and sons
Rizzo, V., Capozza, M., Panza, R., Laforgia, N., and Baldassarre, M. (2022) Macronutrients and Micronutrients in Parenteral Nutrition for Preterm Newborns: A Narrative Review. Nutrients 6;14(7):1530. doi: 10.3390/nu14071530
Intra venous therapy
Hypoxic Ischaemic Encephalopathy
Necrotizing enterocolitis
Intrauterine growth restriction
Respiratory distress syndrome