Development of the respiratory system- overview
Key concepts
- Stages of lung developmental
- Surfactant
Fetal lung development
Development of the lower respiratory tract begins as early as day 28 of gestation. Although fetal lungs do not participate in gas exchange in utero, it is suggested that respiratory-like movements can be detected as early in pregnancy. During this time, the lungs contribute to the production of amniotic fluid and the synthesis of crucial phospholipids required for effective breathing after birth. Premature birth disrupts the normal sequence of lung development, significantly increasing the risk of respiratory distress in the newborn due to immature lung structure and insufficient surfactant production (Kain & Mannix 2023, Gardner et al 2021)
Pulmonary Development in the Fetus
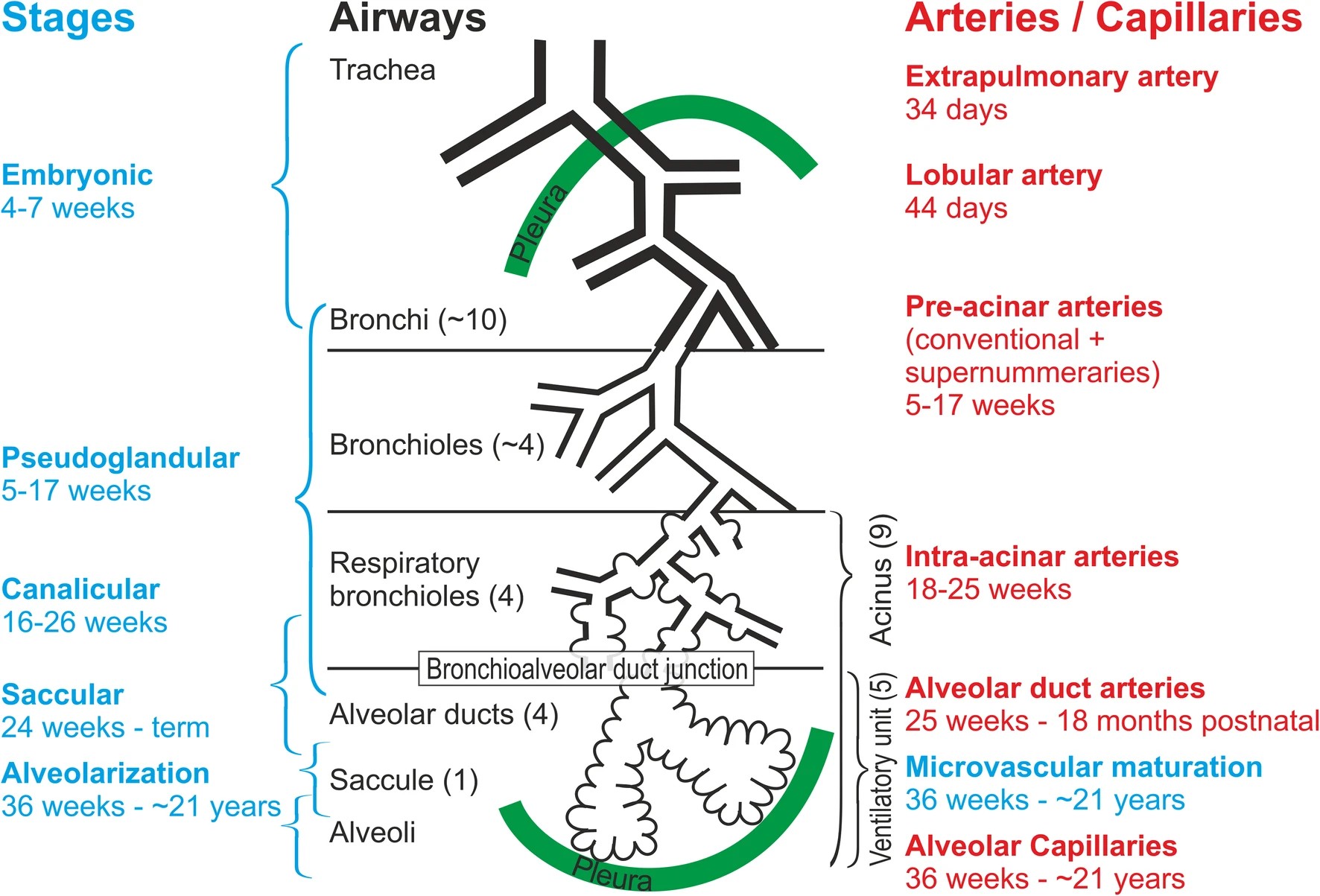
From 28 days of gestation the lungs develop through five stages of lung development: Embryonic (4-7 weeks), Pseudoglandular (5-17 weeks), Canicular (16-26 weeks), Saccular (24 to birth, and Alveolar (36 weeks + into postnatal life), distinct features of these stages are highlighted below.
Image Attribution and Text description
Image Overview of lung development from Schittny, J.C. How high resolution 3-dimensional imaging changes our understanding of postnatal lung development. Histochemistry and Cell Biology 150, 677–691 (2018). https://doi.org/10.1007/s00418-018-1749-7 licenced CC BY 4.0
Image depicts the stages of lung development with images representative of the lung structures developed during each stage.
End of Image Attribution
Role of Pulmonary Surfactant
Surfactant production begins as early as 20-24 weeks (only in small amounts), its role is to decrease surface tension and facilitate alveolar expansion. It is secreted by Type II alveolar cells (or pneumocytes). Within the lungs the alveoli are highly specialised cells. When wet causes a problem of surface tension which is present at any interface between gas and liquid, this can be caused by a lack of pulmonary surfactant within the lungs, which leads to airspaces closing (atelectasis). The amount of surfactant within the lungs is directly proportional to gestational age (Rehman & Bacha 2023).
A deficiency in quality/quantity leads to:
- alveolar collapse on expiration (atelectasis)
- epithelial damage
- development of respiratory distress syndrome (RDS).
(Rehman & Bacha 2023).
In infants born extremely prematurely (before 26 weeks), the lungs often lack sufficient surfactant to support effective ventilation. Pulmonary surfactant plays a crucial role in reducing surface tension within the alveoli, preventing their collapse and allowing the development of functional residual capacity—the volume of air remaining in the alveoli after exhalation. Additionally, surfactant assists in clearing lung fluid after birth and contributes to immune defence through its antimicrobial properties (Graves, 2013).
Transition at birth
The initiation of breathing at birth is triggered by a number of factors such as environmental temperature (generally cooler), tactile stimulation (accoucheur and drying of infant) and changes in partial pressures of oxygen and carbon dioxide during birth (within the lungs). For successful transition from the in-utero environment, three major physiological processes occur, the initiation and sustained regular respiration, fluid-filled air spaces cleared of excess fluid to air-filled for effective gas exchange, and the redirect blood flow towards the fetal lungs and close fetal shunts (Gardner et al 2021 ).
The first breath at birth, liquid is substituted by gas to expand the alveoli. After they are open, a film of surface-active material stabilizes the alveoli (Surfactant). First breath requires high opening pressures, and less pressure is required with each subsequent breath to allow for a similar volume. The effort of breathing is lessened with each subsequent breath, however, without surfactant (or low amounts), alveoli would collapse at the end of expiration, requiring increasing effort with each inspiration to reopen/ force alveoli open (Gardner et al 2021 ).
For further information regarding neonatal transition refer back to chapter one on Transition
Review this chapter
To review of this chapter, watch the following video that summarises fetal lung development:
References
Erickson, E., Bhakta, R., and Mendez, M. (2023) Pediatric Bronchiolitis. National Library of Medicine StatPearls (internet). https://www.ncbi.nlm.nih.gov/books/NBK519506/
Gardner, S., Carter, B., Enzman-Hines, M. and Niermeyer, S. (2021) Merenstein and Gardner’s Handbook of Neonatal Intensive Care. 9th Edition. Elsevier.
Graves, B., (2013) Newborn Transition. Journal of Midwifery and Women’s Health. https://doi.org/10.1111/jmwh.12097
Kain, V., and Mannix, T. (2023). Neonatal Care for Nurses and Midwives. Principles for Practice. Second edition. Elsevier.
Rehman, S. & Bacha, D. (2023) Embryology, Pulmonary. National Library of Medicine. StatPearls (internet). https://www.ncbi.nlm.nih.gov/books/NBK544372/