Neonatal Sepsis
Key Concepts
- Immune system
- Neonatal sepsis
Neonates, especially those born prematurely (less than 28 weeks’ gestation), are particularly vulnerable to sepsis. Factors related to the mother, the neonate, and the environment all contribute to the risk of infection in the neonate. The primary goal is to prevent infections during the perinatal and early newborn period. Neonatal infection can lead to life-threatening sepsis. Neonatal sepsis is a significant cause of mortality and morbidity in infants accounting for 10% of all neonatal mortality. The incidence for neonatal sepsis is 1 – 8 per 1000 live births (Safer Care Victoria 2017). Sepsis may be early-onset (infection arising within 48 hours of birth) or late-onset (infection arising more than 48 hours after birth).
Terminologies
- Infection- any infectious process caused by bacteria, fungal, protozoal or viral agent.
- Sepsis– the clinical condition associated with organisms in blood, CSF or urine.
- Septicaemia– organisms present in blood cultures.
Overview of the Neonatal immune system
Humoral Immunity involves immunoglobulins, also known as antibodies, which are a diverse group of proteins. When B-cells in lymph nodes, the spleen, or other lymphatic tissues encounter antigens, they are activated and begin secreting immunoglobulins. These antibodies play a crucial role in the immune system (Sinha et al 2017). There are five primary classes of immunoglobulins:
|
Immunoglobulin type |
Explanation |
|
Immunoglobulin G (IgG) |
Is the most prevalent immunoglobulin and is essential for combating viruses, bacteria, and toxins. It is distributed widely in tissues and plasma and can be transferred from the mother to the fetus starting at 17 weeks of gestation. By 30 weeks of gestation, an infant has about half the levels of a full-term infant. Infants start producing their own between 4 and 6 months of age. The subclass IgG2 has a relatively short half-life, and is effective against polysaccharide antigens such as E. coli, Group B streptococcus (GBS), and streptococcus pneumoniae. |
|
Immunoglobulin A (IgA) |
Is an early defence against bacteria and viruses, found in saliva, tears, and other mucosal secretions. Does not cross the placenta. It exists in two forms: secretory IgA and serum IgA. Serum IgA is absent at birth but starts to appear around 10 months of age. Secretory IgA is present soon after birth, detectable in tears by 10 to 20 days, and in the intestinal mucosa by 4 weeks. It is also present in breast milk, providing essential protection for preterm infants. |
|
Immunoglobulin E (IgE) |
Is found in respiratory secretions and is involved in allergic reactions. Does not cross the placenta. Infants have low levels. It is synthesised in mucosal tissues and is associated with triggering allergic responses. Appears to have a role in fighting respiratory syncytial virus (RSV), and there may be a connection between RSV and future allergic responses. |
|
Immunoglobulin D (IgD) |
Function is not well understood. |
|
Immunoglobulin M (IgM) |
Is the first antibody produced in response to an infection and is present in the fetus from 30 weeks’ gestation. It plays a major role in fighting gram-negative bacteria. Does not cross the placenta. Elevated levels at birth may indicate a congenital infection. |
(Gardner et al 2021, Kain and Mannix 2023, Sinha et al 2017).
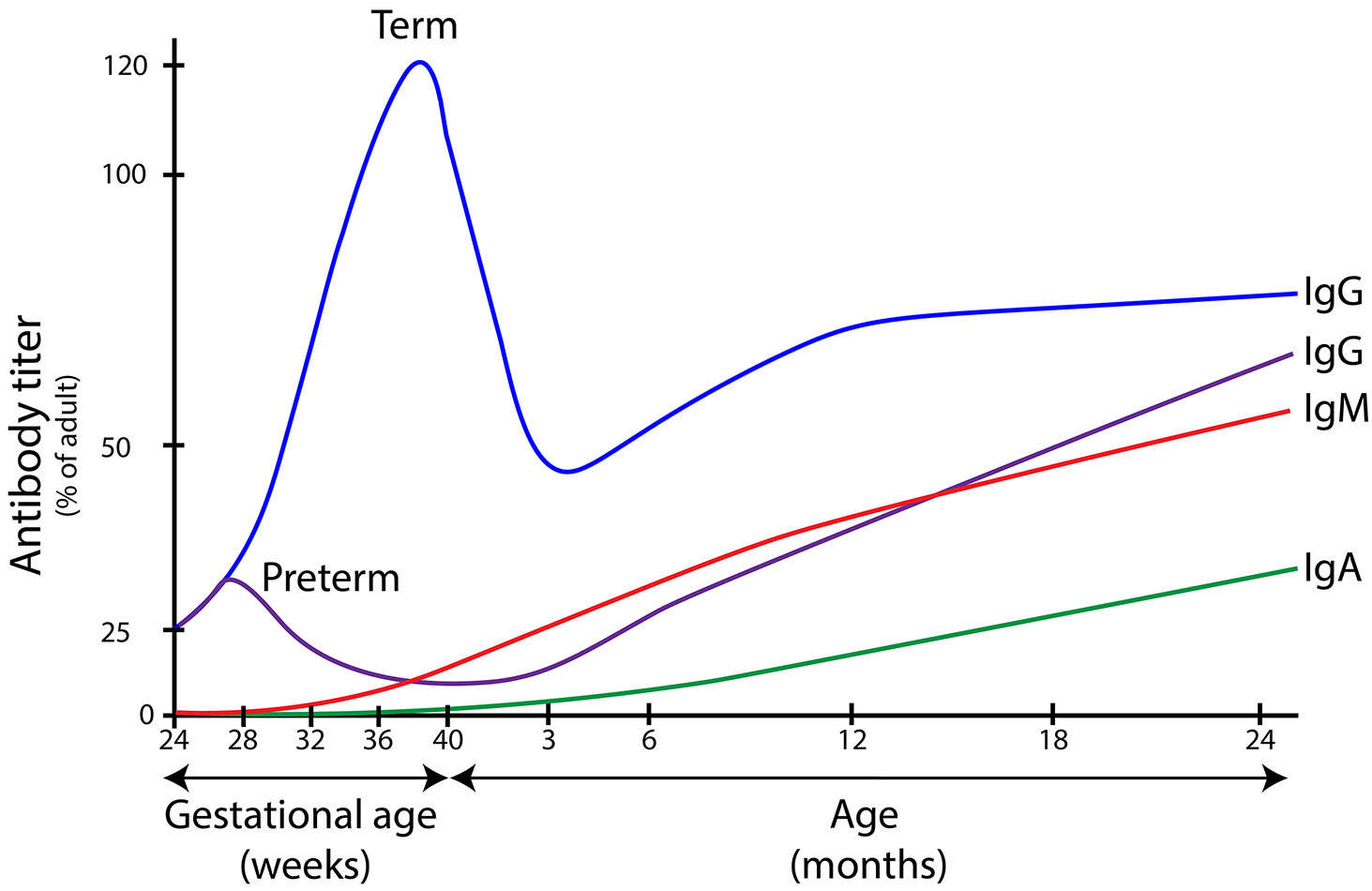
The following diagram gives an idea of the levels of immunoglobulins over time:
Image Attribution and text description
Comparison of Fetal and Neonatal Circulation from Maternal-Newborn Nursing by Amy Giles, Regina Prusinski, Laura Wallace OpenStax is licenced under CC BY 4.0
Image shows that IgG peaks at term before decreasing to 50% of adult antibody titer at 3 months. IgG2 peaks in utero at about 28 weeks gestation, decreasing towards birth and increasing again after birth. IgM commences production about 28 weeks gestation, increasing through birth and subsequent months. IgA is very low at birth increasing slowly over subsequent months.
End of Image Information
Cellular immunity is primarily mediated by T cells, which are activated upon encountering specific antigens. This activation triggers an inflammatory response involving neutrophils, monocytes, and the complement system, all of which work together to establish immune protection. In infants, the response to antigenic stimulation is limited. T cell function may be further impaired by factors such as hyperbilirubinemia, viral infections, corticosteroid therapy, or maternal medications. Neutrophils serve as the first line of defence, and while healthy infants typically have sufficient neutrophil counts, these can drop rapidly during sepsis. Additionally, infants have lower levels of circulating antibodies, and their complement system—a key component of immune defence—is often underdeveloped or functionally suppressed (Kain and Mannix 2023)
Transmission and Predisposing Factors
Infants can acquire infections through:
- Antenatal: Transplacental transmission, vertical transmission via the vagina, premature rupture of membranes (PROM), or uterine infections.
- Intrapartum: Direct contact with vaginal organisms during delivery.
- Postpartum: Horizontal transmission from contact with staff, parents, siblings, equipment, procedures, or through cross-contamination (Gardner et al 2021).
|
Congenital Infections |
Perinatal Infections |
|
Acquired transplacental Pathological organism crosses placenta into fetal circulation
(Gardner et al 2021, Kain and Mannix 2023, Sinha et al 2017). |
Acquired during labour and delivery Infant is exposed to infection through birth canal
|
Preterm infant infection susceptibility
Premature infants are more susceptible to infection because of their immature immune system, immature integumentary system and the need to be cared for in a neonatal nursery. Premature infants have an immature immune response to infection due to the lack of colonisation of resident protective flora, and a reduced ability for the immune system to react and initiate effective inflammatory response. By 30 weeks’ gestation, the infant has half the immunoglobulins of a term infant. The premature infant has a thin, fragile skin, easily that is damaged easily allowing breakdown in barrier to infection. Due to the need for invasive procedures, they are increased risk of infection due to damage to the skin and mucous membranes (Gardner et al 2021, Kain and Mannix 2023, Sinha et al 2017).
Risks for infection include:
|
Maternal/ Intrapartum |
Neonatal |
Environmental |
(Kain and Mannix 2023) |
|
|
Infections can manifest in various ways as shown in the table below:
|
Clinical manifestations: |
|
|
Central Nervous System: |
Generally unwell, fragile, handles poorly, twitching, seizures, poor feeding, bulging fontanelles, high pitched cry, hypotonia or hypertonia, temperature instability (hyperthermia/hypothermia however approximately one third of cases have normal temperature), lethargy, poor tone, poor Moro reflex, irritable, Irregular respiration. |
|
Respiratory System: |
Increased work of breathing, grunting, flaring, accessory muscles, tachypnoea, apnoea, increasing oxygen requirements, cyanosis.
|
|
Cardiovascular System: |
Decreased cardiac output, tachycardia/bradycardia, arrhythmia, murmur, hyper/hypotension, poor peripheral perfusion, cyanosis, mottling/ pallor/ anaemia. Capillary refill greater than 2 seconds, pallor, cyanosis, hypotension, abnormal full blood examination and or coagulation profile, thrombocytopenia, acidosis pH< 7.35, metabolic acidosis unresolved can lead to septic shock. |
|
Gastrointestinal System: |
Poor feeding, vomiting, abdominal distension, bile aspirates, loose stools, hepatomegaly or splenomegaly, delayed gastric emptying (aspirates), carbohydrate intolerance (Guaiac positive stools). |
|
Integumentary System: |
Mottled, rash/ pustules, petechiae, pallor/dusky, jaundice, umbilical stump red/moist/smelly, plus/minus bleeding from puncture sites, co peripheries, or ‘clammy’ skin, cool to touch. |
|
Metabolic System |
Hypoglycaemia – due to inability to compensate overload of microorganisms. Glycosuria (>0.25 mg/m glucose in urine) may be secondary to hyperglycaemia. |
(Gardner et al 2021, Kain and Mannix 2023, Sinha et al 2017).
Prevention of nosocomial infection transmission within the Special Care Nursery
There are various way that nurses and midwives can prevent infection these include:
- Hand Hygiene
- Early screening for at-risk, treat maternal infection intrapartum
- Avoid overhandling (unnecessary handling) of infants
- Monitor temperature instability (high or low)
- Low threshold for screening
- Prophylactic antibiotics -low threshold for suspected sepsis (please refer to below considerations)
- Reduce exposure to pathogens
- Hand hygiene, Personal protective equipment (PPE) aseptic techniques when required
- Proper management of peripheral (remove prior 96 hours or as per local policy) & central lines, VIP score, maintain skin integrity,
- Replace NGT every 5-6 days (or as per hospital policy)
- Promote breastfeeding, or early enteral feeding with breastmilk
- Prophylaxis enteral lactoferrin (a whey protein in human milk – has antimicrobial action, immunomodulatory function, critical in protecting infant from infection)
- Skin integrity measures to prevent pressure injury – cords, change position, interface CPAP, risk screening tools
- Avoid overcrowding of neonatal units, large groups of people/visitors
- Clean equipment between infants (echo machines, x-ray plates)
- Single use equipment (e.g. tapes, stethoscopes, thermometers- not shared between cot spaces)
- Health professionals reduce jewellery (remove rings and bracelets), avoid nail polish – harbour microbes, sleeves above elbows.
- High standards of cleaning, keep bed space clean and uncluttered including no soft/plush toys in cots
- Building standards to ensure good ventilation in nurseries
- Education of parents & staff – stay away if unwell
- Encourage maternal immunisation (flu, COVID, pertussis)
(Gardner et al 2021)
In Summary
Neonatal infections occur within the first 28 days of life. Infections may be acquired during pregnancy, birth, or postnatally and they may affect various organs, leading to conditions like sepsis, pneumonia, or meningitis. They can be caused by bacteria, viruses, fungi, or parasites, with common pathogens including Group B Streptococcus, Escherichia coli, and respiratory viruses. The risk is higher for premature infants, those with low birth weight, and those with weakened immune systems. Early detection and treatment are crucial to reduce the risk of severe complications and death.
Test your understanding
References
Gardner, S., Carter, B., Enzman-Hines, M. and Niermeyer, S. (2021) Merenstein and Gardner’s Handbook of Neonatal Intensive Care. Ninth Edition. Elsevier.
Kain, V., and Mannix, T. (2023). Neonatal Care for Nurses and Midwives. Principles for Practice. Second Edition. Elsevier.
Raymond, S., Stortz, J., Mira, J., Larson, S., Wynn, J., and Moldawer, L. (2017). Immunological Defects in Neonatal Sepsis and Potential Therapeutic Approaches. PubMed 5(13) doi:10.3389/fped.2017.00014
SaferCare Victoria (2017) Sepsis in Neonates. SaferCare Victoria (accessed March 2025) Sepsis in neonates | Safer Care Victoria
Sinha, M., Miall, L., and Jardine, L. (2017) Essential Neonatal Medicine. Fourth edition. Wiley and sons