Engaging with Stakeholders and Partners
Erin Roehrer and Matthew Springer
Learning Outcomes
This chapter will provide HIM leaders with:
- A clear understanding of who the key internal and external stakeholders in HIM are and what their interests and expectations may be.
- Strategies to ensure that all stakeholders are appropriately identified before engaging in any collaboration activities.
- Strategies for effective stakeholder collaboration, engagement, and advocacy to ensure HIM has a strong presence at the decision-making table.
- Insights into how HIM leaders can demonstrate their value proposition to both clinical and non-clinical stakeholders.
- Practical tools and methods for engaging with stakeholders in different organisational contexts.
- Case studies showcasing real-world examples of successful HIM stakeholder engagement.
- Self-assessment activities to help evaluate and refine your own stakeholder engagement strategies.
By the end of this chapter, HIM leaders will have a roadmap for strengthening their influence, securing support for key initiatives, and ensuring HIM remains a central player in the healthcare ecosystem.
Introduction: Why is This Topic Important?
In today’s rapidly evolving healthcare landscape, health information managers and leaders are no longer just record keepers, they are strategic partners in patient care, compliance, and healthcare innovation (Robinson et al 2022, Fenton et al., 2017). Effective stakeholder engagement is critical to ensuring that Health Information Management (HIM) services are valued, supported, and integrated into broader healthcare decision-making processes (Teixeira et al ., 2021).
HIM professionals interact with a diverse range of stakeholders, from clinicians and hospital executives to policymakers, insurers, and patients. Each group has different priorities, expectations, and levels of influence (Petkovic et al., 2023). Failing to effectively engage stakeholders can lead to challenges such as resistance to new technologies, compliance risks, and missed opportunities for HIM leadership to shape the future of healthcare information governance (Serrano et al., 2020).
Why This Matters for HIM Professionals
Traditionally, HIM teams have been seen as back-office support functions, managing patient records, and ensuring regulatory compliance (Fenton et al., 2017). However, as digital health, data governance, and patient-centred care come to the forefront of the success of the health industry, HIM leaders must position themselves as essential contributors to healthcare strategy and decision-making (He et al., 2021; Sheikh et al., 2021).
This means actively building relationships, communicating HIM’s value proposition, and advocating for the role of HIM professionals in improving patient outcomes and operational efficiencies (Isidori et al., 2022). To achieve this, HIM leaders must move beyond transactional relationships and develop long-term engagement strategies that foster collaboration, trust, and influence (Fenton et al., 2017). Without strong engagement, HIM services risk being sidelined in healthcare decision-making.
Background and Context
The Changing Landscape of Health Information Management
HIM has come a long way from the days of paper records and filing cabinets. Today, it sits at the centre of a rapidly evolving healthcare system where digital technologies, data governance, and regulatory compliance shape how information is collected, stored, and used. With the increased presence of electronic health records (EHRs), telehealth, and artificial intelligence in healthcare, HIM professionals are no longer just managing data, they are helping drive strategic decision-making that affects patient care, operational efficiency, and regulatory compliance (Moy et al., 2021).
At the same time, the expectations placed on HIM leaders are higher than ever. Regulatory frameworks such as privacy laws, data protection mandates, artificial intelligence guidance and accreditation standards continue to evolve, requiring HIM professionals to stay ahead of compliance requirements, while also ensuring that health information is accurate, accessible, and secure (Secinaro et al., 2021). This shift means health information management is no longer a background function, and as described by Robinson et al (2022) HIMs are the ‘expert and trusted custodians (of health information)’. They go onto say ‘HIMs face challenges deriving from the multiplicity of the medical record’s contributors and stakeholders. Their governance of privacy in the EMR space extends to system and operational security including sensitivity of system design, aspects of cybersecurity, policies and procedures governing consent to access the record, anonymisation of data (for researchers and governments), standards and directives (Dill et al., 2016; Rezaeibagha et al., 2015 cited in Robinson et al (2022). In short, HIM is a key enabler of safe, effective, and efficient healthcare.
However, this comes with challenges. As technology becomes more complex and interconnected, HIM leaders must navigate competing priorities, organisational resistance to change, and the need for continuous upskilling. The ability to engage effectively with stakeholders, both inside and outside the organisation, has become an essential skill for ensuring HIM remains relevant and influential in shaping the future of healthcare.
Key Internal and External Stakeholders in HIM
Successful HIM leadership is built on strong relationships with a diverse range of stakeholders, each with different priorities and concerns (Segarra-Oña, 2020). Understanding who these stakeholders are, what they care about, and how HIM contributes to their goals is crucial for meaningful collaboration and engagement.
Internal Stakeholders
Within a healthcare organisation, HIM teams work closely with a range of professionals, as outlined below:
- Clinical staff (doctors, nurses, allied health professionals): who rely on accurate patient data for clinical decision-making and patient safety
- Clinical leaders: who drive initiatives dependent on insights from patient data and have a key role in sponsoring HIM initiatives
- Clinical governance: who oversee patient safety and quality monitoring, investigation and improvement
- Administration staff: who enter and manage data related to patient identity, booking and activity
- IT teams: who support the technology infrastructure for EHRs and clinical systems, cybersecurity, and data integration.
- Compliance officers, risk managers and legal counsel: who ensure regulatory and legal standards are met, reducing liability and enhancing data security.
- Hospital executives and administrators: who oversee financial and operational efficiency, requiring data insights to drive decision-making
- Project teams: who require HIM teams’ input to ensure compliance with privacy and data governance requirements
External Stakeholders
HIM professionals also interact with external entities that influence healthcare policies, funding, reporting, and regulations, as outlined below:
- Patients: who are increasingly engaged in their own health data, requiring transparency, access, and security
- Healthcare third parties: who request/access patient data for patient care purposes
- Government and regulatory bodies: who set the rules and frameworks governing health data privacy, interoperability, and reporting
- Accreditation bodies: who ensure healthcare organisations meet quality and compliance standards, often requiring detailed HIM reporting
- Insurers and payers: who depend on accurate coding and documentation for reimbursement and fraud prevention
- Technology vendors: who provide EHRs and EMRs, patient administration and clinical systems, data analytics tools, and AI-driven solutions that must align with HIM workflows, assure confidentiality and meet compliance needs
HIM leaders must bridge the gap between these groups, translating technical and regulatory requirements into meaningful, actionable insights (Low et al., 2019). By building strong stakeholder relationships, HIM professionals can ensure their expertise is recognised, their input is valued, and their role remains central to delivering high-quality, data-driven healthcare.
Engaging with stakeholders is not just about having conversations, it is about knowing who to engage with, how to prioritise stakeholders’ needs, and how to communicate in a way that builds trust and collaboration with stakeholders (Kujala et al., 2022). To achieve this, HIM leaders can lean on a few well-established models that provide guidance on stakeholder management and decision-making.
Theories and Models: What the Evidence Says
Stakeholder Engagement Models
As there is no single approach to engaging with stakeholders; different models help HIM leaders determine who holds influence, how to balance competing interests, and how to align efforts with broader healthcare goals (Kujala et al., 2022).
Mendelow’s Matrix (Power-Interest Matrix) – Who Matters Most?
Not all stakeholders have the same level of influence or interest in HIM initiatives, and that’s where Mendelow’s (1981) matrix comes in handy. This model helps HIM leaders map stakeholders based on two key factors:
- Power – How much authority or influence this stakeholder holds over HIM decisions.
- Interest – How invested is this stakeholder in HIM activities and outcomes.
Using Mendelow’s (1981) matrix, stakeholders fall into four categories:
- High power, high interest (key players) – These are the decision-makers who can make or break HIM initiatives (for example, hospital executives, clinical directors, compliance officers). They require active engagement and strategic communication.
- High power, low interest (keep satisfied) – These stakeholders may not be deeply involved in HIM operations, but they can still influence outcomes (for example, government regulators, consumers of health services). They need periodic updates and reassurance.
- Low power, high interest (keep informed) – These are stakeholders who care about HIM processes but do not have much decision-making power (for example, clinical staff, patients). Providing them with consistent information keeps them engaged.
- Low power, low interest (monitor) – These stakeholders do not need much attention unless their role shifts (for example, certain administrative teams). They require minimal periodic engagement.
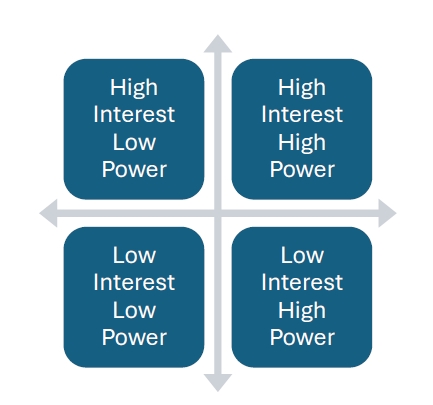
Source: Adapted from matrix in Mendelow (1981).
By understanding stakeholders in this way, HIM leaders can prioritise their time and tailor their engagement strategies to each group’s level of influence and interest.
Freeman’s Stakeholder Theory – Balancing Diverse Needs
Edward Freeman’s Stakeholder Theory (Freeman et al, 2010; Parmar et al, 2010) goes a step further by emphasising that every stakeholder group has a legitimate interest in how an organisation operates. Unlike traditional models that focus solely on shareholders or top decision-makers, this approach reminds HIM professionals that success is not just about meeting executives’ needs—it is also about ensuring patients, staff, and external partners benefit from HIM practices.
In practice, this means:
- Listening to all perspectives – HIM decisions should consider feedback from clinical teams, users of EMR/EHR systems, IT, compliance, and patients when relevant.
- Balancing conflicting priorities – if executives prioritise cost-cutting while clinicians focus on workflow efficiency and patient care, HIM leaders must find solutions that address both concerns.
- Aligning HIM strategies with organisational goals – stakeholder theory reinforces that HIM’s success is linked to the broader success of the healthcare system— whether through better patient outcomes, financial sustainability, or regulatory compliance.
The Quadruple Aim Framework – The Bigger Picture
The Triple Aim Framework (Berwick et al., 2008) developed by the Institute for Healthcare Improvement, is a useful guide for ensuring HIM decisions contribute to healthcare’s ultimate goals. It focuses on three interconnected priorities:
- Better patient care – ensuring data accuracy, security, and accessibility leads to better clinical decision-making and patient safety.
- Improved population health – effective HIM practices contribute to large-scale health insights, enabling better disease prevention and resource allocation.
- Cost efficiency – well-managed health information reduces administrative waste, prevents billing errors, and supports financial sustainability in healthcare organisations.
The Triple Aim Framework was expanded in 2014 to the Quadruple Aim (Lovén et al, 2024) by adding a fourth domain, professional wellbeing or satisfaction of health care workers. This expansion highlights that for quality care to be provided to patients, care must also be provided to those who give it. Burnout in healthcare providers can lower patient satisfaction, increase healthcare costs and reduce overall health outcomes (Bodenheimer & Sinsky, 2014).
By framing HIM’s role within the Quadruple Aim, leaders can clearly demonstrate how HIM initiatives go beyond data management and directly impact the quality, affordability, and effectiveness of healthcare.
Best Practices in Stakeholder Collaboration
Understanding stakeholder theory is one thing—applying it in real-world settings is another. Here are some tried-and-tested best practices that can help HIM leaders engage stakeholders more effectively:
1. Building Trust Through Transparency and Data Integrity
Trust is the foundation of effective collaboration. HIM leaders can strengthen relationships with stakeholders by:
- Ensuring data accuracy – clinicians and administrators rely on precise information for decision-making. Consistently high-quality data builds confidence in HIM processes (Beesley et al, 2020; Sheikh et al, 2021).
- Communicating openly about risks and challenges – whether it is a cybersecurity concern or a new compliance requirement, keeping stakeholders informed (rather than reacting to problems after the fact) fosters trust (He et al, 2021; Petkovic et al, 2023). A good example here is the introduction of electronic medical records. It is important that realistic benefits are shared with stakeholders and functionality and benefits not oversold, leading to disappointment.
- Being a reliable source of truth – HIM professionals must be known for their integrity, presenting unbiased, evidence-based insights that support decision-making (Low et al, 2019; Serrano et al, 2020).
2. Using Evidence-Based Communication to Gain Buy-In
Getting stakeholders to support HIM initiatives often depends on how well the message is framed. Some effective communication strategies include:
- Tailoring the message to the audience – the Chief Financial Officer may want to hear about cost savings, while a clinician may care more about workflow improvements and functionality.
- Using data to tell a compelling story – instead of just presenting raw statistics, translate data into real-world impact (for example, “Improving EHR usability led to a 20% reduction in physician documentation time, allowing more focus on patient care”).
- Anticipating and addressing concerns – stakeholders may resist change. Acknowledge their concerns, provide evidence, and show how the proposed HIM initiative benefits them.
3. Implementing Participatory Decision-Making
One of the best ways to ensure stakeholder buy-in is to involve them early and often. HIM leaders can:
- Seek input during planning stages – rather than presenting a fully developed project for approval, engage stakeholders early to co-create solutions.
- Use stakeholder advisory groups – hold regular meetings with key stakeholders to ensure ongoing dialogue and support.
- Pilot new initiatives before full implementation – testing changes with a small group allows for adjustments before wider rollout, increasing the chances of success.
Bringing It All Together
Stakeholder engagement in HIM is not just about ticking a box, it is about building long-term partnerships that drive better healthcare outcomes. By using established models like Mendelow’s (1981) matrix, stakeholder theory (Freeman et al, 2010), and the quadruple aim (Lovén et al, 2024), HIM leaders can strategically manage relationships, balance competing interests, and align HIM initiatives with broader healthcare goals.
Effective stakeholder engagement is not just about making HIM processes run smoothly, it is about ensuring that HIM actively contributes to a safer, more efficient, and more patient-centred healthcare system (Teixeira et al, 2021).
Activity
Watch this short video, that speaks to the different roles, health information managers can work in. Reflect on the different stakeholders, internal and/or external that these roles would interact with.
Key Implications for Practice
Engaging stakeholders is not just a checkbox activity for HIM professionals—it is a critical strategy for ensuring HIM’s value is recognised, supported, and integrated into broader healthcare decision-making. To achieve this, HIM leaders need to clearly define their value, establish their influence, advocate for change, and use the right tools to engage key stakeholders (Fenton et al, 2017).
Defining the HIM Value Proposition
One of the biggest challenges HIM professionals face is making their contributions visible. While clinical teams are on the front lines delivering care, HIM professionals work behind the scenes ensuring data accuracy, security, compliance, and efficiency, all of which are essential for high-quality healthcare (Fenton et al, 2017). HIMs provide essential value through their expertise in managing health information systems, ensuring data quality, maintaining privacy and security, overseeing clinical documentation, and supporting healthcare delivery through analytics and reporting (HIMAA, 2025). Their role is crucial in maintaining regulatory compliance and facilitating evidence-based decision-making, ultimately contributing to quality healthcare delivery and improved patient outcomes. The key to effective engagement is being able to translate technical expertise into strategic contributions that resonate with decision-makers.
So, what is the HIM value proposition? At its core, HIM enhances patient care, compliance with Standards, Law and compliance, and financial sustainability by ensuring health data are accurate, accessible, and actionable (Teixeira et al, 2021). To make this tangible to stakeholders, HIM leaders should focus on three key messages:
- Better decision-making through high-quality data – HIM professionals provide the foundation for clinical and operational insights by ensuring that health records are complete, accurate, and well-managed (Sheikh et al, 2021; Moy et al, 2021).
- Cost savings and operational efficiencies – proper coding, documentation, and data governance reduce errors, prevent revenue losses, and streamline workflows (Fenton et al, 2017; Teixeira et al, 2021).
- Risk mitigation and compliance – HIM ensures that health organisations meet regulatory requirements, protect patient privacy, and avoid costly penalties (Low et al, 2019; Serrano et al, 2020).
By consistently reinforcing these points, HIM leaders can shift the perception of their role from administrative support to strategic enablers of quality healthcare.
“Having a Seat at the Table” – Ensuring HIM Leadership Influence
For HIM professionals to drive change, they need more than technical expertise, they need visibility, credibility, and influence at the leadership level (Beesley et al., 2020). This means demonstrating HIM’s impact on patient outcomes, financial health, and risk management in ways that resonate with senior decision-makers.
Communicating HIM’s Impact on Patient Outcomes
Accurate health data directly supports clinical decision-making, reducing medical errors and improving care coordination (Sheikh et al, 2021; Moy et al, 2021). Efficient documentation practices enhance continuity of care by ensuring providers have access to complete and up-to-date patient histories (Beesley et al, 2020). Robust data governance ensures patient information remains secure, protecting against breaches and maintaining trust. When HIM leaders frame their contributions in terms of patient safety and quality of care, they create a compelling case for their role in healthcare leadership (Low et al., 2019). Read further about data and data governance in this Chapter Data The Heart of the Healthcare System.
Strengthening Relationships with Senior Leadership
To have a lasting impact, HIM professionals need to actively engage with healthcare clinicians, executives, board members, administrative staff, policy makers and senior administrators (Beesley et al., 2020). Some strategies to build these relationships include:
- Presenting data in decision-making discussions – providing executive teams with insights on risks, safety and quality, operational efficiencies, and financial issues ensures HIM expertise is factored into strategic planning (Sheikh et al, 2021).
- Engaging in hospital committees and advisory groups – having a presence in key meetings ensures HIM perspectives are included in policy development and organisational initiatives (Fenton et al, 2017).
- Proactively addressing challenges – instead of waiting for problems to arise, HIM leaders should anticipate issues, provide data-driven solutions, and position themselves as trusted advisors (Petkovic et al, 2023; He et al, 2021).
Advocacy and Influence Strategies
Beyond internal leadership, HIM professionals also have a role in shaping broader healthcare policies and standards. Advocacy is not just about promoting HIM—it is about ensuring the policies governing healthcare data support better patient care, efficiency, and innovation.
Building Coalitions with Clinical and Administrative Leaders
Advocacy efforts are more effective when HIM leaders collaborate with other influential stakeholders. Some ways to build strategic coalitions include:
- Partnering with directors of medical services, nursing leaders, government policy makers and IT directors to align HIM initiatives with broader organisational goals (Fenton et al, 2017; Freeman et al, 2010).
- Demonstrating how HIM-driven improvements (like better data interoperability or EHR usability enhancements) benefit clinical workflows and patient care (Sheikh et al, 2021; Moy et al, 2021).
- Engaging administrative leaders by linking HIM efficiencies to financial sustainability and regulatory compliance (Teixeira et al, 2021; Low et al, 2019).
Engaging in Policy Development
HIM professionals have a unique perspective on how healthcare regulations impact data management and patient care. To influence healthcare standards, HIM professionals should:
- Participate in professional associations that advocate for HIM policies at national and international levels (Petkovic et al, 2023).
- Contribute to public consultations on data privacy laws, interoperability standards, and reimbursement policies (He et al, 2021).
- Work with legal and compliance teams to ensure health information and other relevant regulations are interpreted and applied in ways that support both compliance and efficiency (Kujala et al, 2022).
Showcasing Data-Driven Improvements
One of the most powerful ways to secure buy-in from stakeholders is by demonstrating measurable results. HIM leaders can:
- Present before-and-after data to demonstrate the impact of HIM initiatives (for example, “Implementing improved documentation standards reduced clinical incidents by 20%”) (Moy et al, 2021; Amer et al, 2022).
- Use case studies and real-world examples to highlight successes in health data governance, patient outcomes, or cost savings (Teixeira et al, 2021; Beesley et al, 2020).
- Continuously measure and report on HIM performance metrics that align with organisational priorities (Kaplan, 1992; Amer et al, 2022).
Tools and Methods for Engagement
Even the best advocacy strategies require the right tools to be effective. HIM leaders should leverage a mix of communication techniques, technology solutions, and feedback mechanisms to engage stakeholders and drive impact.
1. Communication Strategies
- Storytelling with data – presenting health data in a way that tells a compelling story (for example, how improved documentation led to faster patient care).
- Executive summaries – providing leadership with concise, high-impact reports that clearly outline HIM contributions and recommendations.
- Stakeholder workshops – hosting interactive sessions to align HIM initiatives with stakeholder needs and gather valuable feedback.
- Delivering training and education – running or participating on training and education related to health information management, documentation, recording of diagnosis and procedures, use of electronic health record systems.
2. Leveraging Technology
- Dashboards and data visualisation – presenting key HIM and other metrics in clear, interactive formats that make insights accessible to non-technical stakeholders.
- AI-driven analytics – using predictive analytics and machine learning to demonstrate HIM’s role in improving patient outcomes and operational efficiency.
- Enhancing EHR usability – working with IT teams to improve clinician workflows and reduce documentation burden, making HIM processes more integrated and user-friendly.
3. Feedback Mechanisms
- Surveys and stakeholder interviews – regularly collecting input from clinical and administrative teams to refine HIM strategies.
- Advisory committees – establishing dedicated groups that provide ongoing guidance on HIM initiatives.
- Stakeholder mapping exercises – regularly reassessing who holds influence and how engagement strategies should evolve.
Bringing It All Together
For HIM professionals, effective stakeholder engagement is not just about being heard, it is about being a valued and trusted leader in healthcare decision-making. By clearly defining the HIM value proposition, building strategic relationships, using advocacy and influence techniques, and leveraging the right tools and engagement methods, HIM leaders can ensure their expertise drives meaningful improvements in patient care, compliance, and operational efficiency.
Having a seat at the table is not about waiting for an invitation—it is about demonstrating why HIM belongs at the heart of healthcare leadership (Beesley et al., 2020).
Case studies
Stakeholder engagement in HIM is not just a theoretical concept—it plays out in real-world challenges that HIM professionals face every day. The following two cases illustrate how strategic engagement can overcome resistance, drive change, and secure HIM’s role in shaping healthcare policy.
Case 1: Implementing an EHR Change – Engaging Internal Stakeholders
The Challenge: Resistance from Clinicians
A large teaching hospital was preparing to upgrade its EHR system to improve interoperability and streamline documentation. The HIM team identified a major challenge early on: many physicians and nurses resisted the transition, fearing it would disrupt workflows, increase administrative burden, and reduce time spent with patients. Several clinicians voiced concerns that the new system was being implemented without proper consultation and that it could introduce unintended inefficiencies.
Past IT implementations had reinforced this scepticism—previous system updates had caused disruptions, and some users still found workarounds rather than using official documentation processes. The HIM leadership knew that the project was at risk of failure without buy-in from clinicians.
The Solution: Early Involvement and Continuous Training
Recognising that engagement had to start early, the HIM team shifted its approach. Instead of waiting until the system was ready to roll out, they:
- Formed a clinician advisory group early in the process, including doctors, nurses, and allied health professionals to co-design workflows that met both clinical and HIM needs.
- Held interactive workshops and usability testing sessions before the final system configuration, allowing clinicians to voice concerns and propose adjustments.
- Developed a “physician champion” program, enlisting well-respected senior doctors to act as peer mentors and advocates for the change.
- Created a phased training plan, combining hands-on practice, quick-reference guides, and live support teams available on the hospital floor during the transition period.
The Outcome: Increased Adoption and Improved Workflows
The early involvement strategy paid off. Clinicians felt a sense of ownership over the new system because they had been part of the decision-making process. The physician champions helped address scepticism among their peers, and the real-time support teams reduced frustration during go-live.
Within three months of implementation, the hospital saw:
- A 40% reduction in documentation errors compared to the previous system.
- A 20% decrease in time spent on EHR-related administrative tasks due to improved user experience.
- Stronger collaboration between HIM, IT, and clinical teams, leading to smoother updates in the future.
The key takeaway? Stakeholder engagement is not just about communication—it is about co-creation. When HIM leaders actively involve end users, they turn potential resistance into support and shared success.
Case 2: Advocacy for HIM in Policy Development
The Challenge: HIM Leaders Excluded from Policy Discussions
In a national healthcare reform effort , a government task force was developing new data governance regulations to improve privacy protections, interoperability, and patient data access. However, HIM professionals were not initially included in policy discussions—despite their expertise in medical records, compliance, and health data management.
Instead, the task force was primarily composed of policymakers, legal experts, and IT professionals, many of whom had limited knowledge of how data governance decisions would impact clinical workflows and patient care. The HIM community recognised a significant risk: policies might be created that, while well-intentioned, could be difficult to implement or even compromise data integrity and usability.
The Solution: Strategic Advocacy and Policy Engagement
To ensure their voice was heard, HIM leaders took a proactive advocacy approach, focusing on:
- Forming a coalition with professional HIM associations, patient advocacy groups, and healthcare organisations to demonstrate broad industry support for HIM involvement.
- Engaging with policymakers directly, requesting meetings with key decision-makers to explain how data governance affects frontline healthcare operations.
- Presenting case studies from international health systems, showing both the benefits and pitfalls of different policy approaches.
- Securing a role on advisory boards, ensuring that HIM professionals were formally included in the review and decision-making process.
The Outcome: HIM Representation in Health Policy Reforms
Through strategic, data-driven advocacy, HIM professionals were successfully integrated into the policy development process. Their input helped shape regulations in ways that balanced privacy, accessibility, and usability, ensuring that new policies were both effective and practical for healthcare providers.
Key achievements included:
- Standardised HIM-led protocols for implementing privacy and interoperability laws.
- A national HIM advisory committee to provide ongoing guidance on data governance policies.
- Recognition of HIM professionals as essential stakeholders in future healthcare policy initiatives.
The lesson from this case? Advocacy is not just about making noise—it is about demonstrating expertise, building alliances, and showing decision-makers why HIM leadership is essential to shaping the future of healthcare.
Final Thoughts
Both cases highlight the power of proactive engagement. Whether it is leading change within an organisation or advocating at a national policy level, HIM professionals must be strategic, collaborative, and persistent in securing their place at the table.
By leveraging stakeholder engagement models, best practices in communication, and real-world evidence, HIM leaders can ensure that their expertise is recognised—and that their work continues to drive meaningful improvements in healthcare.
Self-Testing Quizzes and Activities
Summary
Success in HIM is not just about maintaining accurate records —it is about having a recognised and valued role in shaping the future of healthcare. As a HIM leader, you will know you have truly made an impact when your expertise is not just acknowledged but actively sought out in decision-making processes.
HIM is Recognised as a Strategic Contributor in Healthcare Decision-Making
One of the clearest signs of success is when HIM is no longer seen as a back-office function, but as an essential part of strategic planning. If senior leadership includes HIM professionals in discussions about digital transformation, patient safety, and healthcare innovation, it is a strong indication that the value of health information is fully understood at the executive level.
Stakeholders Proactively Seek HIM Input on Digital Health Strategies
You know you have built credibility when stakeholders—from clinicians to IT leaders—come to you first when making decisions about EHR optimisation, data analytics, privacy, and interoperability. Instead of HIM teams having to justify their role, they are seen as trusted advisors who help drive digital health initiatives forward.
There is Strong Interdepartmental Collaboration and Trust in HIM Processes
HIM’s success is measured not just in policies and procedures, but in the relationships built across the organisation. When departments trust HIM processes and willingly engage in data-driven decision-making, it is a sign that collaboration is embedded into the culture.
HIM-Led Initiatives Lead to Measurable Improvements in Compliance, Efficiency, and Patient Care
Ultimately, success is measured by impact. If HIM-led initiatives streamline workflows, improve safety and quality, reduce costs, and enhance patient care, then the profession has moved beyond being a support function to being a true driver of healthcare excellence.
References
Beesley, K., McLeod, A., Hewitt, B., & Moczygemba, J. (2020). Health Information management reimagined: Assessing current professional skills and industry demand. Perspectives in Health Information Management, 18 (Winter), 1b. https://pmc.ncbi.nlm.nih.gov/articles/PMC7883363/
Berwick, D., Nolan, T., & Whittington, J. (2008). The triple aim: Care, cost, and quality. Health Aff, 27(3), 759-769. https://doi.org/10.1377/hlthaff.27.3.759
Bodenheimer, T., & Sinsky, C. (2014). From triple to quadruple aim: care of the patient requires care of the provider. The Annals of Family Medicine, 12(6), 573-576. https://doi.org/10.1370/afm.1713
Fenton, S. H., Low, S., Abrams, K. J., & Butler-Henderson, K. (2017). Health information management: changing with time. Yearbook of Medical Informatics, 26(01), 72-77. https://doi.org/10.15265/IY-2017-021
Freeman, R. E., Harrison, J. S., Wicks, A. C., Parmar, B. L., & De Colle, S. (2010). Stakeholder theory: The state of the art. Academy of Management Annals, 4(1), 403-445. https://doi.org/10.5465/19416520.2010.495581
He, W., Zhang, Z. J., & Li, W. (2021). Information technology solutions, challenges, and suggestions for tackling the COVID-19 pandemic. International Journal of Information Management, 57, 102287. https://doi.org/10.1016/j.ijinfomgt.2020.102287
Health Information Management Association of Australia. (2025b). HIMAA Health Information Management Profession Identity Statement. https://www.himaa.org.au/public/169/files/Website%20Document/Our%20Work/Advocacy/HIMAA%20Health%20Information%20Management%20Profession%20Identity%20Statement%20v1_0.pdf
Isidori, V., Diamanti, F., Gios, L., Malfatti, G., Perini, F., Nicolini, A., Bizzarri, G. (2022). Digital technologies and the role of health care professionals: Scoping review exploring nurses’ skills in the digital era and in the light of the COVID-19 pandemic. JMIR Nursing, 5(1), e37631. https://doi.org/10.2196/37631
Kujala, J., Sachs, S., Leinonen, H., Heikkinen, A., & Laude, D. (2022). Stakeholder engagement: Past, present, and future. Business & Society, 61(5), 1136-1196. https://doi.org/10.1177/00076503211066595
Lovén, M., Pitkänen, L. J., Paananen, M., & Torkki, P. (2024). Evidence on bringing specialised care to the primary level—effects on the Quadruple Aim and cost-effectiveness: a systematic review. BMC Health Services Research, 24(1), 2. https://doi.org/10.1186/s12913-023-10159-6
Low, S., Butler-Henderson, K., Nash, R., & Abrams, K. (2019). Leadership development in health information management (HIM): Literature review. Leadership in Health Services, 32(4), 569-583. https://doi.org/10.1108/LHS-11-2018-0057
Mendelow, A. L. (1981). Environmental scanning–the impact of the stakeholder concept. ICIS 1981 Proceedings. 20. https://aisel.aisnet.org/icis1981/20
Moy, A. J., Schwartz, J. M., Chen, R., Sadri, S., Lucas, E., Cato, K. D., & Rossetti, S. C. (2021). Measurement of clinical documentation burden among physicians and nurses using electronic health records: A scoping review. Journal of the American Medical Informatics Association, 28(5), 998-1008. https://doi.org/10.1093/jamia/ocaa325
Parmar, B. L., Freeman, R. E., Harrison, J. S., Wicks, A. C., Purnell, L., & De Colle, S. (2010). Stakeholder theory: The state of the art. The Academy of Management Annals, 4(1), 403-445. https://doi.org/10.5465/19416520.2010.495581
Petkovic, J., Magwood, O., Lytvyn, L., Khabsa, J., Concannon, T. W., Welch, V., Mbuagbaw, L. (2023). Key issues for stakeholder engagement in the development of health and healthcare guidelines. Research Involvement and Engagement, 9(1), 27. https://doi.org/10.1186/s40900-023-00433-6
Robinson K, Barraclough S, Cummings E, Iedema R. The historiography of a profession: The societal and political drivers of the health information management profession in Australia. Health Information Management Journal. 2022;52(2):64-71. doi:10.1177/18333583211070336
Secinaro, S., Calandra, D., Secinaro, A., Muthurangu, V., & Biancone, P. (2021). The role of artificial intelligence in healthcare: a structured literature review. BMC Medical Informatics and Decision Making, 21, 1-23. https://doi.org/10.1186/s12911-021-01488-9
Segarra-Oña, M., Peiró-Signes, Á., & Verma, R. (2020). Fostering innovation through stakeholders’ engagement at the healthcare industry: Tapping the right key. Health Policy, 124(8), 895-901. https://doi.org/10.1016/j.healthpol.2020.05.013
Serrano, A., Garcia-Guzman, J., Xydopoulos, G., & Tarhini, A. (2020). Analysis of barriers to the deployment of health information systems: A stakeholder perspective. Information Systems Frontiers, 22, 455-474. https://doi.org/10.1007/s10796-018-9869-0
Sheikh, A., Anderson, M., Albala, S., Casadei, B., Franklin, B. D., Richards, M., Mossialos, E. (2021). Health information technology and digital innovation for national learning health and care systems. The Lancet Digital Health, 3(6), e383-e396. https://doi.org/10.1016/S2589-7500(21)00005-4
Teixeira, J. C. C., Bernardi, F. A., Lopes Rijo, R. P. C., & Alves, D. (2021). Proposal for a health information management model based on Lean thinking. Procedia Computer Science, 181, 1097-1104. https://doi.org/10.1016/j.procs.2021.01.306
In Australia, we use the term EHR to refer to the longitudinal health records that contain summary information of a person's health information, from cradle to the grave and includes immunisation records, discharge summaries, medications and prescriptions filled, imaging and pathology results. It can be used interchangeably with EMR or electronic medical record.
In other countries it is a term used to describe the digital version of a paper chart. It includes a comprehensive collection of a medical history, such as demographics, progress notes, medications, vital signs, past medical history, laboratory data, and radiology reports from a particular provider (American Medical Association [opens in new tab]).
A digital version of a patient's medical history maintained by healthcare providers, used primarily for documenting diagnoses, treatments and care.

