Electronic Medical and Health Records
Willy Chan; Sheree Lloyd; and Helen Almond
Learning Outcomes
- Understand the health information management considerations for electronic medical records (EMRs)/electronic health records (EHRs) at various levels and their impact on healthcare delivery, consumers, and data management.
- Evaluate the factors in choosing an EMR solution, including functionality, usability, interoperability standards, and resources to make decisions and introduce solutions to enhance healthcare operations.
- Identify the success factors and challenges in the implementation and maturation of EMR/EHR systems.
- Propose solutions to address challenges to EMR/EHR implementation, maximising their value and effectiveness.
Introduction
Electronic medical records (EMRs) and electronic health records (EHRs) represent a significant advancement in the management of health information. Digital records are designed to streamline the collection, storage, retrieval, and sharing of health information, ultimately improving the quality of care. Digital records capture structured and unstructured data and can be analysed to understand health service utilisation, disease, and treatment patterns. This chapter explores the considerations for managing health information through EMRs and EHRs, examining their distinctions, implementation, and impact.
Background and Context
EMRs are foundational to a digitally enabled healthcare system. Organisational EMRs collect vast volumes of data at a very granular level. Countries such as Singapore and Australia have implemented longitudinal health summary records often referred to as EHRs providing vital information across jurisdictions and compiling a lifelong health repository. In Europe, the United Kingdom, and other countries, the term electronic health record refers to clinical records maintained by hospitals, primary care, and aged care providers. In Australia, electronic medical record is used to describe detailed records held by healthcare providers, while electronic health records are a longitudinal digital record accessible by healthcare providers and users.
Healthcare systems that are responsive to health care user needs and preferences can lead to better health outcomes and a more efficient healthcare system (Havana et al., 2023). Digital health solutions such as electronic health and medical records are vital to support the delivery of care at the right time, in the right place and by the appropriate provider. EMRs and EHRs are implemented to support clinicians and healthcare providers to provide seamless and integrated care, and support health care users to achieve improved health outcomes Owens et al cited in (Almond & Mather, 2023). Person-centred service delivery can empower individuals to manage their health, disease, and treatment (Havana et al., 2023). Real-time access to health information enhances decision-making, personalised care, and fosters collaboration between users and providers.
Achieving the United Nations’ Sustainable Development Goals (SDGs), particularly Goal 3: Good Health and Well-Being, requires innovative approaches to improve healthcare delivery, equity, and outcomes on a global scale (United Nations, 2023). Health information systems, particularly EMRs and EHRs, play a central role in supporting these objectives by providing a foundation for data-driven decision-making and resource allocation (Stephen et al., 2024; Vos et al., 2020). These digital tools can facilitate the collection, management, and analysis of health user information, enhancing healthcare operations while tracking progress toward SDG health targets (United Nations, 2023). The chapter on Patient Safety and Sustainable Development Goals Through the Lens of Health Information Management also describes this integral role.
Data from EMRs/EHRs can drive healthcare improvement and performance. Predictive analytics using routinely collected data can enhance healthcare outcomes by identifying trends, optimising resources, and supporting preventive health measures (Canfell, Chan, et al., 2024; Kumar & Suthar, 2024; Obermeyer et al., 2019).
This chapter explores the importance of longitudinal records and data linkage, and the critical factors for successful EMR implementation. The functionality and usability of EMRs, adoption of interoperability standards, and maturity and value of EMR systems are also examined. The goal is to highlight how EMRs can transform healthcare delivery into a more efficient, effective, and person-focused system.
Difference Between EMR and EHR
The introduction touched on the difference between EMRs and EHRs. This differentiation is important. Essentially, EMRs are digital counterparts to traditional paper charts, primarily used to document a person’s diagnosis and treatment history within a single healthcare setting, such as a hospital, community health centre, aged care home, or general practice. EMRs have the potential to streamline clinical workflows, improve record-keeping, and enhance patient care within that specific organisation. In contrast, EHRs are designed to transcend individual care settings by enabling the secure sharing of health information across multiple providers, organisations, and even with healthcare users themselves (McGinn et al., 2012). EHRs serve as a comprehensive, longitudinal health record, capturing data from “cradle to grave” to provide a holistic view of an individual’s health journey over their lifetime. This fundamental distinction highlights the broader, integrative role of EHRs in supporting coordinated care, enhancing healthcare user outcomes, and driving population health initiatives; whereas EMRs remain important for managing care at a local organisational level. Understanding these differences is critical to appreciating their respective contributions to modern healthcare systems and achieving data-driven improvements in care delivery.
Activity Watch and Reflect
This video explains the difference between EMRs and EHRs. Reflect on the benefits of digitised health information. Consider the challenges and barriers of adopting an organisational or national health record.
Health Information Management Considerations for EMRs/EHRs
EMR/EHR systems provide significant benefits for data management, healthcare providers, and consumers. By consolidating healthcare user data, including demographics, medical history, treatments, and outcomes, these systems ensure standardised, real-time data availability for clinical decision-making, resource allocation, and health policy development (Serbanati, 2020). At an institutional level, they can enhance operational efficiency by avoiding repeat diagnostics and medication interactions and improving workflows. For consumers, EMR/EHR systems enable better access to personal health information, fostering greater healthcare user engagement and autonomy in care management (Serbanati, 2020). However, successful implementation requires leadership, change and project management, resource allocation (Abdelhak & Hanken, 2016; Arabi et al., 2022), data security, privacy, governance, and interoperability to maximise their impact across the health ecosystem (Tertulino et al., 2024).
Selecting an appropriate EMR solution is a critical step in enhancing healthcare. This section outlines the key factors that decision-makers must evaluate to ensure the chosen system meets the needs of their healthcare environment.
“People need reasons to change. A case for change is a concise collection of evidence that can be easily communicated to demonstrate the reasons for change and the risks of not changing. Taking the time to develop a convincing case for change is a worthwhile investment as it will help stakeholders clearly understand what, why and how of your project (NSW Agency for Clinical Innovation, 2024)”
Leadership and project and change management are vital for EMR adoption. Effective leadership involves developing a clear vision with realistic goals to gain commitment to the project. Successful EMR implementation requires a leadership team that includes practicing clinicians from all professional streams (Scott et al., 2019), reflecting users’ key role in adoption. Training and support are essential components of implementation. Conducting well-timed training sessions tailored to address the specific needs of staff ensures that all users are adequately prepared to utilise the new system. Continuous technical support provides a safety net as staff adapt to the technology. Workflow redesign is essential to assess and improve existing workflows to integrate the EMR system into daily operations (Scott et al., 2019). This ensures that the new system enhances, rather than disrupts, the efficiency of healthcare delivery (Arabi et al., 2022).
Change management is often neglected during EMR implementation and is key to success. Project management helps to ensure EMR projects are achieved and completed within budget and time frames. Planning for risks and risk management is integral to successful EMR projects.
Financial considerations, such as understanding and managing costs and potential benefits are important in EMR projects. This involves developing a clear business case prior to implementation and careful budgeting and planning to ensure that the implementation is economically viable (Arabi et al., 2022). Resourcing for clinical and other staff to redesign workflows, and deliver training and support to users must be included in project budgets. When adopting EMRs, it is important to allocate additional resources and dedicate time to lead and manage change and complete the tasks required for implementation (Greenhalgh & Abimbola, 2019). The availability of technical infrastructure, funding, and skilled personnel is crucial for the EMR implementation. Without adequate resources, even an advanced EMR system may fail to deliver its full potential (Bostan et al., 2024).
EMR implementation presents opportunities and challenges. Success relies on strong change management strategies, comprehensive training programs, and ongoing stakeholder engagement (Arabi et al., 2022; Scott et al., 2019). Critical challenges include resistance to change, high initial costs, technical barriers, and ensuring data privacy and cybersecurity. Achieving interoperability across fragmented healthcare systems remains a significant hurdle (Kosteniuk et al., 2024).
To successfully implement electronic medical and health records, it is crucial to invest in scalable solutions, particularly in resource-limited settings. This ensures systems can grow with operational demands (Rigby & Ammenwerth, 2016; World Health Organization, 2021). Selecting vendors that promote interoperability is important. Adherence to national and global data exchange standards and encouraging cross-platform integration can create unified health information systems that facilitate seamless data sharing and collaboration (Australian Digital Health Agency, 2023; Kuo & Lee, 2018; Palma, 2022).
Prioritising usability and training is essential to ensuring these systems are user-friendly, and clinicians can be supported to do their work (Lloyd et al., 2021; Lloyd et al., 2024). Through iterative design processes and targeted training programs, healthcare providers can be empowered to use the systems effectively and improve overall efficiency and patient care (Carayon et al., 2021; Tao et al., 2020). Addressing data privacy is also essential. Implementing robust cybersecurity measures, governance frameworks, and legal compliance safeguards against breaches and misuse (Murdoch, 2021; Office of the Australian Information Commissioner, 2023; Ruotsalainen & Blobel, 2020).
Consideration of human factors is essential in the implementation of EMRs. A human factors design focus on the interaction between humans and technology. This consideration ensures that the systems are user-friendly, efficient, and safe. Through understanding human factors, EMR implementation can improve user satisfaction, reduce errors, and enhance overall system performance (Dubé et al., 2025; Kushniruk et al., 2014; Vasquez et al., 2024). Engaging users early in EMR implementation assists in developing solutions that meet healthcare providers and patients’ needs.
Private Sector Considerations
The private health sector faces unique challenges during EMR procurement and implementation processes; for example, private providers lack the size of public health care organisations, which can limit an organisation’s ability to leverage economies of scale during the procurement process. Funding drivers for these projects will differ in the private sector, as the funding will need to be generated from existing revenue streams. The drivers for implementing EMRs can differ for private providers, with a focus on the following:
- Improvements in quality of care. By providing comprehensive and up-to-date patient information, EMRs enable healthcare providers to make more informed and timely decisions (Cahill et al., 2025). Standardised data collection templates (Rowlands et al., 2022) and clinical pathways within EMRs help reduce inconsistencies in patient care, and contribute to safer health care (Australian Commission on Safety and Quality in Healthcare, 2021; Neame et al., 2019). EMRs can alert providers to issues such as drug interactions or allergies, thereby reducing the risk of preventable harm. With access to detailed patient histories and evidence-based guidelines, healthcare providers can tailor treatments to each patient’s specific needs, enhancing the appropriateness of care. EMRs can facilitate better communication between patients and providers, allowing for personalised and consumer-centred care. Data collected through EMRs can be used to monitor patient outcomes and identify areas for quality improvement, leading to continuous enhancements in healthcare delivery (Keasberry et al., 2017; Shaw et al., 2018; Woods et al., 2023).
- Compliance with the Standards for Safety and Quality and to gain accreditation, including the ability to capture clinical indicators and quality data (Australian Commission on Safety and Quality in Healthcare, 2021). Capturing real-time data in the EMR removes the need for workarounds, reducing manual data collection and collation in spreadsheets and other tools. This creates efficiencies and removes the potential for error. Timely data also enable real-time responses.
- Health insurance fund requirements for data on diagnosis, treatment, and costs that could influence contract negotiations and reporting.
- Integrated care models that require healthcare records that encompass the patient journey from inpatient services to in-home and outpatient care post discharge.
The size of private health care organisations may impact the availability of staff to support large scale implementation. Without the scale of public hospitals, a lack of expertise within organisations will influence procurement and implementation processes and increase the need for external support. The lean staffing models that private providers use increase initial implementation costs because external resources will be required to support the process.
Organisations will often seek partnerships with EMR vendors to reduce the initial outlay and leverage vendors’ expert knowledge. The cost of the EMR and the limited funding streams in private hospitals will influence the choice between best of breed, with modules from multiple vendors versus integrated solution from a single vendor. Integrated solutions often require higher initial expenditure as opposed to spreading the expense over time as each module is implemented. The risk of fragmented systems and the requirements for multi-vendor systems integration is often traded for lower cost products.
Addressing these considerations and challenges, EMR/EHR systems can play a transformative role in achieving SDG health-related targets. Through their ability to provide foundational health data, enhance care delivery, and drive policy interventions, these systems contribute to a more sustainable, equitable, and data-driven healthcare future.
Health Information Management at Various Levels
Health information management (HIM) professionals play a pivotal role in leading EMR adoption, ensuring that systems meet user requirements, comply with privacy regulations, and advocate for interoperability at various levels of healthcare delivery. From individual providers to nationwide health systems, each level presents unique challenges and opportunities for HIM practices.
Provider Level
At the provider level, EMRs are used to manage health information within a single setting. EMRs have been implemented in community health centres, primary care practitioner’s offices (GPs, allied health practitioners), and aged and acute care settings. At the provider level, the EMR is the electronic version of the paper chart. Advantages of the EMR are that it can be viewed by more than one healthcare provider at a time in real-time and data can be analysed to understand health trends and patterns of utilisation within the setting. Provider EMRs offer various functionalities, including scheduling, clinical documentation, and prescription and medication management. In the United States, where many EMR vendors have originated, these systems have also been implemented to maximise billing and reimbursement. Provider EMRs have been identified to improve efficiency, reduce errors, and enhance care by providing quick access to health information (Canfell, Woods, et al., 2024; Woods et al., 2023). However, downsides have been identified in the literature, including burnout, data burden, note bloat, and usability (Hettinger et al., 2021; Kaipio et al., 2019; Kushniruk et al., 2014; Lloyd et al., 2021; Lloyd et al., 2024; Melnick et al., 2021; Thomas Craig et al., 2021; Tyllinen et al., 2018).
Case Study and Reflection – Technology in General Practice – Enhancing Patient Care
Background
Dr. Emily Chen is a GP operating a busy clinic. Like many modern healthcare providers, she faces challenges in managing her patients’ records, appointments, and the increasing demand for telehealth consultations. To address these, Dr. Chen has implemented a comprehensive practice management software system.
Problem
Before adopting the software, Dr. Chen’s clinic struggled with:
- Managing paper-based records, leading to inefficiencies and errors.
- High rates of missed appointments due to lack of reminders.
- Complex billing processes requiring manual Medicare claims submissions.
- Difficulty in tracking patient progress for chronic diseases.
Solution
Dr. Chen chose a popular practice management software, to streamline her clinic’s operations. The system offered key functionalities:
- Electronic medical records: Securely store patient data, including medical history, medications, and test results. The solution also seamlessly interfaces external systems (My Health Record, Australia’s EHR for example).
- Appointment scheduling: Enable online booking and send automated reminders.
- Billing integration: Simplify invoicing with Medicare and Worker’s Compensation claims for patients.
- Pathology and imaging integration: Allow seamless ordering and viewing of results.
- Telehealth support: Facilitate virtual consultations with secure video conferencing.
Outcomes
Since implementing practice management software, Dr. Chen’s clinic has seen significant improvements:
- Efficiency gains: Reduced paperwork and faster access to patient information.
- Fewer missed appointments: Automated reminders lowered no-show rates by 25%.
- Improved patient care: Alerts for medication interactions and streamlined test result management enhanced clinical decision-making.
- Revenue management: Integrated billing reduced claim rejections and saved administrative time.
- Better chronic disease management: Data analytics helped track and improve care for patients with long-term conditions.
Key Learning Points
- Software selection: Choosing the right practice management software is critical to meeting specific clinic needs.
- Staff training: Ensuring all staff are well-trained in using the software maximises its potential.
- Integration: Effective integration with Medicare, pathology, and telehealth services enhances both efficiency and patient outcomes.
- Adaptation: Adopting technology helps GPs adapt to the increasing demand for digital healthcare solutions.
Reflection Questions
- How could practice management software improve patient care in other healthcare settings?
- What challenges might clinics face when transitioning to digital systems?
- How can GPs ensure patient data remain secure with electronic health records?
Network Level
At the network level, the summary EHR can facilitate the sharing of health information across multiple providers, improving coordination of care. In New South Wales (NSW), Australia, hospitals within each local health district utilise a unified instance of the EMR (eHealth NSW, 2025). This approach enables seamless sharing of patient information across facilities within the same district.
Regional Level
Regional health information systems share health information across different healthcare providers within a region, enhancing public health monitoring and response. Different approaches have been adopted to address this, with some Australian states moving to a single digital patient record (eHealth NSW, 2025). Tasmania aspires to an EMR that integrates pre-hospital and hospital records (Tasmanian Department of Health, 2022)
Hong Kong Hospital Authority’s EMR, the Clinical Management System serves as a unified platform for managing patient records across all public hospitals (Hong Kong Government, 2020). Complementing this, the Electronic Health Record Sharing System facilitates data sharing between public and private health providers, enabling a patient-centric approach to care (Hong Kong Government, 2020).
National Level
At a national level, summary EHRs support large-scale health information exchanges, enabling comprehensive data analysis for policymaking and research. In a country such as Australia, this means that valuable summary health information can be accessed outside of the consumer’s state of residence and be available when travelling in the event of ill health (Australian Digital Health Agency, 2024).
In the 2021 survey conducted by the Organisation for Economic Co-operation and Development (OCED), several countries reported they had implemented nationwide EHRs including Estonia, Finland, Hungary, and Iceland (Slawomirski et al., 2023).
Longitudinal Records and Data Linkage
Longitudinal records support data collection and the ability to track information over time, providing a comprehensive view of an individual or population’s health. Data linkage involves connecting different data sources to create longitudinal records.
Singapore’s National Electronic Health Record system is designed to create a unified health record for each patient, known as the “One Patient, One Health Record” initiative (Ministry of Health Singapore, 2025). This system allows healthcare providers across the country to access a patient’s summary health record securely and efficiently, ensuring coordinated and patient-centric care (Ministry of Health Singapore, 2025; synapxe). The National Electronic Health Record includes key health information, such as patient demographics, admission and visit history, discharge summaries, lab test results, radiology results, medication history, and records of surgeries or procedures. This centralised repository helps reduce duplicate tests, minimise medical errors, and improve the overall quality of care (Ministry of Health Singapore, 2025; synapxe).
Australia has made large investments in the My Health Record system over many years and is available to all citizens (Australian Digital Health Agency, 2024). The My Health Record is a secure online summary of health information, allowing consumers and their healthcare providers to access and share health information for better coordinated care. It includes personal health summaries, Medicare information, and emergency contacts, with personal control over managing access (Australian Digital Health Agency, 2024).
Activity – Shared Healthcare Records
Web Exploration of Shared Healthcare Records
- Visit Singapore’s digital health platform HealthHub [opens in new tab] and the My Health Record website [opens in new tab]. Navigate these websites to understand how each system works. Look for features such as viewing medical records, managing appointments, and accessing lab results.
- While exploring the websites, take notes on the following:
- Key features of each health record system.
- How patients can access and manage their health information.
- Security measures in place to protect patient data.
Key Features of Each Health Record System
Singapore’s HealthHub
- Appointment management: View, book, reschedule, and cancel medical appointments.
- Lab results: Access lab test results, health screenings, and immunisation records.
- Medication management: Request medication refills or renew prescriptions digitally.
- Family health management: Access and manage health records of loved ones after adding their profiles (Ministry of Health Singapore, 2025).
Australia’s My Health Record
- Shared health summary: Contains an overview of the patient’s health status, including medical history, medications, and allergies.
- Pathology and diagnostic imaging results: Laboratories and imaging providers can upload results directly to the record.
- Specialist letters: Correspondence between specialists and GPs is available.
- Advance care planning: Store advance care directives and other legal documents related to care.
- Medicare and Pharmaceutical Benefit Scheme claims history: Includes claims history for easier review of medications (Australian Digital Health Agency, 2024).
How Patients Can Access and Manage Their Health Information
Singapore’s HealthHub
- Patients can access their health information through the HealthHub website or mobile app.
- They can view their NEHR records, including medications, drug allergies, and laboratory results.
- The app allows patients to see which healthcare institutions have accessed their records and receive notifications when their records are accessed (Ministry of Health Singapore, 2025).
Australia’s My Health Record
- Patients can access their health information online through the My Health Record website or mobile app.
- They can view their medical records, including allergies, medications, immunisations, hospital discharge summaries, and test results.
- Patients can control who views their information by setting access controls and receiving notifications when their record is accessed (Australian Digital Health Agency, 2024).
Security Measures in Place to Protect Patient Data
Singapore’s HealthHub
- Access control: Implementing access control measures to ensure only authorised personnel can access data.
- Data encryption: Encrypting data to protect it from unauthorised access.
- Audit logs: Keeping audit logs to track access to records.
- Regular security updates: Installing software updates promptly to protect against vulnerabilities (Ministry of Health Singapore, 2023).
Australia’s My Health Record
- Firewalls: Using firewalls to block unauthorised access.
- Audit logs: Maintaining audit logs to track access to records.
- Anti-virus scanning: Conducting initial and regular anti-virus scanning of documents uploaded to records.
- System monitoring: Monitoring the system to detect suspicious activity (Australian Digital Health Agency, 2025).
Implementation and Health Information Management Practice
Introducing an EMR system involves key considerations for HIM practice. HIM professionals work to ensure that effective governance of record systems is in place (Kemp et al., 2021). Health information professionals are involved in all phases of EMR acquisition from inception, to development of the business case, to selection of products, and finally, implementation.
Ensuring interoperability and integration with existing systems is critical to avoid data duplication. Establishing reference files for demographic details, disease classification, provider codes, and other key data items ensures consistency and accuracy. Standardised codes and terminologies help avoid errors and discrepancies enabling effective data analytics and reporting. Structured and standardised data formats support trend analysis, performance measurement, audit, data quality assessment, and service improvement. (Abdelhak & Hanken, 2016; Hardy, 2024; Owen et al., 2023).
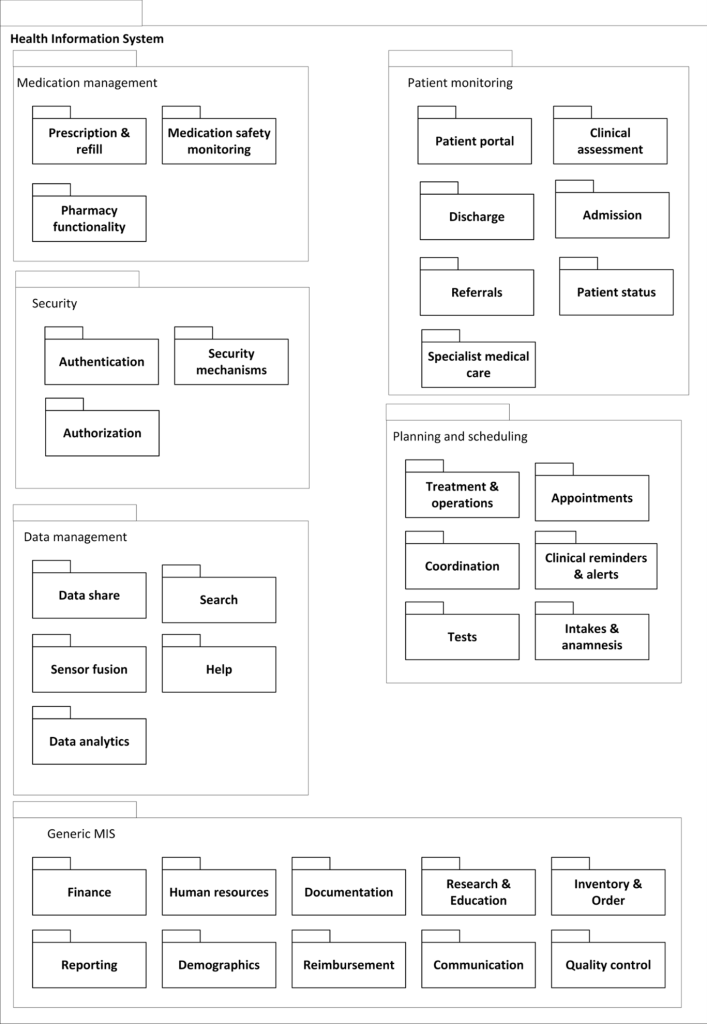
The figure below shows the reference architecture for a health information system and would be tailored to meet reporting and stakeholder requirements (Tummers et al., 2021). This figure provides an example of where reference files may be necessary. Hospitals and general practices should collect data in standardised formats to ensure that the information is comparable and can be aggregated for national health statistics and research. Reference files and data dictionaries are critical requirements for the Australian Institute of Health and Welfare (2025), as they provide standardised terms and protocols for data collection, and maintain consistency across health, community services, and housing sectors, supporting reliable national data collection and reporting, which is essential for informed decision-making and policy development.
HIM professionals are central to data integrity, quality, and accuracy in EMR systems. When entering information into an EMR system, it is important to consider the methods used for data capture and ways to reduce the data collection burden for staff (Sittig et al., 2025). This can be achieved by interfaces between EMR systems and monitoring devices, voice capture, templates, scanning, and the use of bar-codes. Data quality measures help avoid “garbage in, garbage out”, where inaccurate data leads to unreliable and contested outputs.
Protecting consumer and patient information is an essential concern for health information managers and in any EMR or information system implementation. Robust security measures, such as encryption, access controls, and regular security assessments are essential to prevent unauthorised access and data breaches (Boonstra et al., 2014; Sittig et al., 2025). The EMR system and complementary systems like medical imaging and pathology must be able to communicate and exchange data seamlessly with other healthcare systems and providers; while a commitment to standards and their adoption is essential to support continuity of care and comprehensive patient records (Boonstra et al., 2014; Sittig et al., 2025).
Adequate and fit for purpose training and support are vital for effective EMR use, particularly in the highly mobile healthcare workforce (Ting et al., 2021). Continuous education ensures staff and clinicians can leverage new system features and software upgrades. HIM professionals often lead upskilling efforts for professional, administrative, and coding staff.
Compliance with relevant laws and regulations, such as Australia’s Privacy Act and Freedom of Information Act is another critical aspect of EMR implementation (Office of the Australian Information Commissioner, 1982, 1988). HIM professionals ensure proper reporting and adherence to legal requirements. Workflow redesign and effective change management strategies are essential to a smooth transition and to address any resistance from staff during EMR implementation (Boonstra et al., 2014).
Functionality and Usability of EMRs
EMRs are designed to enhance healthcare delivery by digitising information and streamlining workflows. The EMR system’s functionality must support core clinical operations, including healthcare user documentation, decision support, and reporting capabilities. These functionalities are essential for maintaining comprehensive, contemporaneous and accurate clinical records, crucial for effective and safe patient care (Australian Commission on Safety and Quality in Healthcare, 2021; Bhati et al., 2023; Sittig et al., 2025). The table below shows the EMR functionalities that should be considered when purchasing solutions.
| Functionality | Description |
|---|---|
| Clinical Documentation | To capture medical histories and progress notes in a structured searchable format. Supporting unstructured data such as clinical notes (Abdelhak & Hanken, 2016). AI scribes are now being trialled and integrated into EMR systems used in primary and acute sectors (Scott et al., 2021; Scott et al., 2024). To improve legibility of records (Koh & Ahmed, 2021). |
| Order Entry and Referral | To enable clinicians to electronically prescribe medications, order tests, and request referrals (Abdelhak & Hanken, 2016).
To prevent medication errors (Cahill et al., 2025) |
| Decision Support
|
To support leader and manager decision making, safety and quality. Integrated clinical decision support systems provide real-time alerts, reminders and guidance. Real-time data for bed management, discharge planning and operational decision making can be reported to support leaders and managers (Abdelhak & Hanken, 2016). |
| Standards compliance for data sharing
|
To provide support for sharing of data from and with laboratory, radiology, and imaging systems, allowing results to interface directly into the health record for easy review.
To assist data sharing and exchange within and across healthcare settings, supporting continuity of care and collaborative decision-making (Abdelhak & Hanken, 2016; Owen et al., 2023). |
| Patient Portals and Digital Front Door
|
To enable individuals to access their health records, view test results and communicate with providers (Bärkås et al., 2023; Shaw et al., 2018). EMRs can support patient portals through applications that interface to organisational health records and allow individuals to book appointments and schedule telehealth consultations enabling patient empowerment and control. |
Useability Considerations
According to ISO/IEC 9241-11, usability is the degree to which a product or service can be used by specific users to achieve specific goals with effectiveness, efficiency, and satisfaction in a given context of use (International Standards Organisation, 2010). The EMR system must be intuitive and user-friendly to minimise the burden on clinicians and optimise adoption (Lloyd et al., 2021; Lloyd et al., 2024). A system that is difficult to navigate can lead to frustration and decreased efficiency, whereas a user-friendly interface can enhance productivity and satisfaction among healthcare providers (Franks et al., 2024). Interfaces should be learnable and intuitive, enabling users to locate and input information quickly, ensuring ease of navigation. As overloading users with alerts and excessive information can lead to “alert fatigue” (Henry, 2023; Lloyd et al., 2024; Thomas Craig et al., 2021), cognitive load reduction is essential. EMRs must align with clinical workflows, supporting rather than hindering tasks to ensure seamless integration with workflows (Donohue-Ryan et al., 2023; Lloyd et al., 2024). Features such as error-checking algorithms and clear visual layouts help minimise errors and reduce the risk of data entry mistakes. Systems should be accessible across devices, such as desktops, tablets, and mobiles, enabling clinicians to work efficiently from any location.
Usability principles can be applied to improve user experience through appropriately designed user interfaces (Nielsen, 2024). Nielsen’s (2024) usability heuristics are practical rules of thumb when evaluating EMR systems.
Activity Usability Heuristics
Explore Neilsen’s (2024) Usability Heuristics [opens in new tab]
Reflect on the features that should be included in the design of an EMR system to improve user experience in EMR.
Items you might consider include:
The application of Nielsen’s (2024) Usability Heuristics in the design of EMR systems can enhance user experience. These heuristics provide a framework for evaluating and improving the usability of EMR interfaces, which is essential given the complexity and critical nature of healthcare data management.
- Visibility of system status: EMR systems must keep users informed about the status of their actions, such as data entry or retrieval processes. Clear feedback mechanisms, like progress indicators, help reduce uncertainty and enhance user confidence.
- Correlation between the system and the real world: Using familiar medical terminology and conventions in EMR interfaces ensures that healthcare professionals can easily understand and navigate the system. This alignment with real-world practices minimises the learning curve and potential errors.
- User control and freedom: EMR systems should allow users to easily undo or redo actions, providing flexibility and reducing the risk of irreversible errors. This is particularly important in medical settings, where mistakes can have serious consequences.
- Consistency and standards: Consistent design and adherence to established standards across different modules of the EMR system help users predict and understand system behaviour, thereby improving usability and reducing cognitive load.
- Error prevention: Implementing proactive measures to prevent errors, such as validation checks and confirmation dialogues, is vital in EMR systems to ensure data accuracy and patient safety.
- Recognition rather than recall: EMR interfaces should facilitate recognition over recall by providing visible options and actions, reducing the need for users to remember information from one part of the system to another.
- Flexibility and efficiency of use: EMR systems should cater to both novice and expert users by offering shortcuts and customisable workflows, enhancing efficiency and user satisfaction.
- Aesthetic and minimalist design: A clean and uncluttered interface helps users focus on essential tasks without being overwhelmed by unnecessary information, which is critical in high-pressure healthcare environments.
- Help users with errors: Providing clear, actionable error messages and guidance helps users recover from mistakes quickly and effectively, maintaining the integrity of medical records.
- Help and documentation: Comprehensive help resources and documentation should be readily accessible within the EMR system to assist users to resolve issues and understand functionalities.
A positive user experience is essential for widespread user adoption and satisfaction. Responsiveness to user inputs and the ability to customise the EMR to meet specific needs (templates, dashboards) can improve documentation quality (Rowlands et al., 2022; Smelcer et al., 2009). Features to support team-based care and documentation, and flexible documentation methods that complement clinician workflow and reduce documentation burden by reducing duplication have been identified as important (Rowlands et al., 2022). Excessive copying and pasting of text can lead to lengthy, cluttered notes, referred to as “note bloat” (Lloyd et al., 2024). EMRs should encourage concise, meaningful documentation while providing sufficient context (Strudwick et al., 2022) and enhance the patient experience by facilitating communication and transparency. Features like patient portals and shared decision-making tools help achieve this goal (Warren et al., 2019). Incorporating user feedback into system updates ensures that the EMR evolves to meet the changing needs of its users.
Case Study EMR Usability and Nursing Perspectives
Read the paper and reflect on key themes.
Health information practitioners’ involvement in procurement can contribute to the selection of systems that effectively meet end users’ needs in the following ways:
- Including well-defined usability requirements in tendering provides a tangible basis for comparative evaluation (Hettinger et al., 2021; Lloyd et al., 2024; Saari et al., 2024).
- Acknowledging only linear and easily definable use cases may lead to a lack of understanding about the usability of complex systems, such as EMRs.
- Recognising the relevant complexity of each case helps identify and focus on the most significant use cases when determining requirements and constructing usability evaluations for the procurement process.
- Usability practitioners should consider existing IT architecture and appropriate methods for using evaluation tools when defining usability evaluation criteria for the procurement of complex systems (Tyllinen et al., 2018).
Provider Adoption of Standards for Interoperability
Interoperability in health information systems enables the seamless exchange of health data across different systems and organisations and supports healthcare providers to access complete and accurate patient information. This capability also supports public health monitoring and response by facilitating the aggregation and analysis of health data from diverse sources (Kuo & Lee, 2018; Owen et al., 2023).
Interoperability is critical for the effective use of EHRs. Standards such as Health Level 7 (HL7) [opens in new tab]), Fast Healthcare Interoperability Resources (FHIR) [opens in new tab], and Digital Imaging and Communications in Medicine ensure that different systems can communicate and share information seamlessly (Abdelhak & Hanken, 2016). HL7 is a set of international standards for the exchange, integration, sharing, and retrieval of electronic health information (Owen et al., 2023). These standards define how information is packaged and communicated from one party to another, ensuring that different healthcare systems can work together seamlessly (International Standards Organization). FHIR is a standard developed by HL7 and designed to be flexible and easy to implement, using web technologies such as RESTful APIs (REpresentational State Transfer Application Programming Interfaces) , JSON (JavaScript Object Notation), and XML (eXtensible Markup Language) (Gazzarata et al., 2024; International Standards Organization, 2023; Owen et al., 2023). FHIR aims to simplify the implementation process without sacrificing information integrity, making it easier for different healthcare systems to share data and improve patient care (International Standards Organization, 2023).
Several foundational elements are necessary to achieve interoperability. Standardised data formats, such as HL7 and FHIR ensure consistent interpretation and use of data across systems (Gazzarata et al., 2024). Semantic interoperability, which involves using common data models and coding systems like SNOMED CT and ICD, preserves the meaning of data when exchanged between systems (Owen et al., 2023). Additionally, robust technical infrastructure, including Application Programming Interfaces (APIs) and secure data exchange protocols, is essential for facilitating data transfer(Owen et al., 2023).
Strong data governance and security measures are also critical to protect patient privacy and ensure compliance with legislation and regulations (Smallwood, 2018). Organisational commitment and supportive policies are required to promote data sharing and collaboration among stakeholders. By establishing these foundations, healthcare systems can achieve high levels of interoperability, leading to improved patient care, operational efficiency, and public health outcomes (Owen et al., 2023).
Adoption of Electronic Medical Records
Implementing an EMR system should be approached like any project. This means that the EMR project should have clear objectives, budgets, timeframes, and deliverables. EMR and other digital solutions and deployment of technology can be challenging, although significant improvement has been noted in recent times due to “out of the box” or “off the shelf” and “ready to go” software solutions. The days of end-user product fit requiring significant development are diminishing in the name of cost savings. Digital product suppliers are also offering more refined solutions where end-user needs are included and considered within their product development. Most organisations investing in large solutions, like EMR systems, will take a “best of breed” and “off the shelf” approach to purchase, which allows the user to contract with a software vendor to provide a fully functional product. The user knows the functionality offered by the product and exactly what is being purchased. They are often able to see these systems operating in other healthcare organisations. This is the simplest and safest (least risky) option. However, it should be recognised that these systems are not always innovative or leading-edge solutions. Any system that has been developed and implemented in several organisations will, by the nature of the fast evolution of computer systems, be old technology.
Choosing an EMR Solution
When choosing an EMR solution, health providers must evaluate a range of criteria to ensure the system aligns with clinical, operational, and strategic goals. Important considerations are shown in the table below.
|
Consideration |
Description |
|
Functionality |
Core capabilities are robust and relevant (e.g. clinical documentation, creation of care plans, order entry and management, decision support, and integration with diagnostic tools). The ability to view summaries and longitudinal data across visits, decision support, and alerts (Hardy, 2024). Ease of data entry and capture should be considered, ensuring that order management systems can be tailored to suit different user categories and the time taken to enter complex medication orders should be considered (Hardy, 2024; Owen et al., 2023). Functionality to support users to search and retrieve data is also important. |
|---|---|
|
Interoperability |
Exchange of information with other clinical information systems and healthcare providers is a key consideration (Abdelhak & Hanken, 2016; Hardy, 2024), as is compatibility with mainstream standards, for example, HL7, FHIR and DICOM for data exchange (Owen et al., 2023; Williams et al., 2019).This ensures that data can be shared smoothly across different platforms, facilitating better coordination and continuity of care (Gazzarata et al., 2024). |
|
Usability |
A user-friendly interface that supports workflows of health providers. A solution that provides customisable templates, tools to facilitate inbox management, voice and speech recognition, and targeted alerts to reduce administrative burdens and data errors can be beneficial (Dymek et al., 2020; Vainiomäki et al., 2020). |
|
Cost |
Assessment of initial setup costs, such as hardware, software and training and ongoing expenses (e.g. licensing, maintenance and system support). However, understanding the recurrent and ongoing costs is important, as secure cloud storage, software, and hardware upgrades and ongoing training will be required (Hardy, 2024). |
|
Security |
Adherence to legislation, for example, in Australia, each state and territory are required to adhere to federal and state laws with respect to freedom of information, privacy, and reporting to meet the requirements of the Australian Healthcare Reform or Funding Agreements (Australian Government, 2020). Evidence of the vendor’s approach to robust data encryption and user authentication mechanisms should be sought. |
|
Scalability |
Ability to grow with the health provider’s needs, accommodating additional users, locations, and functionalities. |
|
Customisation |
Reports should be able to be customised to suit frontline staff, management, and administrative purposes. The ability to create customised reports should align with the skill sets within the organisation (Hardy, 2024). Customisation and use of templates can aid data capture in digital data capture (Rowlands et al., 2022). |
Vendor relationships are an important consideration. There should be a good fit between the organisation acquiring the EMR and the vendor (Hardy, 2024). Understanding the vendor’s process for making changes, and the availability for technical support, training, and updates should be front of mind (Hardy, 2024). Speaking with other organisations that have purchased systems from vendors will provide insights into and validate the information provided by vendors. When purchasing an EMR, organisations are likely to have a relationship with vendors across many years. Effective relationships will be based upon open and professional communication and clear processes for dispute resolution (usually built into contracts) and establishing communication channels and information flow between IT, clinicians and the vendor can lead to reduced costs and better service (Hardy, 2024).
To promote a sustainable health and social care system, the impact on the environment should be considered and factored into purchasing decisions.(Paul et al., 2023). It involves energy efficiency, reducing electronic waste, responsible disposal practices and adopting other eco-friendly practices to mitigate the environmental footprint of IT infrastructure and operations (Paul et al., 2023). By optimising energy consumption and reducing electronic waste, health and social care organisations can lower their carbon footprint and operational expenses. Incorporating sustainability approaches not only creates value but also demonstrates corporate social responsibility. Investments in energy-saving technologies and cloud-based services also provide scalability and flexibility. Green computing in healthcare includes digitising records and imaging and reducing paper. The use of cloud-based services consolidates servers, reducing energy consumption and costs (Paul et al., 2023)
Case Study – Kenya’s national roll-out of EMR to monitor HIV response
In Kenya, the Ministry of Health recognised the need for a standardised approach to adopting EMR systems as part of the national strategy to enhance HIV care and public health (Kang’a et al., 2017). The Ministry of Health developed standards and guidelines for EMRs and conducted a comprehensive review of existing systems to identify those suitable for nationwide rollout.
The checklist and scoring tool developed for evaluating EMR solutions was a critical component of the selection process. The tool included seven domains, each representing a critical aspect of EMR functionality:
- clinical decision support,
- order entry and results management,
- health information reporting,
- interoperability,
- data security and privacy,
- usability and interface design, and
- system reliability and scalability (Kang’a et al., 2017)
Evaluation of Different EMR Solutions
Evaluating EMR solutions requires a structured approach to compare features, costs, and vendor performances (Abdelhak & Hanken, 2016). The evaluation team should reflect the breadth of users with the ability to assess the product across the functional and technical requirements identified in the tender/procurement process. The steps to perform a robust evaluation include:
1. Needs Assessment
Identify the clinical and administrative needs for the solution. Prioritise those “must have” features (deal breakers) and those that would be nice to have. From initial discussions, stakeholders such as clinicians, IT technicians, and health administrators should be involved. The adoption of an EMR system should align with the organisation’s key strategic priorities (Hardy, 2024). The project should be identified as an organisational priority (Hardy, 2024).
2. Research
Investigate available EMR solutions in use by similar organisations. Talk to users and leaders in organisations using the EMR about various products’ strengths and weaknesses. Focus on vendors with experience in similar settings. Conducting a scan of emerging and new technologies can be helpful in determining how solutions may be impacted by technological trends.
3. Request for Proposal
Issue requests for proposal to vendors, specifying desired features, timeframes, technical requirements, and support needs (Abdelhak & Hanken, 2016; Hardy, 2024).
4. Demonstrations and Testing
Organise solution demonstrations to assess usability and functionality. Conduct testing in simulated healthcare settings to evaluate performance, relevancy, and gather user feedback.
5. Scoring and Analysis
Use weighted scoring systems to compare solutions based on criteria (e.g. functionality, cost and user satisfaction).
Cost and Support
EMR system costs includes initial setup, training, and ongoing maintenance. Providers should also consider the level of vendor support, including technical assistance and updates.
1. Initial Costs
- Hardware and infrastructure: Servers, networking, and user devices.
- Software licensing: Purchase or subscription fees for the EMR software.
- Training and change management: Expenses for onboarding staff and adapting workflows.
- Implementation: System configuration, integration with existing clinical information systems and data migration (Hardy, 2024).
2. Ongoing Costs
- Maintenance: Fees for software updates, patches and hardware upkeep.
- Hardware and equipment upgrades: Desktops, printers and other equipment need to upgraded to meet changing needs and asset retirement.
- Licensing renewals: Annual or periodic fees for continued software use.
- Support: Vendor provided help desk services and troubleshooting (Hardy, 2024).
Success Factors for Implementation
Successful implementation of EMR systems depends on factors such as stakeholder engagement, comprehensive training, and continuous support. Addressing common challenges, such as resistance to change and data migration issues is crucial for a smooth transition from paper to digital. Some factors that support successful EMR implementations are described below.
- Importance of planning: Successful digital health implementation requires thorough planning to align with strategic goals and minimise disruptions (Abdelhak & Hanken, 2016).
- Leadership support: Leaders should create an environment conducive to innovation and change (Lloyd et al., 2018)
- Change management: Implementing an EMR will involve operational, strategic, cultural, and political changes. To manage change effectively, applying models such as Lewin’s 3-Step Model, ADKAR, and Kotter’s 8-Step Change Model is essential.
- Engaging with stakeholders: Involving stakeholders early in the process will build trust and support. Identifying stakeholders and understanding their needs is crucial for assessing the project’s impact and addressing any concerns. Maintaining transparency and open communication helps manage expectations and gain stakeholder buy-in by keeping everyone informed and fostering trust.
- Implementation foundations: Alignment of people, processes, technology, and governance is key to execution:
- People: Engage and train staff, address resistance, and ensure digital literacy.
- Processes: Align new systems with existing workflows or utilise the change to redesign processes for efficiency.
- Technology: Select appropriate technology tools and ensure integration with existing systems.
- Governance: Establish clear roles, responsibilities, and decision-making processes (Abdelhak & Hanken, 2016).
- Evaluation and sustainability: Conduct evaluations to assess progress and outcomes through formative and summative evaluation. Track and measure the benefits of digital health implementation. Plan for long-term sustainability by addressing potential barriers and enablers. Assess and improve digital maturity to enhance the effectiveness of health information systems
Successful digital health implementation is dependent upon comprehensive planning, effective change management, stakeholder engagement, and continuous evaluation. By addressing these areas, health organisations can achieve sustainable and impactful digital transformations.
Activity Success Factors for EMR Implementation
Objective
To identify and understand the key success factors for implementing EMRs in hospitals.
Instructions
Read this paper on the factors for EMR implementation and digital transformation. Identify key learnings from this paper and apply them to a case study through analysis.
Case Study
Scenario: A mid-sized hospital is planning to implement an EMR system. The hospital has faced resistance from some staff members concerned about the changes. The IT infrastructure is outdated, and there is a lack of clear communication about the implementation process.
- What organisational considerations should the hospital address first?
- How can the hospital ensure technical readiness for the EMR implementation?
- What training and support strategies would be most effective?
- How can the hospital address cultural resistance to change?
- What steps should be taken post-implementation to ensure continuous improvement?
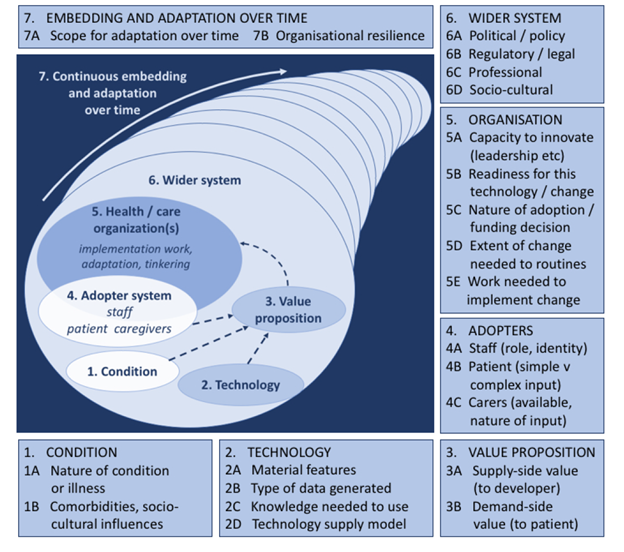
The Non-adoption, Abandonment, Scale-up, Spread, and Sustainability (NASSS) framework [opens in new tab] provides a comprehensive approach to understanding the complexities of adopting and sustaining health technologies such as EMR (Greenhalgh & Abimbola, 2019; Greenhalgh et al., 2010; Greenhalgh et al., 2018; Greenhalgh et al., 2017). The framework, shown in the diagram below, confirms the importance of the technology’s properties, its usability, and how well it integrates with existing systems. Clinical and cost-effectiveness, and how these benefits are distributed among stakeholders is emphasised. The framework considers the individuals and groups who will use the technology, such as patients, healthcare professionals, and caregivers, and reinforces the need to understand their readiness and capacity to adopt the technology (Greenhalgh & Abimbola, 2019; Greenhalgh et al., 2010; Greenhalgh et al., 2018; Greenhalgh et al., 2017). Understanding the organisational context and capacity to implement the technology, and how well the technology aligns with organisational goals is included. The framework examines the wider system, including regulatory, policy, and market factors that can influence the adoption and sustainability of the technology. Finally, the NASSS framework looks at how the technology and its use evolve over time (Greenhalgh & Abimbola, 2019; Greenhalgh et al., 2010; Greenhalgh et al., 2018; Greenhalgh et al., 2017). This includes the processes of adaptation and the technology’s sustainability over the long term. When implementing EMRs, using a framework such as NASSS that analyses the complexity of health care systems can help identify potential barriers and facilitators to the successful implementation and long-term use of health technologies (Greenhalgh & Abimbola, 2019; Greenhalgh et al., 2010; Greenhalgh et al., 2018; Greenhalgh et al., 2017).
Maturity of EMR Systems and Value
Digital health maturity refers to the extent to which healthcare organisations have integrated digital tools and technologies into their operations to enhance patient care, improve population health outcomes, reduce healthcare costs, and improve the work life of healthcare providers. It encompasses the development and implementation of digital health infrastructure, such as electronic health records, telehealth services, and mobile health applications, as well as the training and education of healthcare staff to effectively use these technologies (Woods et al., 2023; Woods et al., 2022). Higher levels of digital health maturity are associated with better patient experiences, more efficient healthcare delivery, and improved health outcomes (Woods et al., 2023; Woods et al., 2022).
The maturity of EMR systems can be assessed through stages such as initial adoption, optimisation, and full integration (HIMSS, 2025). Measuring the value of EMR systems involves evaluating their impact on outcomes, operational efficiency, and overall healthcare quality. Future trends include the integration of artificial intelligence and advanced analytics to further enhance the capabilities of EMR systems (Woods et al., 2022).
The Electronic Medical Record Adoption Model (EMRAM) [opens in new tab] is a framework developed by the Healthcare Information and Management Systems Society (HIMSS) (2025) to assess the maturity and effectiveness of EMR systems within healthcare organisations (HIMSS, 2025; Woods et al., 2022). EMRAM consists of eight stages, ranging from Stage 0, where no EMR systems are in place, to Stage 7, where the EMR system is fully integrated and optimised across the organisation (HIMSS, 2025). Each stage represents a higher level of sophistication and integration, with specific criteria that must be met to advance to the next stage. The model helps healthcare organisations identify their current level of EMR adoption, set goals for improvement, and benchmark their progress against other organisations (HIMSS, 2025).
Achieving higher stages of EMRAM is associated with benefits, including improved patient safety, enhanced clinical outcomes, and increased operational efficiency (HIMSS, 2025). For example, at Stage 3, healthcare organisations have implemented clinical documentation and decision support systems, which can reduce medical errors and improve the quality of care. By Stage 6, organisations have achieved advanced levels of data analytics and interoperability, enabling them to leverage health information for population health management and predictive analytics. Ultimately, reaching Stage 7 signifies that an organisation has fully integrated EMR systems that support seamless care delivery, real-time data access, and continuous quality improvement. This level of maturity not only enhances patient care, but also positions healthcare organisations to meet regulatory requirements and adapt to future technological advancements (HIMSS, 2025).
Activity Test Your Knowledge
Answer this short set of questions to test your knowledge.
Future Trends in EMR/EHR
openEHR (2024) is a technology comprising open specifications, clinical models, and software. The various components of openEHR are produced by the openEHR community and managed by openEHR International, a non-profit organisation established in 2003 and previously overseen by the openEHR Foundation. The openEHR initiative offers numerous benefits, by enhancing the interoperability and accessibility of health data. openEHR aims to provide a standardised architecture for EHRs and seamless data exchange across different healthcare systems and platforms. openEHR is designed to support the creation of longitudinal, consumer-centred health records (Open EHR, 2024). openEHR [opens in new tab] includes valuable information on this initiative.
openEHR’s vendor-neutral approach enhances interoperability, reduces vendor lock-in. and promotes innovation by enabling the integration of best-of-breed solutions. openEHR’s use of detailed clinical models, developed by and for healthcare professionals, ensures the system meets user needs. Additionally low-code application tools support rapid customisation and deployment tailored diverse healthcare settings (Open EHR, 2024).
Personally Held Records
As global mobility increases personally held healthcare records (PHRs) offer significant benefits. They enable individuals to share their health information with multiple healthcare providers, reducing communication gaps, errors, and duplicate tests (Archer et al., 2011; Ford et al., 2016; Tang et al., 2006). PHRs support people to actively participate in their own healthcare management, track health over time, and make informed decisions critical for managing chronic conditions and reducing healthcare expenditure (Ford et al., 2016).
PHR enablers include advancements in technology and supportive government policies. For example, the Australian Government’s investment in the My Health Record system has provided a secure online summary of health information accessible to consumers and healthcare providers (Australian Digital Health Agency, 2024). My Health Record allows people to upload health information and includes Medicare data, medication details and emergency contacts, giving individuals control over who can access their records (Australian Digital Health Agency, 2024).
Many PHR systems allow secure messaging between patients and providers, making it easier to communicate and address health concerns directly and can lead to earlier interventions and improved health outcomes. PHRs that can streamline administrative processes by providing easy access to electronic prescription refills and appointment scheduling are convenient for consumers (Archer et al., 2011; Ford et al., 2016; Tang et al., 2006).
The European Commission (2024) has recommended an EHR exchange format that promotes cross-border EHR interoperability. This initiative enables EU citizens to securely access and exchange their health data across the EU , improving care quality and reducing costs by avoiding duplication of medical tests and procedures (European Commission, 2024; Raab et al., 2023). Many European countries have already launched ambitious PHR projects to advance digital health solutions (European Commission, 2024). Health information exchange facilitates the secure sharing of health information among healthcare providers to improve the quality and continuity of care (Simon et al., 2009; Slawomirski et al., 2023).
In the United Kingdom, patient record access has developed significantly, particularly in the context of GP records, due to widespread computerisation. The National Health System (NHS) app allows patients to manage their personal health records, enabling them to view their GP health records, order prescriptions, and communicate with their healthcare providers (NHS, 2024). This system aims to enhance patient engagement and improve the coordination of care (NHS, 2024).
In Ireland, access to medical records is governed by data protection laws and the Freedom of Information Act (Citizens Information Board, 2025). Patients can access their health records by writing to the Health Service Executive or through data protection requests (Citizens Information Board, 2025). There is also recognition that supporting the use of EHRs and investing in digital health can improve healthcare delivery (McDonald, 2024). This approach aligns with Europe’s goal to make health records more accessible and compatible across borders (European Commission, 2024).
Health data in EMR and EHRs have transformative potential, but often remain siloed within institutions and jurisdictions. For example, Australia’s My Health Record is limited to domestic use. However, platforms like PatientsLikeMe, Open Humans, and Health Record Banks challenge traditional models by enabling personal data sharing, self-health management, research, and clinical care (Kariotis et al., 2020). These models shift data stewardship and explore emerging data governance models, posing challenges for traditional health services and raising policy questions about the use of public good data (Kariotis et al., 2020).
Case Study Analysis and Solution Development
Evaluating and Implementing EMR/EHR Solutions for Sustainable Healthcare Goals
Objective
- Deepen your understanding of EMR/EHR considerations for health information management, decision-making, and implementation.
- Apply knowledge to analyse challenges and propose solutions to enhance EMR/EHR systems.
- Relate EMR/EHR implementation to achieving Sustainable Development Goals (SDG) (United Nations, 2023), especially Goal 3.
Activity Description
The activity centres on a case study of a healthcare system facing challenges in implementing an EMR/EHR solution. Readers will analyse the case, identify key problems, and develop practical solutions that address health information management, EMR selection criteria, and implementation challenges, while aligning with SDG objectives.
Case Study
You are part of the leadership team at a regional hospital tasked with implementing an EMR system to improve healthcare delivery, data management, and patient outcomes.
- The hospital serves a diverse population, including underserved communities.
- Current challenges include fragmented patient records, low interoperability with other systems, clinician resistance to technology, and resource limitations.
- The hospital must ensure the EMR system meets SDG Goal 3 objectives, such as tracking vaccination coverage, disease prevalence, and access to care while supporting real-time decision-making.
Activity Tasks
a. Health Information Management:
-
- Identify the types of data the EMR system should prioritise (e.g., patient outcomes, immunisation records, social determinants of health).
- Describe how these data will improve decision-making and contribute to SDG targets.
b. Choosing an EMR Solution
-
- Evaluate factors like functionality, usability, interoperability, and resources to recommend an EMR system.
- Explain how these features will improve healthcare delivery and patient outcomes.
c. Challenges and Solutions
-
- Identify 2–3 key challenges to implementing the EMR system (e.g., resistance to change, cost, lack of training).
- Propose practical solutions to overcome these challenges.
d. Alignment with SDGs
-
- Provide 1–2 examples of how the EMR system will align with SDG Goal 3 outcomes, such as reducing child mortality, improving maternal health, or ensuring equitable access to healthcare.
Reflection Questions
-
- How can EMR systems address healthcare inequities in resource-limited settings?
- What role does data interoperability play in achieving SDG health targets?
- How can predictive analytics from EMR data contribute to proactive healthcare interventions?
Expected Outcome
Readers will develop a solution-based understanding of EMR/EHR systems, addressing:
- Health data priorities and their alignment with SDGs.
- Decision-making for EMR system selection.
- Solutions to common implementation challenges.
Key Implications for Practice
EMR and EHRs can contribute to effective health care practice. The key implications for practice highlight the importance of careful planning, stakeholder engagement, and evaluation in the successful implementation and use of EMRs and EHRs. When adopting EMRs, health information professionals’ input into robust governance systems, interoperability standards, and user-friendly systems contribute to maximising the benefits of digital health solutions.
Health information management considerations: Effective governance for record systems is crucial. Health information professionals play a central role in ensuring data integrity, privacy, security, and interoperability. They are involved in all phases of EMR acquisition from inception to implementation
Choosing an EMR solution: Providers should consider factors such as cost, ease of use, interoperability, and vendor support. Evaluating different solutions through case studies and pilot programs can help in making informed decisions. The business case for an EMR should justify the project by evaluating benefits, costs, and risks
Functionality and Usability of EMRs: Key functionalities include clinical documentation, order entry, and decision support. Usability considerations involve the system interface, ease of navigation, and the ability to integrate with other systems. Addressing usability challenges is essential for enhancing the efficiency and satisfaction of healthcare providers.
Provider Adoption of Standards for Interoperability: Interoperability is critical for effective use of EHRs. Standards such as HL7, FHIR, and DICOM ensure that different systems can communicate and share information seamlessly. This capability supports public health monitoring and response by facilitating the aggregation and analysis of health data from diverse sources
Success Factors for Implementation: Successful implementation depends on factors such as stakeholder engagement, comprehensive training, and continuous support. Addressing common challenges, such as resistance to change and data migration issues, is crucial for a smooth transition. Effective management strategies are required to ensure a smooth transition and to address any resistance from staff
Maturity of EMR Systems and Value: The maturity of EMR systems can be assessed through stages, such as initial adoption, optimisation, and full integration. Measuring the value of EMR systems involves evaluating their impact on outcomes, operational efficiency, and overall healthcare quality. Future trends include the integration of artificial intelligence and advanced analytics to further enhance EMR systems’ capabilities.
References
Abdelhak, M., & Hanken, M. A. (2016). Health information : management of a strategic resource (Fifth edition. ed.). Elsevier.
Almond, H., & Mather, C. (2023). Digital Health: A Transformative Approach. Elsevier Health Sciences.
Alshehri, A. A., & Alanazi, A. (2023). Usability Study of an Electronic Medical Record From the Nurse Practitioners’ Practice: A Qualitative Study Using the Think-Aloud Technique. Cureus, 15(7), e41603. https://doi.org/10.7759/cureus.41603
Arabi, Y. M., Al Ghamdi, A. A., Al-Moamary, M., Al Mutrafy, A., AlHazme, R. H., & Al Knawy, B. A. (2022). Electronic medical record implementation in a large healthcare system from a leadership perspective. BMC Medical Informatics and Decision Making, 22(1), 66. https://doi.org/10.1186/s12911-022-01801-0
Archer, N., Fevrier-Thomas, U., Lokker, C., McKibbon, K. A., & Straus, S. E. (2011). Personal health records: a scoping review. Journal of the American Medical Informatics Association, 18(4), 515-522. https://doi.org/10.1136/amiajnl-2011-000105
Australian Commission on Safety and Quality in Healthcare. (2021). National Safety and Quality Health Service Standards. In (2nd ed.).
Australian Digital Health Agency. (2023). National Digital Health Strategy 2023-2028. https://www.digitalhealth.gov.au/discover-the-national-digital-health-strategy-2023-2028
Australian Digital Health Agency. (2024). My Health Record. https://www.digitalhealth.gov.au/
Australian Digital Health Agency. (2025). My Health Record system security. https://www.digitalhealth.gov.au/initiatives-and-programs/my-health-record/manage-your-record/privacy-and-access-my-health-record/my-health-record-system-security
Australian Government. (2020). 2020–25 National Health Reform Agreement (NHRA). https://www.health.gov.au/our-work/2020-25-national-health-reform-agreement-nhra
Bärkås, A., Kharko, A., Blease, C., Cajander, Å., Johansen Fagerlund, A., Huvila, I., Johansen, M. A., Kane, B., Kujala, S., Moll, J., Rexhepi, H., Scandurra, I., Wang, B., & Hägglund, M. (2023). Errors, Omissions, and Offenses in the Health Record of Mental Health Care Patients: Results from a Nationwide Survey in Sweden [Original Paper]. J Med Internet Res, 25, e47841. https://doi.org/10.2196/47841
Bhati, D., Deogade, M. S., & Kanyal, D. (2023). Improving Patient Outcomes Through Effective Hospital Administration: A Comprehensive Review. Cureus, 15(10), e47731. https://doi.org/10.7759/cureus.47731
Boonstra, A., Versluis, A., & Vos, J. F. J. (2014). Implementing electronic health records in hospitals: a systematic literature review. BMC Health Services Research, 14(1), 370. https://doi.org/10.1186/1472-6963-14-370
Bostan, S., Johnson, O. A., Jaspersen, L. J., & Randell, R. (2024). Contextual barriers to implementing Open-Source electronic health record systems for low-and lower-middle-income countries: scoping review. Journal of Medical Internet Research, 26, e45242.
Cahill, M., Cleary, B. J., & Cullinan, S. (2025). The influence of electronic health record design on usability and medication safety: systematic review. BMC Health Serv Res, 25(1), 31. https://doi.org/10.1186/s12913-024-12060-2
Canfell, O. J., Chan, W., Pole, J. D., Engstrom, T., Saul, T., Daly, J., & Sullivan, C. (2024). Artificial intelligence after the bedside: co-design of AI-based clinical informatics workflows to routinely analyse patient-reported experience measures in hospitals. BMJ Health Care Inform, 31(1). https://doi.org/10.1136/bmjhci-2024-101124
Canfell, O. J., Woods, L., Meshkat, Y., Krivit, J., Gunashanhar, B., Slade, C., Burton-Jones, A., & Sullivan, C. (2024). The Impact of Digital Hospitals on Patient and Clinician Experience: Systematic Review and Qualitative Evidence Synthesis. J Med Internet Res, 26, e47715. https://doi.org/10.2196/47715
Carayon, P., Kleinschmidt, P., Hose, B. Z., & Salwei, M. (2021). Human Factors and Ergonomics in Health Care and Patient Safety from the Perspective of Medical Residents. In L. Donaldson, W. Ricciardi, S. Sheridan, & R. Tartaglia (Eds.), Textbook of Patient Safety and Clinical Risk Management (pp. 81-89). Springer. https://doi.org/10.1007/978-3-030-59403-9_7
Citizens Information Board. (2025). Access to medical records Ireland. https://www.citizensinformation.ie/en/health/legal-matters-and-health/access-to-medical-records/
Donohue-Ryan, M. A., Peleg, N. A., Fochesto, D., & Kowalski, M. O. (2023). An Organization’s Documentation Burden Reduction Initiative: A Quality Improvement Project. Nursing Economic$, 41(4).
Dubé, M., Hron, J. D., Biesbroek, S., Chan-MacRae, M., Shearer, A., Landi, R., Swenson, M., Kats, D. J., White, D., Birmingham, R., Coogle, L., & Arnold, J. (2025). Human factors and systems simulation methods to optimize peri-operative EHR design and implementation. Advances in Simulation, 10(1). https://doi.org/10.1186/s41077-025-00349-z
Dymek, C., Kim, B., Melton, G. B., Payne, T. H., Singh, H., & Hsiao, C.-J. (2020). Building the evidence-base to reduce electronic health record–related clinician burden. Journal of the American Medical Informatics Association, 28(5), 1057-1061. https://doi.org/10.1093/jamia/ocaa238
eHealth NSW. (2025). Single Digital Patient Record (SDPR). https://www.ehealth.nsw.gov.au/solutions/clinical-care/electronic-medical-records/sdpr
European Commission. (2024). Electronic cross-border health services. https://health.ec.europa.eu/ehealth-digital-health-and-care/electronic-cross-border-health-services_en
Ford, E. W., Hesse, B. W., & Huerta, T. R. (2016). Personal Health Record Use in the United States: Forecasting Future Adoption Levels. J Med Internet Res, 18(3), e73. https://doi.org/10.2196/jmir.4973
Franks, A. M., Clements, C., Bannister, T., Mays-Kingston, A., Beaty, A., Korkmaz, A., Parker, J. A., & Petrany, S. M. (2024). Optimization of Electronic Health Record Usability Through a Department-Led Quality Improvement Process. Ann Fam Med, 22(2), 81-88. https://doi.org/10.1370/afm.3073
Gazzarata, R., Almeida, J., Lindsköld, L., Cangioli, G., Gaeta, E., Fico, G., & Chronaki, C. E. (2024). HL7 Fast Healthcare Interoperability Resources (HL7 FHIR) in digital healthcare ecosystems for chronic disease management: Scoping review. International Journal of Medical Informatics, 189, 105507. https://doi.org/https://doi.org/10.1016/j.ijmedinf.2024.105507
Greenhalgh, T., & Abimbola, S. (2019). The NASSS Framework – A Synthesis of Multiple Theories of Technology Implementation. Stud Health Technol Inform, 263, 193-204. https://doi.org/10.3233/SHTI190123
Greenhalgh, T., Hinder, S., Stramer, K., Bratan, T., & Russell, J. (2010). Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. Bmj, 341.
Greenhalgh, T., Wherton, J., Papoutsi, C., Lynch, J., Hughes, G., A’Court, C., Hinder, S., Procter, R., & Shaw, S. (2018). Analysing the role of complexity in explaining the fortunes of technology programmes: empirical application of the NASSS framework. BMC medicine, 16, 1-15.
Greenhalgh, T., Wherton, J., Papoutsi, C., Lynch, J., Hughes, G., Hinder, S., Fahy, N., Procter, R., & Shaw, S. (2017). Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. Journal of Medical Internet Research, 19(11), e8775.
Hardy, L. R. (2024). Health informatics: An interprofessional approach (3rd ed.). Elsevier Health Sciences.
Havana, T., Kuha, S., Laukka, E., & Kanste, O. (2023). Patients’ experiences of patient-centred care in hospital setting: A systematic review of qualitative studies. Scand J Caring Sci, 37(4), 1001-1015. https://doi.org/10.1111/scs.13174
Henry, T. A. (2023). 7 EHR useability, safety challenges – and how to overcome them. Retrieved 8/1/2025 from https://www.ama-assn.org/practice-management/digital/7-ehr-usability-safety-challenges-and-how-overcome-them
Hettinger, A. Z., Melnick, E. R., & Ratwani, R. M. (2021). Advancing electronic health record vendor usability maturity: Progress and next steps. J Am Med Inform Assoc, 28(5), 1029-1031. https://doi.org/10.1093/jamia/ocaa329
HIMSS. (2025). Electronic Medical Record Adoption Model (EMRAM). https://www.himss.org/maturity-models/emram/
Hong Kong Government. (2020). Electronic Health Record Sharing System. https://www.ehealth.gov.hk/en/healthcare-provider-and-professional/resources/clinic-management-system/index.html
International Standards Organisation. (2010). ISO 9241‑210:2010, definition 2.1 Usability. In.
International Standards Organization. Introduction to HL7 Standards. In.
International Standards Organization. (2023). FHIR Overview. In.
Kaipio, J., Hyppönen, H., & Lääveri, T. (2019). Physicians’ Experiences on EHR Usability: A Time Series from 2010, 2014 and 2017. Stud Health Technol Inform, 257, 194-199. https://www.ncbi.nlm.nih.gov/pubmed/30741195
Kang’a, S., Puttkammer, N., Wanyee, S., Kimanga, D., Madrano, J., Muthee, V., Odawo, P., Sharma, A., Oluoch, T., Robinson, K., Kwach, J., & Lober, W. B. (2017). A national standards-based assessment on functionality of electronic medical records systems used in Kenyan public-Sector health facilities. International Journal of Medical Informatics, 97, 68-75. https://doi.org/https://doi.org/10.1016/j.ijmedinf.2016.09.013
Kariotis, T., Ball, M. P., Greshake Tzovaras, B., Dennis, S., Sahama, T., Johnston, C., Almond, H., & Borda, A. (2020). Emerging health data platforms: From individual control to collective data governance. Data & Policy, 2. https://doi.org/10.1017/dap.2020.14
Keasberry, J., Scott, I. A., Sullivan, C., Staib, A., & Ashby, R. (2017). Going digital: a narrative overview of the clinical and organisational impacts of eHealth technologies in hospital practice. Aust Health Rev, 41(6), 646-664. https://doi.org/10.1071/AH16233
Kemp, T., Butler-Henderson, K., Allen, P., & Ayton, J. (2021). The impact of health information management professionals on patient safety: A systematic review. Health Info Libr J, 38(4), 248-258. https://doi.org/10.1111/hir.12400
Koh, J., & Ahmed, M. (2021). Improving clinical documentation: introduction of electronic health records in paediatrics. BMJ Open Qual, 10(1). https://doi.org/10.1136/bmjoq-2020-000918
Kosteniuk, J., Morgan, D., Elliot, V., Bayly, M., Froehlich Chow, A., Boden, C., & O’Connell, M. E. (2024). Factors identified as barriers or facilitators to EMR/EHR based interprofessional primary care: a scoping review. Journal of Interprofessional Care, 38(2), 319-330. https://doi.org/10.1080/13561820.2023.2204890
Kumar, D., & Suthar, N. (2024). Predictive analytics and early intervention in healthcare social work: a scoping review. Soc Work Health Care, 63(4-5), 208-229. https://doi.org/10.1080/00981389.2024.2316700
Kuo, M., & Lee, J. (2018). Interoperability in health information systems: A review of the barriers and enablers. Health Information Science and Systems, 6, 1-11.
Kushniruk, A., Kaipio, J., Nieminen, M., Hyppönen, H., Lääveri, T., Nohr, C., Kanstrup, A. M., Berg Christiansen, M., Kuo, M. H., & Borycki, E. (2014). Human Factors in the Large: Experiences from Denmark, Finland and Canada in Moving Towards Regional and National Evaluations of Health Information System Usability. Contribution of the IMIA Human Factors Working Group. Yearb Med Inform, 9(1), 67-81. https://doi.org/10.15265/IY-2014-0023
Lloyd, S., Long, K., Oshni Alvandi, A., Di Donato, J., Probst, Y., Roach, J., & Bain, C. (2021). A National Survey of EMR Usability: Comparisons between medical and nursing professions in the hospital and primary care sectors in Australia and Finland. Int J Med Inform, 154, 104535. https://doi.org/10.1016/j.ijmedinf.2021.104535
Lloyd, S., Long, K., Probst, Y., Di Donato, J., Oshni Alvandi, A., Roach, J., & Bain, C. (2024). Medical and nursing clinician perspectives on the usability of the hospital electronic medical record: A qualitative analysis. Health Inf Manag, 53(3), 189-197. https://doi.org/10.1177/18333583231154624
Lloyd, S., Low, S., Win, S. L., Fitzgerald, G., Cliff, C., & Collie, J. (2018). The Ingredients for Innovation: impacts for practice and the education of health service managers. Asia Pacific Journal of Health Management, 13(2). https://doi.org/10.24083/apjhm.2018.0015
McDonald, K. (2024, 8 November 2024). Hospital consultants back investment in digital health. PulseIT.
McGinn, C. A., Gagnon, M.-P., Shaw, N., Sicotte, C., Mathieu, L., Leduc, Y., Grenier, S., Duplantie, J., Abdeljelil, A. B., & Légaré, F. (2012). Users’ perspectives of key factors to implementing electronic health records in Canada: a Delphi study. BMC Medical Informatics and Decision Making, 12(1), 105. https://doi.org/10.1186/1472-6947-12-105
Melnick, E. R., West, C. P., Nath, B., Cipriano, P. F., Peterson, C., Satele, D. V., Shanafelt, T., & Dyrbye, L. N. (2021). The association between perceived electronic health record usability and professional burnout among US nurses. J Am Med Inform Assoc, 28(8), 1632-1641. https://doi.org/10.1093/jamia/ocab059
Ministry of Health Singapore. (2023). Cyber and Data Security Guidelines for Healthcare Providers. https://www.healthinfo.gov.sg/files/MOH_Cir_No_85_2023_04Dec2023_Cyber_and_Data_Security_Guidelines_for_Healthcare_Providers_Annex_A.pdf
Ministry of Health Singapore. (2025). Health Information and the NEHR. Retrieved 11/112/2024 from https://www.healthinfo.gov.sg/overview/health-info-and-nehr/
Murdoch, B. (2021). Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Medical Ethics, 22(1), 122. https://doi.org/10.1186/s12910-021-00687-3
Neame, M. T., Chacko, J., Surace, A. E., Sinha, I. P., & Hawcutt, D. B. (2019). A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc, 26(4), 356-363. https://doi.org/10.1093/jamia/ocy176
NHS. (2024). GP Connect. https://digital.nhs.uk/services/gp-connect
Nielsen, J. (2024). 10 Usability Heuristics for User Interface Design. https://www.nngroup.com/articles/ten-usability-heuristics/
NSW Agency for Clinical Innovation. (2024). Case for Change – Initiation. https://aci.health.nsw.gov.au/__data/assets/pdf_file/0008/486737/Initiation-Case-for-change.pdf
Obermeyer, Z., Powers, B., Vogeli, C., & Mullainathan, S. (2019). Dissecting racial bias in an algorithm used to manage the health of populations. Science, 366(6464), 447-453. https://doi.org/10.1126/science.aax2342
Office of the Australian Information Commissioner. (1982). Freedom of Information Act. https://www.oaic.gov.au/freedom-of-information
Office of the Australian Information Commissioner. (1988). Australian Privacy Principles. https://www.oaic.gov.au/privacy/australian-privacy-principles
Office of the Australian Information Commissioner. (2023). Cyber security incidents impact data breach risk. https://www.oaic.gov.au/news/media-centre/cyber-security-incidents-impact-data-breach-risk
Open EHR. (2024). Open EHR The future of health & care is open. https://openehr.org/
Owen, S., Fojtik, R., Braga, B., & Raghunathan, K. (2023). Interoperability and User Experience. In H. Almond & C. Mather (Eds.), Digital Health: A Transformative Approach. Elsevier Health Sciences.
Palma, F. N. S. (2022). Digital Health Beyond Borders: Interoperability Challenges and Critical Success Factors in the Deployment of Cross-border ePrescription in Finland and Estonia. IEEE International Conference on Digital Health,
Paul, S. G., Saha, A., Arefin, M. S., Bhuiyan, T., Biswas, A. A., Reza, A. W., Alotaibi, N. M., Alyami, S. A., & Moni, M. A. (2023). A comprehensive review of green computing: Past, present, and future research. IEEE Access, 11, 87445-87494.
Raab, R., Küderle, A., Zakreuskaya, A., Stern, A. D., Klucken, J., Kaissis, G., Rueckert, D., Boll, S., Eils, R., Wagener, H., & Eskofier, B. M. (2023). Federated electronic health records for the European Health Data Space. The Lancet Digital Health, 5(11), e840-e847. https://doi.org/10.1016/S2589-7500(23)00156-5
Rigby, M., & Ammenwerth, E. (2016). The Need for Evidence in Health Informatics. Stud Health Technol Inform, 222, 3-13. https://www.ncbi.nlm.nih.gov/pubmed/27198087
Rowlands, S., Tariq, A., Coverdale, S., Walker, S., & Wood, M. (2022). A qualitative investigation into clinical documentation: why do clinicians document the way they do? Health Inf Manag, 51(3), 126-134. https://doi.org/10.1177/1833358320929776
Ruotsalainen, P., & Blobel, B. (2020). Health Information Systems in the Digital Health Ecosystem-Problems and Solutions for Ethics, Trust and Privacy. Int J Environ Res Public Health, 17(9). https://doi.org/10.3390/ijerph17093006
Saari, T., Savolainen, K., Tyllinen, M., Viitanen, J., & Nieminen, M. (2024). Addressing Usability and Complexity in Procurement of IT Systems. Journal of User Experience, 20(1), 27-45.
Scott, I. A., Abdel-Hafez, A., Barras, M., & Canaris, S. (2021). What is needed to mainstream artificial intelligence in health care? Aust Health Rev, 45, 591-596. https://doi.org/10.1071/AH21034
Scott, I. A., Sullivan, C., & Staib, A. (2019). Going digital: a checklist in preparing for hospital-wide electronic medical record implementation and digital transformation. Australian Health Review, 43(3), 302-313. https://doi.org/https://doi.org/10.1071/AH17153
Scott, I. A., van der Vegt, A., Lane, P., McPhail, S., & Magrabi, F. (2024). Achieving large-scale clinician adoption of AI-enabled decision support. BMJ Health Care Inform, 31(1). https://doi.org/10.1136/bmjhci-2023-100971
Serbanati, L. D. (2020). Health digital state and Smart EHR systems. Informatics in Medicine Unlocked, 21, 100494. https://doi.org/https://doi.org/10.1016/j.imu.2020.100494
Shaw, T., Hines, M., & Kielly-Carroll, C. (2018). Impact of digital health on the safety and quality of health care. Australian Commission on Safety and Qualith in Healthcare. https://www.safetyandquality.gov.au/sites/default/files/migrated/Report-The-Impact-of-Digital-Health-on-Safety-and-Quality-of-Healthcar….pdf
Simon, S. R., Evans, J. S., Benjamin, A., Delano, D., & Bates, D. W. (2009). Patients’ attitudes toward electronic health information exchange: qualitative study. J Med Internet Res, 11(3), e30. https://doi.org/10.2196/jmir.1164
Sittig, D. F., Flanagan, T., Sengstack, P., Cholankeril, R. T., Ehsan, S., Heidemann, A., Murphy, D. R., Salmasian, H., Adelman, J. S., & Singh, H. (2025). Revisions to the Safety Assurance Factors for Electronic Health Record Resilience (SAFER) Guides to update national recommendations for safe use of electronic health records. Journal of the American Medical Informatics Association, 32(4), 755-760. https://doi.org/10.1093/jamia/ocaf018
Slawomirski, L., Lindner, L., de Bienassis, K., Haywood, P., Oliveira, T., Hashiguchi., Steentjes, M., & Oderkirk, J. (2023). Progress on implementing and using electronic health record systems: Developments in OECD countries as of 2021.
Smallwood, R. F. (2018). Information Governance for Healthcare Professionals: A Practical Approach (First edition. ed.). Productivity Press. https://doi.org/10.4324/9780203705247
Smelcer, J. B., Miller-Jacobs, H., & Kantrovich, L. (2009). Usability of electronic medical records. Journal of usability studies, 4(2), 70-84.
Stephen, M., Jay, D., & Oyeniyi, J. (2024). The Impact of Electronic Health Records on Healthcare Delivery Transformation and Economic Benefits.
Strudwick, G., Jeffs, L., Kemp, J., Sequeira, L., Lo, B., Shen, N., Paterson, P., Coombe, N., Yang, L., Ronald, K., Wang, W., Pagliaroli, S., Tajirian, T., Ling, S., & Jankowicz, D. (2022). Identifying and adapting interventions to reduce documentation burden and improve nurses’ efficiency in using electronic health record systems (The IDEA Study): protocol for a mixed methods study. BMC Nursing, 21(1), 213. https://doi.org/10.1186/s12912-022-00989-w
synapxe. NEHR FAQs. https://www.synapxe.sg/healthtech/national-programmes/national-electronic-health-record-nehr/faq
Tang, P. C., Ash, J. S., Bates, D. W., Overhage, J. M., & Sands, D. Z. (2006). Personal Health Records: Definitions, Benefits, and Strategies for Overcoming Barriers to Adoption. Journal of the American Medical Informatics Association, 13(2), 121-126. https://doi.org/10.1197/jamia.M2025
Tao, D., Wang, T., Wang, T., Zhang, T., Zhang, X., & Qu, X. (2020). A systematic review and meta-analysis of user acceptance of consumer-oriented health information technologies. Computers in Human Behavior, 104, 106147.
Tasmanian Department of Health. (2022). The Digital Health Transformation program 2022 – 2032. https://www.health.tas.gov.au/about/what-we-do/strategic-programs-and-initiatives/digital-health-transformation-program-2022-2032
Tertulino, R., Antunes, N., & Morais, H. (2024). Privacy in electronic health records: a systematic mapping study. Journal Public Health, 32, 435–454. https://doi.org/https://doi.org/10.1007/s10389-022-01795-z
Thomas Craig, K. J., Willis, V. C., Gruen, D., Rhee, K., & Jackson, G. P. (2021). The burden of the digital environment: a systematic review on organization-directed workplace interventions to mitigate physician burnout. J Am Med Inform Assoc, 28(5), 985-997. https://doi.org/10.1093/jamia/ocaa301
Ting, J., Garnett, A., & Donelle, L. (2021). Nursing education and training on electronic health record systems: An integrative review. Nurse Educ Pract, 55, 103168. https://doi.org/10.1016/j.nepr.2021.103168
Tummers, J., Tobi, H., Catal, C., & Tekinerdogan, B. (2021). Designing a reference architecture for health information systems. BMC Med Inform Decis Mak, 21(1), 210. https://doi.org/10.1186/s12911-021-01570-2
Tyllinen, M., Kaipio, J., & Lääveri, T. (2018). A Framework for Usability Evaluation in EHR Procurement. Stud Health Technol Inform, 247, 446-450. https://www.ncbi.nlm.nih.gov/pubmed/29678000
https://ebooks.iospress.nl/pdf/doi/10.3233/978-1-61499-852-5-446
United Nations. (2023). The Sustainable Development Goals Report 2023: Special Edition. https://unstats.un.org/sdgs.
Vainiomäki, S., Heponiemi, T., Vänskä, J., & Hyppönen, H. (2020). Tailoring EHRs for specific working environments improves work well-being of physicians. International journal of environmental research and public health, 17(13), 4715.
Vasquez, H. M., Pianarosa, E., Sirbu, R., Diemert, L. M., Cunningham, H., Harish, V., Donmez, B., & Rosella, L. C. (2024). Human factors methods in the design of digital decision support systems for population health: a scoping review. BMC Public Health, 24(1), 2458. https://doi.org/10.1186/s12889-024-19968-8
Vos, J. F. J., Boonstra, A., Kooistra, A., Seelen, M., & van Offenbeek, M. (2020). The influence of electronic health record use on collaboration among medical specialties. BMC Health Serv Res, 20(1), 676. https://doi.org/10.1186/s12913-020-05542-6
Warren, L. R., Harrison, M., Arora, S., & Darzi, A. (2019). Working with patients and the public to design an electronic health record interface: a qualitative mixed-methods study. BMC Medical Informatics and Decision Making, 19(1), 250. https://doi.org/10.1186/s12911-019-0993-7
Williams, M. S., Taylor, C. O., Walton, N. A., Goehringer, S. R., Aronson, S., Freimuth, R. R., Rasmussen, L. V., Hall, E. S., Prows, C. A., Chung, W. K., Fedotov, A., Nestor, J., Weng, C., Rowley, R. K., Wiesner, G. L., Jarvik, G. P., & Del Fiol, G. (2019). Genomic Information for Clinicians in the Electronic Health Record: Lessons Learned From the Clinical Genome Resource Project and the Electronic Medical Records and Genomics Network. Front Genet, 10, 1059. https://doi.org/10.3389/fgene.2019.01059
Woods, L., Eden, R., Canfell, O. J., Nguyen, K. H., Comans, T., & Sullivan, C. (2023). Show me the money: how do we justify spending health care dollars on digital health? Med J Aust, 218(2), 53-57. https://doi.org/10.5694/mja2.51799
Woods, L., Eden, R., Duncan, R., Kodiyattu, Z., Macklin, S., & Sullivan, C. (2022). Which one? A suggested approach for evaluating digital health maturity models. Front Digit Health, 4, 1045685. https://doi.org/10.3389/fdgth.2022.1045685
World Health Organization. (2021). Global strategy on digital health 2020-2025.
Image descriptions
Figure 1: A diagram depicting the decomposition of a Health Information System architecture into six main modules with 34 sub-modules. The layout is organised into boxes delineating the modules and their related sub-modules. The decomposition view helps to check for the presence of the required modules for all stakeholders.
- The first module is Medication management, containing sub-modules related to medication handling, distribution, and safety monitoring.
- The second module is Patient monitoring and contains sub-modules related to the assessment, admission, discharge, status, and referrals of patients, and is input for the electronic health record. The Patient monitoring module also contains a sub-module labeled Patient portal in which the patient can check his/her files.
- The Security module with the sub-modules Authentication, Authorisation, and Security mechanisms must ensure the privacy and security of the Health Information System and its data.
- Module number four is Planning and scheduling, with sub-modules used by various stakeholders to ensure proper care coordination.
- The Generic MIS module is not healthcare specific. Its sub-modules are important to keep track of assets, such as staff and inventory, to provide means for organisation-wide communication, quality control, and financial affairs.
These five modules generate data, which needs management. This happens in the sixth module, Data management, which has sub-modules to ensure proper import, sharing, analysis, and data search. Generic MIS involves Finance, Human resources, Documentation, Research and Education, Inventory and Order, Reporting, Demographics, Reimbursement, Communication, and Quality control.

