Navigating the Future
The Impact of Health Informatics and Digital Technologies on Healthcare
Usman Iqbal; Amina Tariq; and Sandeep Reddy
Learning Outcomes
- Evaluate how digital health technologies, particularly Electronic Health and Medical Records (EHRs/EMRs) and Artificial Intelligence, transform healthcare delivery and patient outcomes, demonstrating critical understanding of their benefits and limitations.
- Apply principles of user-centered design and safety protocols in the development and implementation of health information systems, with consideration of interoperability requirements and industry standards.
- Analyse potential risks in health informatics systems and develop appropriate mitigation strategies, while maintaining compliance with information sharing protocols and governance frameworks.
Introduction
Overview of Health Informatics and Digital Health
Health informatics refers to the interdisciplinary field that leverages information technology and data science to improve healthcare delivery, decision-making, and management (Buntin et al., 2011). It combines computer science, healthcare, and information science to optimise the collection, storage, retrieval, and utilisation of health information. Digital health, a broad and evolving domain, encompasses all forms of technology used to improve health outcomes, including mobile health apps, wearable devices, telemedicine, artificial intelligence (AI), and electronic health records (EHRs) (Kellermann & Jones, 2013).
Technologies such as AI and big data analytics enable personalised care by using patient data to generate real-time insights and predictive models (Jiang et al., 2017). The integration of these tools enhances clinical decision-making and promotes efficient care delivery. The integration of AI in healthcare, particularly in diagnostic processes, can introduce challenges such as bias in algorithmic decisions and inequities in care, which require comprehensive risk management strategies (Iqbal et al., 2024 [opens in new tab]). Digital health has rapidly gained traction, driven by the need for healthcare systems to address growing patient populations, chronic diseases, and administrative inefficiencies (Topol, 2019).
Importance of Effective Health Information Management in the Digital Context
Effective management of health information is crucial in the digital age to ensure the quality, safety, and efficiency of healthcare services. With the increasing reliance on digital tools like EHRs/EMRs (hereafter referred to as EHRs), cloud computing, and telemedicine, management and integration of health data across systems are more important than ever (Buntin et al., 2011). Proper data management enables healthcare providers to track patient history, make informed decisions, and reduce errors or misdiagnoses, as effective integration of AI tools can significantly enhance diagnostic performance and support clinical decision-making (Goh et al., 2024).
Digital health tools also empower patients by providing them with access to their health data, allowing them to monitor their conditions and actively engage in their healthcare. For example, patients with chronic diseases like diabetes can use mobile health apps to track blood sugar levels and communicate with their healthcare providers in real time, improving treatment adherence and outcomes (Goel & Taneja, 2023).
Current and Emerging Applications
Electronic Health Record Systems
EHRs have become a fundamental component of modern healthcare systems globally, transforming how healthcare organisations collect, store, and use patient information (Nasserh et al., 2015). As healthcare continues to evolve in the digital era, the global adoption of EHR systems has gained substantial momentum, albeit with varying degrees of progress across different regions (Tsai et al., 2020). The adoption of EHR systems has been notably expeditious in developed countries, with nations such as the United States, United Kingdom, and Australia at the forefront (Morrison et al, 2011). In these countries, governmental initiatives and financial incentives have played a pivotal role in encouraging healthcare providers to transition from paper-based records to electronic systems. Conversely, numerous developing countries face challenges in implementing EHR systems due to limited resources, inadequate infrastructure, and a dearth of trained personnel (Morrison et al, 2011). Nevertheless, there are promising initiatives in countries such as India and Brazil, where governments are investing in digital health infrastructure to enhance healthcare delivery and management (Barbalho et al., 2022; Pai et al., 2021). Read the chapter Electronic Medical and Health Records.
Benefits and Challenges
EHR systems have revolutionised healthcare delivery by offering significant improvements in clinical outcomes, including enhanced quality of care and reduced medical errors, while simultaneously increasing organisational efficiency (Ratwani, 2017). These systems provide comprehensive patient data access, facilitate improved clinical decision-making, and enable effective population health management. The implementation of EHRs has demonstrated considerable potential in transforming healthcare delivery by streamlining processes and improving patient care quality through integrated healthcare informatics tools (Ratwani, 2017).
Notwithstanding their potential advantages, healthcare organisations encounter numerous challenges in the adoption and implementation of EHRs (Menachemi & Collum,2011). A primary obstacle is interoperability, wherein inconsistent data formats and communication deficiencies between disparate systems impede seamless information exchange. Additional challenges comprise concerns regarding data security, patient confidentiality, and the substantial costs associated with implementation and maintenance. While EHRs offer considerable promise for enhancing efficiency, quality, and safety, healthcare providers frequently encounter various implementation challenges that necessitate careful consideration to maximise the systems’ potential benefits (Menachemi & Collum,2011).
Future Outlook
As healthcare continues to evolve, EHRs will play an increasingly pivotal role in delivering high-quality, patient-centred care (Tsai et al., 2020). By addressing the challenges associated with EHR implementation and leveraging their numerous benefits, healthcare organisations can harness the potential of digital technology to improve outcomes and enhance the patient experience (Menachemi & Collum,2011). While EHRs have significantly transformed healthcare globally by improving efficiency, patient safety, and care coordination, addressing challenges related to privacy, interoperability, and resource allocation remains essential to fully realise their potential. Electronic Health and Medical Records are covered in more detail in a separate chapter for those interested in learning more.
Artificial Intelligence (AI): Applications in Diagnostics and Patient Management
The integration of AI into healthcare, particularly in diagnostics and patient management, is rapidly evolving, driven by advancements in machine learning, deep learning, and natural language processing. Current evidence suggests that AI has the potential to revolutionise healthcare delivery, leading to more accurate diagnoses, personalised treatments, and improved patient outcomes (Reddy et al, 2019 [opens in new tab]). This section delves into the theoretical underpinnings and models that form the basis of AI applications in healthcare, supported by empirical evidence from recent studies. The integration of AI in healthcare extends beyond diagnostics and patient management, encompassing areas such as drug discovery, medical imaging analysis, and predictive analytics for population health. Machine learning algorithms, particularly deep neural networks, have demonstrated remarkable capabilities in analysing complex medical data, including EHRs, genomic information, and medical images (Reddy et al., 2019 [opens in new tab]). These AI systems can identify patterns and correlations that may not be immediately apparent to human clinicians, potentially leading to earlier disease detection and more targeted interventions (Wang. 2023). For example, studies have shown that AI-powered image analysis can detect subtle abnormalities in radiological scans with accuracy comparable to, or sometimes exceeding, that of experienced radiologists (Kato et al. 2022). The figure below reflects the need to balance the benefits that AI can bring to challenges in healthcare.
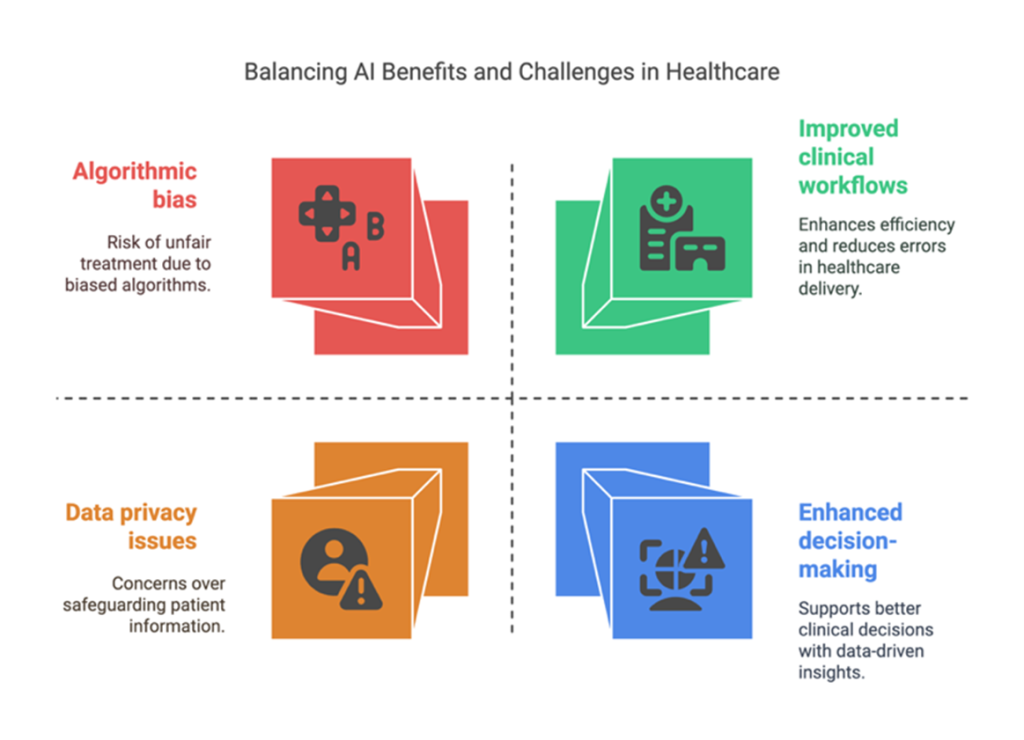
The theoretical framework underlying AI in healthcare is rooted in computational models that simulate human cognitive processes, such as pattern recognition and decision-making. These models are trained on vast datasets of medical information, allowing them to learn and improve their performance over time (Haken et al. 1996). However, the implementation of AI in clinical settings raises important ethical and practical considerations (Reddy & Shaikh, 2025 [opens in new tab]). Issues such as data privacy, algorithmic bias, and the interpretability of AI-generated recommendations need to be carefully addressed to ensure the responsible and equitable deployment of these technologies. As AI continues to evolve, its integration into healthcare systems promises to enhance clinical workflows, reduce medical errors, and ultimately improve the quality and accessibility of healthcare services worldwide. In the next section we will discuss the theory, evidence and models related to AI application in healthcare.
Machine Learning in Diagnostic Imaging
One of the most prominent applications of AI in diagnostics is in the field of medical imaging. Machine learning algorithms, particularly deep learning models like convolutional neural networks (CNNs), have demonstrated remarkable accuracy in analysing images such as X-rays, CT scans, and MRIs.
- Theory: CNNs are inspired by the visual cortex of the brain and are designed to automatically learn hierarchical features from images. They excel at pattern recognition, making them ideal for identifying subtle anomalies in medical images that might be missed by human observers (Aishwarya et al.2025).
- Evidence: Esteva et al. (2017) developed a CNN that could classify skin lesions with an accuracy comparable to that of board-certified dermatologists. The model was trained on a dataset of over 129,000 clinical images, demonstrating the potential of deep learning for skin cancer detection. Similarly, Rajpurkar et al. (2017) developed CheXNet, a 121-layer CNN that could detect pneumonia from chest X-rays exceeding the performance of practicing radiologists.
- Model: The typical model involves training a CNN on a large dataset of annotated medical images, where each image is labelled with the corresponding diagnosis. The trained model can then be used to analyse new, unseen images and provide diagnostic predictions (Aishwarya et al.2025).Natural Language Processing for Clinical Documentation and Decision Support
Natural Language Processing for Clinical Documentation and Decision Support
Natural language processing (NLP) algorithms are employed to extract valuable information from unstructured clinical text, such as EHRs, physician notes, and pathology reports.
- Theory: NLP techniques like tokenisation, part-of-speech tagging, and named entity recognition are used to analyse and understand the meaning of clinical text. Machine learning models, such as recurrent neural networks and transformers are then trained to identify relevant information and patterns within the text (Cheruku et al. 2025).
- Evidence: Miotto et al. (2016) demonstrated the use of unsupervised deep learning on EHR data to derive patient representations that could predict future diagnoses with high accuracy. This approach leverages the vast amount of information contained within EHRs to improve disease prediction. In addition, Wang et al. (2019) implemented a real-time clinical decision support system based on NLP, leading to significant improvement in adherence to clinical practice guidelines and reducing potential medical errors. In the context of pulmonary hypertension (PH), AI algorithms have been designed to detect PH using EHRs, with results showing the model’s capability to accurately retrospectively predict the diagnosis of PH up to 18 months prior to the clinical confirmation of PH (Averjanovaitė et al. 2023). This highlights the potential of AI tools to substantially reduce diagnostic delays in PH and thereby enhance patient outcomes.
- Model: This approach involves preprocessing clinical text, extracting relevant features using NLP techniques, and then training a machine learning model to perform tasks such as disease prediction, risk stratification, or generating clinical alerts.
AI-Powered Predictive Analytics for Patient Management
AI algorithms are increasingly being used to develop predictive models that can forecast patient outcomes, identify high-risk individuals, and personalise treatment plans.
- Theory: Predictive models leverage various machine learning algorithms, including regression, classification, and clustering, to analyse patient data (demographics, medical history, lab results, etc.) and predict future events, such as hospital readmissions, disease progression, or response to treatment (Raghul et al. 2025 and Gandra et al. 2024).
- Evidence: Futoma et al. (2015) developed a machine learning model that could predict sepsis onset in ICU patients’ hours before clinical recognition, potentially allowing for earlier intervention and improved outcomes. Weng et al. (2017) conducted a large-scale study demonstrating that machine learning models could outperform traditional risk assessment tools in predicting cardiovascular events. AI has also found application in other areas of healthcare, such as genomics and drug discovery (Nardone et al., 2024). By exploiting AI algorithms, researchers and doctors can analyse large amounts of genomic data to identify genetic markers associated with certain diseases, including cancer. This information can be used to develop targeted therapies and personalised treatment plans for patients. Clinical Decision Support Systems powered by AI can help healthcare professionals make more informed decisions by providing evidence-based recommendations and warnings (Liao et al. 2023).
- Model: These models are typically built by training machine learning algorithms on historical patient data, where the target variable is the outcome of interest (e.g., hospital readmission). The trained model can then be applied to new patient data to generate predictions and inform clinical decision-making (Gandra et al. 2024).
Robotic Process Automation for Administrative Tasks
AI-driven automation, specifically robotic process automation (RPA), is gaining traction for streamlining administrative tasks, freeing up clinicians’ time, and reducing operational costs. AI has the potential to enhance productivity and improve the quality of care in two main ways: information synthesis, as the amount and complexity of data (e.g., patient data from electronic health records, gene sequencing, or medical literature) is overwhelming for a human operator to handle alone; and enhancement of human performance, by helping healthcare providers track and analyse all available information (Radaelli et al. 2024).
- Theory: RPA involves using software robots to automate repetitive, rule-based tasks, such as appointment scheduling, billing, and claims processing. These robots mimic human actions by interacting with existing software systems without requiring deep integration (Choubey, 2024).
- Evidence: A study by McKinsey Global Institute (2018) estimated that RPA can automate up to 45% of work activities in healthcare, leading to significant cost savings. Healthcare institutions can potentially attain positive results after implementing RPA for tasks like prior authorisation processing and patient registration (Jain & Bhatnagar, 2019).
- Model: The RPA model typically involves identifying suitable tasks for automation, designing workflows for the software robots, and deploying the robots to perform the tasks automatically (Agarwal et al. 2024).
Designing Health Information Systems
Usability: User-centred Design Principles
Usability in digital health applications ensures tools are effective, intuitive, and capable of fostering meaningful health outcomes. Poor usability often leads to low adoption rates, as seen in applications requiring excessive manual data entry, which users may find burdensome (Buis & Huh-Yoo, 2020). A recent cross-sectional survey study conducted across 112 U.S. hospitals explored the relationship between EHR usability and safety performance (Classen et al. 2023). The findings revealed a significant association between higher EHR usability and improved safety outcomes, suggesting that enhancing usability can directly benefit patient safety (Classen et al., 2023).
User-centred design in healthcare focuses on involving end users—patients, clinicians, and other stakeholders—throughout the design process to ensure digital health tools are intuitive, effective, and aligned with user needs (Bhattacharyya et al., 2019). Its importance lies in enhancing usability, fostering adoption, and ultimately improving health outcomes by tailoring solutions to real-world contexts (Johnson et al. 2005, Duffy et al., 2022). Some critical evidence-based principles when designing digital health technologies include:
- Understanding User Context: Designing for diverse populations means recognising context specific challenges. For example, elderly users often struggle with app navigation due to limited digital literacy. By integrating large buttons, voice navigation, and simplified interfaces, developers can address these needs (Azimi et al., 2017).
- Iterative Testing and Feedback: Successful examples include the iterative development of “Learn to Quit,” a smoking cessation app tailored for individuals with serious mental illness. Each design iteration incorporated user feedback, significantly improving usability and engagement (Vilardaga et al., 2018).
- Multistakeholder Collaboration: A collaborative approach was exemplified in the development of a rheumatoid arthritis intervention. Clinicians, patients, and developers co-designed a tool that integrated patient-reported outcomes into routine care, improving both usability and clinical applicability (Ragouzeos et al., 2019).
- Minimise User Burden: The “MyFitnessPal” app initially struggled with user retention due to tedious manual entry. Introducing barcode scanning for food items simplified the process, reducing user burden and boosting engagement (Harte et al., 2017).
- Adapt to Clinical Contexts: Digital health tools often fail when they disrupt clinical workflows. An example is the adaptation of a tablet-based tool for primary care that prioritised patient discussion topics during visits, seamlessly fitting into clinicians’ routines (Lyles et al., 2016).
- Prioritise Accessibility and Inclusivity: Accessibility features in diabetes management apps, such as screen readers and high-contrast modes, have made these tools usable for individuals with visual impairments, expanding their impact (Duffy et al., 2022).
Activity
Learners will identify the User Centred Design principles applied in hypothetical digital health implementation scenarios. In this activity, more than one UCD principle may apply to a single scenario, testing students’ deeper understanding of user-centered design in real-world contexts.
Safety: Minimising Errors and Enhancing Patient Safety
There is growing evidence regarding how digital health technologies can have a positive impact on patient safety, particularly in reducing errors related to medication management. Westbrook et al. (2022) demonstrated the impact of an electronic medication management system in paediatric hospitals. Over one year, the study found a 36% reduction in overall prescribing errors and a 33% decrease in high-risk medication errors compared to paper-based systems. However, in the first 70 days of implementation, potential adverse drug events increased by 62%, highlighting the need for robust support during the transition. Automated barcode medication administration systems further ensure correct drug delivery to the right patient, reducing administration errors by up to 50% (Poon et al., 2010). Beyond medication safety, telemedicine interventions, such as those reviewed by Grygorian et al. (2024), have improved patient safety in abdominal surgery by reducing hospital readmissions by 33% and emergency visits through enhanced postoperative monitoring and early detection of complications. Additionally, AI is emerging as a possible transformative technology in enhancing patient safety. AI applications such as early warning systems, predictive analytics, process automation, and personalised treatment have been associated with cost savings through reduced adverse events and improved operational efficiency in hospital settings (Epelde, 2024). Recent evidence underscores AI’s potential in refining cancer detection and supporting clinical decision-making in oncology. For example, Mota et al. (2023) investigated the effectiveness of an AI system in delineating prostate cancer boundaries to enhance diagnostic precision. The study compared the AI’s performance to that of expert radiologists, assessing accuracy and agreement with pathology results. The results showed that the AI system significantly improved detection and delineation of prostate cancer, providing reliable support for clinical decision-making and treatment planning. These evidence-based examples emphasise the critical role of digital health technologies in minimising errors and promoting safer, more coordinated healthcare practices.
Interoperability and Information Sharing
Seamless information exchange is essential for improving patient outcomes, reducing healthcare costs, and ensuring continuity of care by enabling timely access to accurate and comprehensive patient information (Bates & Samal, 2018). This is enabled by enabling interoperability across the digital ecosystem in healthcare services.
Interoperability, Information Standards and Protocols: Ensuring Seamless Information Exchange
Interoperability in healthcare refers to the ability of different information systems, devices, and applications to access, exchange, and cooperatively use data in a coordinated manner across organisational, regional, and national boundaries (HIMSS, 2021). Interoperability can be categorised into foundational, structural, and semantic types. Foundational interoperability allows basic data exchange without requiring interpretation, structural interoperability ensures data exchange is organised and preserved, and semantic interoperability enables systems to interpret and use the exchanged data meaningfully (Hughes & Karla, 2023).
Standards and protocols play a crucial role in enabling this seamless exchange of information. The International Organization for Standardization (ISO) and the European Committee for Standardization (CEN) have also been instrumental in setting guidelines for global health data exchange. For example, ISO/TS 13940:2015 provides principles and definitions to harmonize healthcare information (ISO, 2015). The adoption of coding systems like SNOMED CT and ICD-10 further ensures consistent representation of clinical data, enhancing its usability across systems (Chang & Mostafa, 2021). The global push for interoperability is underscored by initiatives like the Global Digital Health Partnership, which fosters international collaboration to improve health outcomes through standardised data exchange (Rucker et al., 2020). Regulatory frameworks such as the General Data Protection Regulation in the European Union (Voigt & Bussche, 2017) and the Health Insurance Portability and Accountability Act in the United States (Edemekong et al., 2024) also emphasise secure, standardised data sharing practices.
The adoption of universal standards ensures that healthcare data is comprehensible and usable, regardless of the system or technology used. Key standards like Health Level Seven (HL7), Fast Healthcare Interoperability Resources (FHIR), and Digital Imaging and Communications in Medicine are widely recognised for enabling interoperability (HL7 International, 2023; Vorisek et al. 2022, Graham et al. 2005). HL7 and FHIR provide frameworks for structuring and exchanging health information (HL7 International, 2023; Mandl et al., 2016). While HL7 has been foundational in the development of healthcare communication standards, FHIR, introduced more recently, leverages modern web technologies such as RESTful APIs to facilitate real-time data sharing and interoperability (Mandel et al., 2016; HL7 International, 2023).
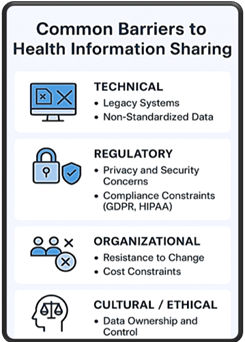
Challenges: Addressing Barriers to Effective Information Sharing
Despite advancements in health information exchange, significant challenges impede effective interoperability. Key barriers include technological fragmentation, data privacy concerns, and organisational resistance (Abell et al. 2023). These issues collectively hinder the realisation of integrated, patient-centric care.
Technological fragmentation: This arises from disparate healthcare systems and platforms, which often use proprietary data formats. As noted by Peiris et al. (2024), the lack of uniform standards across vendors leads to data silos, where critical patient information is trapped within specific systems. Legacy systems in many healthcare facilities also cannot easily integrate with modern technologies, necessitating costly upgrades or replacements (Tariq et al., 2014; Walker et al. 2005).
Data privacy and security: Cybersecurity threats, including data breaches and ransomware attacks, compromise patient trust and deter organisations from fully embracing interoperability (Kruse et al., 2017). Regulations like General Data Protection Regulation and the Health Insurance Portability and Accountability Act aim to mitigate these risks but often create additional complexities, particularly for multinational organisations navigating diverse compliance requirements (Voigt & Bussche, 2017). An explanation of European and United States compliance requirements can be found here GDPR and HIPAA.
Organisational and cultural barriers: Resistance to change, whether due to financial constraints, lack of technical expertise, or perceived threats to competitive advantage, often slows down the adoption of interoperable systems (Fernando et al., 2024). Financial disincentives, such as the cost of implementation and maintenance, are also among the top reasons for delayed interoperability projects (Holmgren et al. 2017).
Data ownership and governance: Ethical concerns regarding data ownership and consent further complicate information sharing. While patients own their health data in principle, inconsistencies in laws and policies across regions create ambiguity in data access rights. For example, a review by Khatri and Assefa (2023) highlighted significant disparities in patient data governance frameworks, which undermine international data exchange efforts.
Limitations in standards adoption: Variability in information standards adoption, especially across low and middle-income countries (LMICs), creates disparities in health data exchange capabilities (Borges et al. 2023). Harmonisation between older legacy systems and modern platforms also remains a significant hurdle.
Addressing these barriers requires a multifaceted approach. Investments in standardised, interoperable systems must be complemented by robust policies that prioritise data security and patient consent (Khatri et al., 2023). Capacity-building initiatives, particularly in LMICs, are essential to equip healthcare providers with the skills and resources needed to implement interoperable technologies. Collaborative efforts, such as those by the World Health Organization (2021) aim to bridge these gaps by promoting universal health coverage through digital health technologies.
Risk Management
Identifying Risks: Potential Issues in Health Informatics
While digital health and health informatics offer substantial benefits, they also come with several risks that need to be managed effectively. One major concern is data security and patient privacy. Healthcare data is highly sensitive, and breaches can lead to significant consequences, including identity theft, financial loss, and loss of trust in healthcare systems (Rindfleisch, 1997). Cybersecurity threats such as ransomware attacks on healthcare organisations highlight the vulnerabilities within health IT systems (Ewoh & Vartiainen, 2024). Further reading on Cybersecurity and Cyber Risk Management is provided in other chapters in this text.
Another risk is the lack of interoperability between different digital health systems. Many healthcare systems use diverse platforms and technologies for managing patient data, which can create silos that hinder information exchange. This lack of interoperability can lead to incomplete or inaccurate patient records, impacting the quality of care (Li et al., 2022).
The integration of AI and machine learning in healthcare also presents challenges, particularly regarding algorithmic bias and the potential for inequities in care. AI models are trained on data that may not represent all demographic groups equally, which can result in biased outcomes, particularly for minority or underserved populations (Obermeyer et al., 2019). To ensure AI tools contribute positively to healthcare, it is crucial to design collaborative human-AI systems and address ethical, legal, and social frameworks that govern their integration (Iqbal et al., 2020).
Mitigation Strategies: Approaches to Managing and Reducing Risks
Addressing the risks associated with digital health requires a multi-pronged approach, including robust cybersecurity measures, standardisation of health data systems, and careful oversight of AI tools. To mitigate cybersecurity risks, healthcare organisations should adopt end-to-end encryption, regularly conduct security audits, and comply with data protection laws like that from the United States, HIPAA (Buntin et al., 2011). The use of secure cloud storage and identity authentication protocols can further enhance the security of health data.
To tackle interoperability issues, it is essential to adopt standardised frameworks for health data exchange, such as the Fast Healthcare Interoperability Resources standard, which enables seamless sharing of patient information between different health systems (Lambrecht et al., 2019). Promoting the adoption of integrated IT platforms that combine EHRs, telemedicine, and patient portals into a single system can also improve data flow and reduce errors.
In the case of AI and machine learning, healthcare organisations must ensure transparency and accountability in algorithm development. Regular audits should be conducted to assess the fairness and performance of AI tools, and algorithms should be trained on diverse, representative datasets to avoid biases (Obermeyer et al., 2019). Moreover, AI should be used as a decision-support tool, with final decisions always remaining in the hands of qualified healthcare professionals. AI has significant potential in revolutionising healthcare by enabling personalised treatment plans and earlier interventions, through predictive models and big data analytics (Iqbal et al., 2024).
Summary
Health informatics and digital health are playing a transformative role in modern healthcare, offering solutions to longstanding issues such as inefficiencies in care delivery, disparities in healthcare access, and the management of chronic diseases. However, the adoption of these technologies is not without its challenges. Data privacy and security, interoperability, and the ethical use of AI are key risks that must be addressed through comprehensive risk management strategies (Cuff, 2023 and Rashid et al. 2025).
Implementing strong cybersecurity practices, promoting data standardisation, and ensuring that AI tools are equitable and transparent will enable healthcare organisations to harness the potential of digital health while minimising the associated risks. The future of healthcare lies in the effective integration of digital health technologies, with the goal of improving patient outcomes, optimising healthcare delivery, and ensuring that these innovations are accessible to all. The integration of AI tools requires a balanced approach to minimise risks while maximising benefits (Iqbal et al., 2020).
Future Directions in Health Informatics and Digital Health
Looking ahead, several key trends are likely to shape the future of health informatics and digital health. One of the most promising areas is the use of precision medicine, which tailors medical treatment to individual genetic profiles, lifestyle factors, and other unique characteristics (Collins & Varmus, 2015). Advancements in genomics, combined with big data analytics and AI, will make it increasingly possible to provide personalised care that is more effective and cost-efficient.
The growth of telehealth, telemedicine and remote patient monitoring will continue to expand, particularly as healthcare systems around the world work to increase access to care, especially in rural and underserved regions. The ongoing development of 5G networks and improved mobile technologies will support real-time communication between healthcare providers and patients, enabling faster diagnosis and treatment.
Current evidence strongly supports the potential of AI to transform diagnostics and patient management (Wang, 2023). Machine learning, deep learning, and NLP are driving innovations in image analysis, clinical documentation, predictive analytics, and automation. While challenges remain in terms of data availability, model interpretability, and regulatory approval, ongoing research and development efforts are paving the way for wider adoption of AI in healthcare (Reddy & Shaikh, 2025). As these technologies mature, we can expect to see even more sophisticated AI models that will further enhance the accuracy, efficiency, and personalisation of healthcare delivery. However, it is crucial to address the ethical, privacy, and regulatory challenges associated with AI implementation to ensure its responsible and equitable adoption across the healthcare sector.
Moreover, blockchain technology holds promise for enhancing data security and patient consent management. By providing decentralised, tamper-proof records of health data transactions, blockchain can increase transparency, improve data privacy, and facilitate secure data sharing across multiple stakeholders (Agbo et al., 2019).
As digital health technologies continue to evolve, it is critical to ensure that these innovations are implemented equitably, providing benefits to all populations, regardless of socioeconomic status or geographic location. Addressing both the opportunities and risks associated with health informatics will enable healthcare systems to create a more efficient, secure, and patient-centred future.
Activity Reflection
Identify three challenges in health and consider:
- How might a digital solution contribute to addressing the problem or challenge?
- Consider emerging technologies and the role they could play in addressing the problem or challenge?
Possible challenges and solutions
Healthcare access in remote areas continues to affect healthcare systems globally. Through telehealth, telemedicine and remote patient monitoring, we’re seeing changes in care delivery. Patients in remote locations can connect with healthcare providers through video consultations, while wearable devices and IoT sensors, powered by 5G technology, enable continuous health monitoring. This digital connection is removing geographical barriers and bringing healthcare to underserved communities.
Mental health service delivery, can be supported through digital platforms. AI-powered chatbots can provide 24/7 support, while virtual therapy sessions make mental health care more accessible. These solutions, enhanced by machine learning and natural language processing, can detect early warning signs and provide timely interventions. Virtual Reality applications offer new approaches to exposure therapy and treatment.
Chronic disease management, can be improved through integrated care management platforms. These systems combine personal health apps, digital health records, and automated monitoring to create a comprehensive care system. Emerging technologies like predictive analytics and blockchain are enabling early intervention and secure data sharing. Smart devices for automated medication dispensing are improving treatment adherence, while coordinated care platforms ensure healthcare providers have access to patient information.
These digital solutions are creating a more connected and efficient healthcare system. By using emerging technologies, we can address current challenges while developing a framework for future healthcare improvements that support better outcomes and more accessible care.
References
Abell, B., Naicker, S., Rodwell, D., Donovan, T., Tariq, A., Baysari, M., … & McPhail, S. M. (2023). Identifying barriers and facilitators to successful implementation of computerized clinical decision support systems in hospitals: A NASSS framework-informed scoping review. Implementation Science, 18(1), 32. https://doi.org/10.1186/s13012-023-01287-y
Agbo, C. C., Mahmoud, Q. H., & Eklund, J. M. (2019). Blockchain technology in healthcare: A systematic review. Healthcare, 7(2), 56. https://doi.org/10.3390/healthcare7020056.
Aishwarya, S., Selvamurugan, C., Lakshmikandhan, K. K., Tharik Raja, J., Manoj Prabhakar, J., & Parthiban, K. G. (2025). Convolutional Neural Networks (CNNs) for Medical Imaging (pp. 263–312). igi global. https://doi.org/10.4018/979-8-3693-9816-6.ch011
Averjanovaitė, V., Gumbienė, L., Zeleckienė, I., & Šileikienė, V. (2023). Unmasking a Silent Threat: Improving Pulmonary Hypertension Screening Methods for Interstitial Lung Disease Patients. Medicina. https://doi.org/10.3390/medicina60010058
Azimi, I., Rahmani, A.M., Liljeberg, P., & Tenhunen, H. (2017). Internet of things for remote elderly monitoring: A study from user-centered perspective. J Ambient Intell Human Comput 8, 273–289. https://doi.org/10.1007/s12652-016-0387-y
Agrawal, R. R., Gupta, S., Sharma, B., & Shinde, S. (2024). Fundamental Of Robotic Process Automation (RPA). San International Scientific Publications. https://doi.org/10.59646/rpa/225
Barbalho, I. M. P., Fernandes, F., Barros, D. M. S., Paiva, J. C., Henriques, J., Morais, A. H. F., Coutinho, K. D., Coelho Neto, G. C., Chioro, A., & Valentim, R. A. M. (2022). Electronic health records in Brazil: Prospects and technological challenges. Frontiers in Public Health, 10, 963841. https://doi.org/10.3389/fpubh.2022.963841
Bates, D. W., & Samal, L. (2018). Interoperability: What Is It, How Can We Make It Work for Clinicians, and How Should We Measure It in the Future? Health Services Research, 53(5), 3270–3277. https://doi.org/10.1111/1475-6773.12852
Bhattacharyya, O., Mossman, K., Gustafsson, L., & Schneider, E. (2019). Using human-centered design to build a digital health advisor for patients with complex needs: Persona and prototype development. Journal of Medical Internet Research, 21(5), e10318. https://doi.org/10.2196/10318
Borges do Nascimento, I. J., Abdulazeem, H., Vasanthan, L. T., Martinez, E. Z., Zucoloto, M. L., Østengaard, L., Azzopardi-Muscat, N., Zapata, T., & Novillo-Ortiz, D. (2023). Barriers and facilitators to utilizing digital health technologies by healthcare professionals. NPJ Digital Medicine, 6(1), 161. https://doi.org/10.1038/s41746-023-00899-4
Buis, L. R., & Huh-Yoo, J. (2020). Common shortcomings in applying user-centered design for digital health. IEEE Pervasive Computing, 19(3), 45–49. https://doi.org/10.1109/MPRV.2020.2997615
Buntin, M. B., Burke, M. F., Hoaglin, M. C., & Blumenthal, D. (2011). The benefits of health information technology: A review of the recent literature shows predominantly positive results. Health Affairs, 30(3), 464-471. https://doi.org/10.1377/hlthaff.2011.0178.
Chang, E., & Mostafa, J. (2021). The use of SNOMED CT, 2013-2020: A literature review. Journal of the American Medical Informatics Association: JAMIA, 28(9), 2017–2026. https://doi.org/10.1093/jamia/ocab084
Cuff, A. (2023) The evolution of digital health and its continuing challenges. BMC Digit Health 1, 3. https://doi.org/10.1186/s44247-022-00004-x
Classen, D. C., Longhurst, C. A., Davis, T., Milstein, J. A., & Bates, D. W. (2023). Inpatient EHR User Experience and Hospital EHR Safety Performance. JAMA Netw Open. 6(9):e2333152. doi:10.1001/jamanetworkopen.2023.33152
Collins, F. S., & Varmus, H. (2015). A new initiative on precision medicine. New England Journal of Medicine, 372(9), 793-795. https://doi.org/10.1056/NEJMp1500523
Cheruku, V. R. (2025). Cloud-Based NLP Models for Clinical Documentation: Accelerating Insights from Unstructured Healthcare Data. European Journal of Computer Science and Information Technology, 13(22), 87–104. https://doi.org/10.37745/ejcsit.2013/vol13n2287104
Choubey, M. (2024). RPA Demystified: How Software Robots are Revolutionizing Customer Service. International Journal of Scientific Research in Computer Science, Engineering and Information Technology, 10(5), 641–648. https://doi.org/10.32628/cseit241051013
Duffy, A., Christie, G. J., & Moreno, S. (2022). The challenges toward real-world implementation of digital health design approaches: Narrative review. JMIR Human Factors, 9(3), e35693. https://doi.org/10.2196/35693
Epelde, F. (2024). Revolutionizing Patient Safety: The Economic and Clinical Impact of Artificial Intelligence in Hospitals. Hospitals, 1(2), 185-194. https://doi.org/10.3390/hospitals1020015
Esteva, A., Kuprel, B., Novoa, R. A., Ko, J., Swetter, S. M., Blau, H. M., & Thrun, S. (2017). Dermatologist-level classification of skin cancer with deep neural networks. Nature, 542(7639), 115–118. https://doi.org/10.1038/nature21056
Ewoh, P., & Vartiainen, T. (2024).Vulnerability to Cyberattacks and Sociotechnical Solutions for Health Care Systems: Systematic Review. Journal of Medical Internet Research, 26, e46904.. doi: 10.2196/46904. PMID: 38820579; PMCID: PMC11179043.
Fernando, M., Abell, B., McPhail, S. M., Tyack, Z., Tariq, A., & Naicker, S. (2024). Applying the Non-Adoption, Abandonment, Scale-up, Spread, and Sustainability Framework Across Implementation Stages to Identify Key Strategies to Facilitate Clinical Decision Support System Integration Within a Large Metropolitan Health Service: Interview and Focus Group Study. JMIR Medical Informatics, 12(1), e60402. doi: 10.2196/60402
Futoma, J., Morris, J., & Lucas, J. (2015). A comparison of models for predicting early hospital readmissions. Journal of Biomedical Informatics, 56, 229–238. https://doi.org/10.1016/j.jbi.2015.05.016
Goel, A., & Taneja, U. (2023). Mobile health applications for health-care delivery: trends, opportunities, and challenges. Journal of Public Health, 1-12.https://doi.org/10.1007/s10389-023-02165-z
Goh, E., Gallo, R., Hom, J., Strong, E., Weng, Y., Kerman, H., … & Chen, J. H. (2024). Large language model influence on diagnostic reasoning: A randomized clinical trial. JAMA Network Open, 7(10), e2440969-e2440969.doi:10.1001/jamanetworkopen.2024.40969.
Graham, R., Perriss, R., & Scarsbrook, A. (2005). DICOM demystified: A review of digital file formats and their use in radiological practice. Clinical Radiology, 60 11, 1133-40. https://doi.org/10.1016/j.crad.2005.07.003
Grygorian, A., Montano, D., Shojaa, M., Ferencak, M., & Schmitz, N. (2024). Digital health interventions and patient safety in abdominal surgery: A systematic review and meta-analysis. JAMA Network Open, 7(4), e248555. https://doi.org/10.1001/jamanetworkopen.2024.8555
Gandra, A. (2024). Predicting hospital readmissions in diabetes patients: A comparative study of machine learning models. International Journal of Health Sciences, 8(3), 289–297. https://doi.org/10.53730/ijhs.v8n3.15189
Haken, H. (1996). Decision Making as Pattern Recognition (pp. 275–278). springer nature. https://doi.org/10.1007/978-3-642-79570-1_18
HIMSS. (2021). The Role of Interoperability in Health Systems’ Digital Transformation: Five key takeaways from a HIMSS APAC virtual government roundtable. Retrieved from https://gkc.himss.org/sites/hde/files/media/file/2021/12/17/himss-apac-interoperability-vgrt-report.pdf
HL7 International. (2023). Health Level Seven (HL7) Standards. https://www.hl7.org/
Harte, R., Glynn, L., Rodríguez-Molinero, A., Baker, P. M., Scharf, T., Quinlan, L. R., et al. (2017). A human-centered design methodology to enhance the usability, human factors, and user experience of connected health systems. JMIR Human Factors, 4(1), e8. https://doi.org/10.2196/humanfactors.5443
Holmgren, A. J., Patel, V., & Adler-Milstein, J. (2017). Progress In Interoperability: Measuring US Hospitals’ Engagement In Sharing Patient Data. Health affairs (Project Hope), 36(10), 1820–1827. https://doi.org/10.1377/hlthaff.2017.0546
Hughes, N., Kalra, D. (2023). Data Standards and Platform Interoperability. In: He, W., Fang, Y., Wang, H. (eds) Real-World Evidence in Medical Product Development. Springer, Cham. https://doi.org/10.1007/978-3-031-26328-6_6
Iqbal, U., Celi, L. A., & Li, Y. C. J. (2020). How can artificial intelligence make medicine more preemptive? Journal of Medical Internet Research, 22(8), e17211.URL: https://www.jmir.org/2020/8/e17211
doi: 10.2196/17211. PMID: 32780024.
Iqbal, U., Hsu, Y. H. E., Celi, L. A., & Li, Y. C. J. (2024). Artificial intelligence in healthcare: Opportunities come with landmines. BMJ Health & Care Informatics, 31(1), e101086. doi: 10.1136/bmjhci-2024-101086. PMID: 38839426; PMCID: PMC11163668.
ISO. (2015). ISO/TS 13940:2015. Health informatics – System of concepts to support continuity of care. Retrieved from https://www.iso.org/standard/58102.html (6th January 2025)
Jain, R & Bhatnagar, R. (2019). Robotic process automation in healthcare-a review. International Robotics & Automation Journal, 5(1), 12–14. https://doi.org/10.15406/iratj.2019.05.00164
Jiang, F., Jiang, Y., Zhi, H., Dong, Y., Li, H., Ma, S., … & Wang, Y. (2017). Artificial intelligence in healthcare: past, present and future. Stroke and Vascular Neurology. https://doi.org/10.1136/svn-2017-000101.
Johnson, C. M., Johnson, T. R., & Zhang, J. (2005). A user-centered framework for redesigning health care interfaces. Journal of Biomedical Informatics, 38(1), 75–87. https://doi.org/10.1016/j.jbi.2004.11.005
Kellermann, A. L., & Jones, S. S. (2013). What it will take to achieve the as-yet-unfulfilled promises of health information technology. Health Affairs, 32(1), 63-68. doi: 10.1377/hlthaff.2012.0693. PMID: 23297272.
Kato, S., Mizuki, M., Amemiya, S., Abe, O., Sakamoto, N., Watanabe, Y., Miki, S., Suzuki, F., Yamashita, H., Takao, H., & Fujimoto, K. (2022). Computer-aided detection improves brain metastasis identification on non-enhanced CT in less experienced radiologists. Acta Radiologica, 64(5), 1958–1965. https://doi.org/10.1177/02841851221139124
Khatri, R. B., & Assefa, Y. (2023). Drivers of the Australian Health System towards Health Care for All: A Scoping Review and Qualitative Synthesis. BioMed Research International, 2023, 6648138. https://doi.org/10.1155/2023/6648138
Kruse, C. S., Frederick, B., Jacobson, T., & Monticone, D. K. (2017). Cybersecurity in healthcare: A systematic review of modern threats and trends. Technology and health care: Official Journal of the European Society for Engineering and Medicine, 25(1), 1–10. https://doi.org/10.3233/THC-161263
Li, E., Clarke, J., Ashrafian, H., Darzi, A., & Neves, A. L. (2022). The impact of electronic health record interoperability on safety and quality of care in high-income countries: systematic review. Journal of Medical Internet research, 24(9), e38144.doi: 10.2196/38144. PMID: 36107486; PMCID: PMC9523524.
Lyles, C. R., Altschuler, A., Chawla, N., Kowalski, C., McQuillan, D., & Bayliss, E. (2016). User-centered design of a tablet waiting room tool for complex patients to prioritize discussion topics for primary care visits. JMIR mHealth and uHealth, 4(3), e108. https://doi.org/10.2196/mhealth.6187
Liao, J., Li, X., Gan, Y., Han, S., Rong, P., Wang, W., Li, W., & Zhou, L. (2023). Artificial intelligence assists precision medicine in cancer treatment. Frontiers in oncology, 12, 998222. https://doi.org/10.3389/fonc.2022.998222
Mandel, J. C., Kreda, D. A., Mandl, K. D., Kohane, I. S., & Ramoni, R. B. (2016). SMART on FHIR: A standards-based, interoperable apps platform for electronic health records. Journal of the American Medical Informatics Association: JAMIA, 23(5), 899–908. https://doi.org/10.1093/jamia/ocv189
McKinsey Global Institute. (2018). Notes from the AI frontier: Applications and value of deep learning. McKinsey Global Institute.
Menachemi, N., & Collum, T. H. (2011). Benefits and drawbacks of electronic health record systems. Risk Management and Healthcare Policy, 4, 47–55. https://doi.org/10.2147/RMHP.S12985
Miotto, R., Li, L., Kidd, B. A., & Dudley, J. T. (2016). Deep patient: An unsupervised representation to predict the future of patients from the electronic health records. Scientific Reports, 6(1), 26094. https://doi.org/10.1038/srep26094
Morrison, Z., Robertson, A., Cresswell, K., Crowe, S., & Sheikh, A. (2011). Understanding Contrasting Approaches to Nationwide Implementations of Electronic Health Record Systems: England, the USA and Australia. Journal of Healthcare Engineering, 2, 25-42. https://doi.org/10.1260/2040-2295.2.1.25.
Mota, S. M., Priester, A., Shubert, J., Bong, J., Sayre, J., Berry-Pusey, B., … Natarajan, S. (2024). Artificial Intelligence Improves the Ability of Physicians to Identify Prostate Cancer Extent. Journal of Urology, 212(1), 52–62. https://doi.org/10.1097/JU.0000000000003960
Nardone, V., Marmorino, F., Germani, M., Cichowska-Cwalińska, N., Menditti, V., Gallo, P., et al. (2024). The Role of Artificial Intelligence on Tumor Boards: Perspectives from Surgeons, Medical Oncologists and Radiation Oncologists. Current Oncology. https://doi.org/10.3390/curroncol31090369
Nasserh.Zaied, A., Elmogy, M., & Abd Elkader, S. (2015). Electronic Health Records: Applications, Techniques and Challenges. International Journal of Computer Applications, 119(14), 38–49. https://doi.org/10.5120/21139-4153
Obermeyer, Z., Powers, B., Vogeli, C., & Mullainathan, S. (2019). Dissecting racial bias in an algorithm used to manage the health of populations. Science, 366(6464), 447-453. doi: 10.1126/science.aax2342. PMID: 31649194.
Pai, M. M. M., Sinha, R. K., Ganiga, R., & Pai, R. M. (2021). Standard electronic health record (EHR) framework for Indian healthcare system. Health Services and Outcomes Research Methodology, 21(3), 339–362. https://doi.org/10.1007/s10742-020-00238-0
Peiris, D., Feyer, A. M., Barnard, J., Billot, L., Bouckley, T., Campain, A., Cordery, D., de Souza, A., Downey, L., Elshaug, A. G., Ford, B., Hanfy, H., Hales, L., Khalaj, B. H., Huckel Schneider, C., Inglis, J., Jan, S., Jorm, L., Landon, B., Lujic, S., … Willcox, D. (2024). Overcoming silos in health care systems through meso-level organisations – a case study of health reforms in New South Wales, Australia. The Lancet Regional Health. Western Pacific, 44, 101013. https://doi.org/10.1016/j.lanwpc.2024.101013
Poon, E. G., Keohane, C. A., Yoon, C. S., et al. (2010). Effect of bar-code technology on the safety of medication administration. New England Journal of Medicine, 362(18), 1698–1707. https://doi.org/10.1056/NEJMsa0907115
Radaelli, D., Di Maria, S., Jakovski, Z., Alempijevic, D., Al-Habash, I., Concato, M., et al. (2024). Advancing Patient Safety: The Future of Artificial Intelligence in Mitigating Healthcare-Associated Infections: A Systematic Review. Healthcare. https://doi.org/10.3390/healthcare12191996
Ragouzeos, D., Gandrup, J., Berrean, B., Li, J., Murphy, M., Trupin, L., & Yazdany, J. (2019). “Am I OK?” Using human-centered design to empower rheumatoid arthritis patients through patient-reported outcomes. Patient Education and Counseling, 102(3), 503–510. https://doi.org/10.1016/j.pec.2018.10.016
Rashid, Z., Ahmed, H., Nadeem, N. et al. The paradigm of digital health: AI applications and transformative trends. Neural Comput & Applic 37, 11039–11070 (2025). https://doi.org/10.1007/s00521-025-11081-0
Rajpurkar, P., Irvin, J., Zhu, K., Yang, B., Mehta, H., Duan, T., … & Langlotz, C. P. (2017). CheXNet: Radiologist-level pneumonia detection on chest x-rays with deep learning. arXiv preprint arXiv:1711.05225.
Ratwani R. (2017). Electronic Health Records and Improved Patient Care: Opportunities for Applied Psychology. Current Directions in Psychological Science, 26(4), 359–365. https://doi.org/10.1177/0963721417700691
Reddy, S., Fox, J., & Purohit, M. P. (2019). Artificial intelligence-enabled healthcare delivery. Journal of the Royal Society of Medicine, 112(1), 22–28. https://doi.org/10.1177/0141076818815510
Reddy, S., & Shaikh, S. (2025). The long road ahead: navigating obstacles and building bridges for clinical integration of artificial intelligence technologies. Journal of Medical Artificial Intelligence. https://doi.org/10.21037/jmai-24-148
Raghul, M. G. (2025). Advanced Prediction and Classification of Liver Cirrhosis using Machine Learning Techniques. International Journal for Research in Applied Science and Engineering Technology, 13(5), 4193–4197. https://doi.org/10.22214/ijraset.2025.71139
Rindfleisch, T. C. (1997). Privacy, information technology, and health care. Communications of the ACM, 40(8), 92-100. https://doi.org/10.1145/257874.25789
Rucker, D., Hasan, A., Lewis, L., Tao, D. (2020). Advancing Interoperability Together Globally: GDHP White Paper on Interoperability. Sydney, Australia GDHP-Interop-Final.pdf
SNOMED International. (2023). SNOMED CT: The global standard for health terms. https://www.snomed.org/
Tariq, A., Lehnbom, E., Oliver, K., Georgiou, A., Rowe, C., Osmond, T., & Westbrook, J. (2014). Design challenges for electronic medication administration record systems in residential aged care facilities. Applied Clinical Informatics, 5(04), 971-987. https://doi.org/10.4338/ACI-2014-08-RA-0062
Topol, E. (2019). Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again. Basic Books.
Tsai, C. H., Eghdam, A., Davoody, N., Wright, G., Flowerday, S., & Koch, S. (2020). Effects of Electronic Health Record Implementation and Barriers to Adoption and Use: A Scoping Review and Qualitative Analysis of the Content. Life (Basel, Switzerland), 10(12), 327. https://doi.org/10.3390/life10120327
Vilardaga, R., Rizo, J., Zeng, E., Kientz, J. A., Ries, R., & Otis, C. (2018). User-centered design of Learn to Quit, a smoking cessation smartphone app for people with serious mental illness. JMIR Serious Games, 6(1), e2. https://doi.org/10.2196/games.8881
Voigt, P., & Bussche, A.V. (2017). The EU General Data Protection Regulation (GDPR): A Practical Guide. Springer, Cham, Switzerland. https://dl.acm.org/doi/10.5555/3152676
Vorisek, C. N., Lehne, M., Klopfenstein, S. A. I., Mayer, P. J., Bartschke, A., Haese, T., & Thun, S. (2022). Fast Healthcare Interoperability Resources (FHIR) for Interoperability in Health Research: Systematic Review. JMIR Medical Informatics, 10(7), e35724. https://doi.org/10.2196/35724
Wang, L., Luo, L., Wang, Y., Wampfler, J., Yang, P., & Liu, H. (2019). Natural language processing for populating lung cancer clinical research data. BMC Medical Informatics and Decision Making, 19(Suppl 5), 239. https://doi.org/10.1186/s12911-019-0931-8
Walker, J., Pan, E., Johnston, D., Adler-Milstein, J., Bates, D. W., & Middleton, B. (2005). The value of health care information exchange and interoperability. Health affairs (Project Hope), Suppl Web Exclusives, W5–W18. https://doi.org/10.1377/hlthaff.w5.10
Weng, S. F., Reps, J., Kai, J., Garibaldi, J. M., & Qureshi, N. (2017). Can machine-learning improve cardiovascular risk prediction using routine clinical data? PLoS One, 12(4), e0174944. https://doi.org/10.1371/journal.pone.0174944
Westbrook, J. I., Li, L., Raban, M. Z., Mumford, V., Badgery-Parker, T., Gates, P., Fitzpatrick, E., Merchant, A., Woods, A., Baysari, M., McCullagh, C., Day, R., Gazarian, M., Dickinson, M., Seaman, K., Dalla-Pozza, L., Ambler, G., Barclay, P., Gardo, A., O’Brien, T., … White, L. (2022). Short- and long-term effects of an electronic medication management system on paediatric prescribing errors. NPJ Digital Medicine, 5(1), 179. https://doi.org/10.1038/s41746-022-00739-x
World Health Organization (2021), Global strategy on digital health 2020-2025. Licence: CC BY-NC-SA 3.0 IG, Available at: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf.
This acronym describes the European Union General Data Protection Regulation (GDPR) Source : Voigt, P., & Bussche, A.V. (2017). The EU General Data Protection Regulation (GDPR): A Practical Guide. Springer, Cham, Switzerland. https://dl.acm.org/doi/10.5555/3152676
An acronym that stands for the Health Insurance Portability and Accountability Act. This Act, from the United States is designed to improve efficiency and requires health services to adopt national standards for electronic health care transactions and code sets, unique health identifiers, and security.

