5 Levels of evidence and search frameworks
 Learning Outcomes
Learning Outcomes
After completing this chapter, you should be able to:
- understand what evidence based practice entails
- identify different search frameworks and how they work
- identify different types of evidence
Evidence-based practice
What is evidence-based practice?
Evidence-based practice (EBP) is the integration of clinical expertise, patient values and the best evidence into the decision-making process for patient care.
The aim of EBP is for health care professionals to practise based on the best research evidence available, rather than on personal opinion. This leads to:
- a reduction in the variations in individual clinicians’ practices
- an enhancement of best practices
- reduced costs
- improved quality in health care
- increased patient satisfaction.
Formulating a clinical question
Translating a knowledge gap into an answerable and well-built clinical question is an important skill for health care practitioners.
A well-built clinical question:
- gives you a head start in finding information that is relevant (applicable to the patient) and valid (accurately measures what the authors state they intend to measure)
- provides you with a checklist for the main concepts to be included in your search strategy
- allows you to find information quickly. If tracking down the evidence takes too long, you will probably avoid it in your clinical practice.
Search frameworks
Quantitative frameworks
The PICO framework is an effective tool for constructing a well-built clinical question.
Click on each of the letters below to identify the PICO elements that can be used in a range of clinical questions.
Let’s have a look at a PICO example. This little story focuses on the care of a patient and explores some of the clinical questions that arose during the encounter.
Formulating a well-built clinical question: A PICO Story – Part A
Formulating a well-built clinical question: A PICO Story – Part B
Now that you have some context, let’s move onto Part B of the story. This part allows you to focus on how the questions, posed by the 5 hospital personnel, can be translated into the PICO framework.
The activities in the slides below, provide you with an opportunity to delve further into each of the questions posed by the Intern, Nurse, Podiatrist, Physiotherapist and Dentist to identify:
- the population of the encounter
- any intervention/s posed
- any comparison/s (alternative/s) that are considered and
- any outcomes that arise from the interventions/comparisons
Instructions: drag and drop the information from the question, into the correct PICO element. To see if you are correct, click the blue Check icon.
This part of Chapter 4 is a recap and pulls all the information from both parts of the PICO Story – Part A (the scenario) and Part B (the questions asked by the hospital personnel) – into a neat little PICO pack. Toggle through the PICO accordion below for the recap.
Adapted from Answering Clinical Questions by The University of Western Australia. © 2025 The University of Western Australia, licenced under a Creative Commons Attribution-NonCommercial (CC BY-NC) 4.0 license.
Qualitative frameworks
Modified PICo
Modified PICo, an adaptation of the PICO framework (Population, Intervention, Comparison, Outcome), was developed specifically to structure qualitative research questions and facilitate systematic searches of qualitative literature. By removing elements that primarily serve quantitative research (Comparison and Outcome) and replacing them with Context, PICo creates a more appropriate framework for exploring experiential and interpretive research questions.
Example question
What are the experiences of first-year nursing students during their initial clinical placements in urban teaching hospitals?
PICo example
P - First-year nursing students
I - Their experiences
Co - Initial clinical placements in urban teaching hospitals.
PCC
The PCC (Population, Concept, Context) framework is a research methodology for qualitative systematic reviews and research question development. It helps researchers examine relationships between people, phenomena, and environments by systematically analysing who is being studied, what is being explored, and under what circumstances.
Example question
How do remote technology workers experience and manage work-life boundaries during the transition to permanent hybrid work arrangements?
PCC example
P - Remote technology workers
C - Experience and management of work-life boundaries
C - During transition to permanent hybrid work arrangements
SPIDER
SPIDER is a research methodology used primarily in healthcare and social sciences. It stands for Sample, Phenomenon of Interest, Design, Evaluation, and Research type. SPIDER helps structure qualitative and mixed-methods studies by providing a clear framework for identifying research questions, participants, and data analysis, ensuring focused and systematic inquiry.
Example question
How do first-generation entrepreneurs perceive and navigate venture capital fundraising challenges through in-depth interviews to understand their lived experiences using a phenomenological approach?
SPIDER example
S - First-generation entrepreneurs
PI - Perceptions and navigation of venture capital fundraising challenges
D - In-depth interviews
E - Understanding lived experiences
R - Phenomenological study
Understanding the evidence
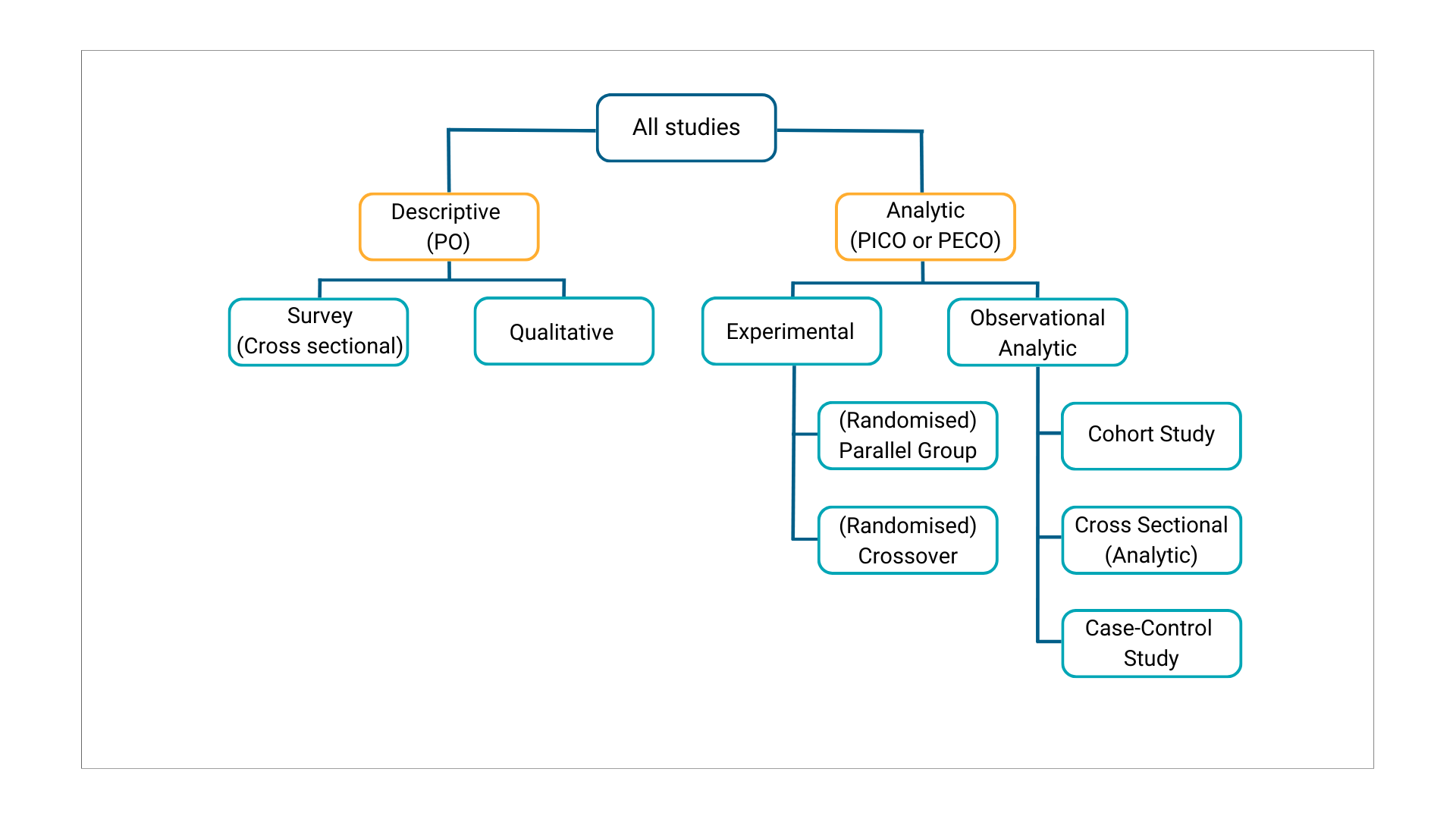
The image below shows a basic tree of possible designs, with branches of groups and subgroups by whether the studies are descriptive or analytic and by whether the analytic studies are experimental or observational.
Levels of evidence
Types of study design
| Evidence | Advantages | Disadvantages |
|---|---|---|
| Randomised Controlled Trial (RCT) An experimental comparison study in which participants are allocated to treatment/intervention or control/placebo groups using a random mechanism (see randomisation). Best for study the effect of an intervention. |
unbiased distribution of confounders; blinding more likely; randomisation facilitates statistical analysis. |
expensive: time and money; volunteer bias; ethically problematic at times. |
| Crossover Design A controlled trial where each study participant has both therapies, e.g, is randomised to treatment A first, at the crossover point they then start treatment B. Only relevant if the outcome is reversible with time, e.g, symptoms. |
all subjects serve as own controls and error variance is reduced thus reducing sample size needed; all subjects receive treatment (at least some of the time); statistical tests assuming randomisation can be used; blinding can be maintained. |
all subjects receive placebo or alternative treatment at some point; washout period lengthy or unknown; cannot be used for treatments with permanent effects |
| Cohort Study Data are obtained from groups who have been exposed, or not exposed, to the new technology or factor of interest (eg from databases). No allocation of exposure is made by the researcher. Best for study the effect of predictive risk factors on an outcome. |
ethically safe; subjects can be matched; can establish timing and directionality of events; eligibility criteria and outcome assessments can be standardised; administratively easier and cheaper than RCT. |
controls may be difficult to identify; exposure may be linked to a hidden confounder; blinding is difficult; randomisation not present; for rare disease, large sample sizes or long follow-up necessary. |
| Case-Control Studies Patients with a certain outcome or disease and an appropriate group of controls without the outcome or disease are selected (usually with careful consideration of appropriate choice of controls, matching, etc) and then information is obtained on whether the subjects have been exposed to the factor under investigation. |
quick and cheap; only feasible method for very rare disorders or those with long lag between exposure and outcome; fewer subjects needed than cross-sectional studies. |
reliance on recall or records to determine exposure status; confounders; selection of control groups is difficult; potential bias: recall, selection. |
| Cross-Sectional Survey A study that examines the relationship between diseases (or other health-related characteristics) and other variables of interest as they exist in a defined population at one particular time (ie exposure and outcomes are both measured at the same time). Best for quantifying the prevalence of a disease or risk factor, and for quantifying the accuracy of a diagnostic test. |
cheap and simple; ethically safe. |
establishes association at most, not causality; recall bias susceptibility; confounders may be unequally distributed; Neyman bias; group sizes may be unequal. |
Table adapted from Study designs, by Centre for Evidence-Based Medicine. © 2025 University of Oxford licenced under a Creative Commons Attribution (CC BY) 4.0 license
In conclusion, evidence-based practice integrates diverse research methodologies and types of evidence to inform clinical decision-making. By critically appraising and applying the best available evidence, practitioners can ensure high-quality, patient-centered care. Understanding the strengths and limitations of various approaches empowers professionals to bridge research and practice effectively, fostering improved outcomes.
For more information visit the Evidence-Based Practice Library Guide.
 GenAI Tip
GenAI Tip
Try GenAI tools like Microsoft Copilot, ChatGPT, Gemini or Claude to help you brainstorm ideas and refine your clinical question.
Try the following prompts:
“I would like to explore information and evidence about [enter topic(s) of interest]. Can you help me form a clinical question, please?”
“This is the clinical question I am considering: [enter question]. Can you suggest 3 refined versions of the question, please?”

