2.3 Digital health leadership and management
Tracy Parrish; Kalpana Raghunathan; Ken Ho; and Fiona Faulks

This chapter aims to provide health professionals with a foundational understanding of leadership and management in digital health, preparing them to navigate the evolving digital ecosystem and contribute meaningfully to the future of health care.
Nurses and midwives comprise the largest professional group in healthcare environments, and they are increasingly required to adopt digital competencies and leadership skills to ensure effective care delivery in a rapidly evolving environment. The National Nursing and Midwifery Digital Health Framework (October 2020) outlines key capability requirements for nurse and midwifery leaders with respect to digital health.
These capabilities acknowledge the leadership role of nurses and midwives in shaping digital health technologies. By contributing to the design, implementation and evaluation of digital health systems, nurses and midwives can bridge the gap between policy and patient-centred care. Nurses and midwives are also expected to explore new data sources, participate in digital technology decisions, and lead the development of digital health strategies and policies. This includes ensuring that the principles of diversity, equity, and inclusion are upheld for all groups and individuals involved, as well as the broader community.
Digital health leadership involves guiding healthcare teams and organisations through the integration and application of technologies such as electronic medical records, telehealth platforms and clinical tools powered by artificial intelligence (AI). Effective leadership requires more than technological understanding – it demands the ability to influence, collaborate on and advocate for sustainable digital transformation that aligns with clinical goals and improves patient outcomes. Management, on the other hand, involves the coordination and oversight of digital initiatives to maintain efficiency, safety and quality in care delivery.
The chapter provides insights into leadership theories relevant to digital health, practical strategies for managing digital initiatives and the challenges posed by legal, ethical and regulatory frameworks. It also addresses the essential elements of stakeholder engagement, risk management and alignment of business objectives with healthcare priorities to ensure seamless digital integration. With case studies illustrating real-world applications, the chapter will equip health professionals with frameworks for digital leadership and guide them on how to lead effectively in the dynamic healthcare environment. It also explores the importance of fostering information cultures, change management models and team collaboration to drive technological adoption across healthcare settings. Finally, the chapter examines future trends, including the rise of AI, data sovereignty and emerging roles within digital health ecosystems. As nurses and midwives take on increasingly multidisciplinary roles in digital health, mastering leadership and management principles will be essential for maintaining high-quality care and achieving meaningful health outcomes in the digital era.
learning outcomes
By the end of this chapter you will be able to:
- Describe the role of digital health leadership and management in the development and running of digital healthcare systems.
- Identify key leadership and management strategies to support digital health initiatives.
- Demonstrate an understanding of governance frameworks related to digital health.
- Recognise alignment of digital health initiatives with organisational goals and better healthcare outcomes.
- Demonstrate an understanding of stakeholder engagement and communication to support digital health adoption and sustainability.
- Identify and apply change, risk, quality and project management processes to support digital health implementation and benefit realisation.
- Identify pathways into digital health leadership and management.
Framing questions
- What is the role of leadership in digital health?
- What does it mean to effectively lead digital transformation in health care?
- What are the essential leadership and management principles necessary to navigate the rapidly evolving digital health landscape?
- What specific processes are important for health professionals to ensure that they are prepared to lead and manage the digital transformation in their work environment?
- How can health professionals develop capacity for interdisciplinary collaboration, policy and governance and the need for continuous learning and adaptation in digital health?
- How can nurses and midwives contribute to digital health strategies in the complex and dynamic healthcare ecosystem?
- How can nurses and midwives contribute to an organisational culture that supports digital innovation in health care?
- How can nurses and midwives meaningfully engage in digital innovation and the transformation in health care?
1. Introduction to digital health leadership and management
This chapter examines the scope of digital health leadership, highlighting its critical role in healthcare transformation through the integration of technologies such as electronic health records and telehealth. It emphasises the importance of effective leadership in driving innovation, while addressing risks like poor adoption. Transformational leadership theory is presented as a model for fostering team motivation and innovation. Legal and ethical challenges, such as data security, are discussed, alongside a case study on Bendigo Health’s 2020 electronic patient record implementation, which illustrates the impact of nurse-led leadership in digital transformation.
1.1 Definition and scope of digital health leadership and management
Digital health leadership and management involves guiding and overseeing the integration of digital technologies into healthcare systems to enhance patient care, operational efficiency and data management (Kruahong & Lachman, 2021). This encompasses strategic planning, implementation and evaluation of digital health initiatives, including electronic health records, telemedicine and health information exchanges (Kruahong & Lachman, 2021). Effective digital health leaders demonstrate a blend of clinical knowledge, technological expertise and change management skills to navigate the complexities of healthcare digitalisation. Conversely, poor leadership has been linked to implementation failure and poor uptake of digital health strategies (Laukka et al., 2020).
1.2 The importance of digital health leadership in the modern healthcare landscape
Digital health leadership is central to the successful development and integration of technology to enhance patient care, operational efficiency and data management within the context of health care (Laukka et al., 2022). Digital transformation in healthcare environments is challenging. Evidence suggests that the Australian health and health management workforce lacks sufficient readiness to effectively engage with digital health and health informatics (Brommeyer et al., 2023). Effective leadership, however, has been identified as a key enabler for the adoption and scaling of digital health innovations (Schlieter et al., 2022).
1.3 The role of nursing and midwifery leadership in digital health
The National Nursing and Midwifery Digital Health Capability Framework outlines essential competencies, including digital professionalism, leadership and advocacy, and information-enabled care, to guide nurses and midwives in effectively integrating digital technologies into their practice (Australian Digital Health Agency, 2020b).
1.4 Leadership theories and application
Numerous leadership theories exist to guide healthcare leaders. Transformational leadership theory lends itself particularly to digital health adoption and effective change management in health care services. Transformational leadership theory emphasises the ability of leaders to inspire and motivate staff to achieve exceptional outcomes by transforming their beliefs, values and attitudes (Bass, 2012). Transformational leaders act as role models, demonstrating high ethical standards and earning trust and respect from their staff (Bass, 2012). They articulate a clear and compelling vision while also challenging assumptions and supporting a solutions-based approach among the team (Bass, 2012). Transformational leaders understand their teams and offer personalised support and mentorship, fostering growth and development (Bass, 2012). Transformational leadership is associated with improved organisational outcomes, enhanced job satisfaction and increased employee performance (Judge et al., 2004).
1.5 Qualities and strategies
Nurses and midwives who are leaders in the digital healthcare space must demonstrate key capabilities to influence the workforce and successfully achieve clinical transformation. Capabilities include effective collaboration and communication, digital literacy and technological competence, an innovation-focused approach, a commitment to their own learning and development and a focus on effective engagement with patients and communities (Hussain et al., 2023; Spanos et al., 2024).
1.6 Advocacy and influencing policy
Nurses and midwives play a central role as advocates in digital health, leveraging their clinical experience to influence policy and practice. Their involvement ensures that digital health initiatives are person centred and effectively integrated into healthcare systems (Janes et al., 2025). Nurses and midwives promote equity in digital health, ensuring equitable access to digital health technologies, particularly for vulnerable populations. Their understandings of acute and community health dynamics enable them to identify and address barriers to digital inclusion, such as technological literacy or resource limitations (Chang et al., 2021).
1.7 Prioritising inclusivity, diversity and accessibility
Principles of inclusivity, diversity, and accessibility are central to digital health because they create equitable healthcare environments, ultimately leading to better healthcare delivery (Sharma et al., 2024; Tan, 2019). Nurses and midwives play a vital role in digital health transformation due to their clinical experience and direct patient care responsibilities. Their expertise allows them to provide valuable insights into the design and functionality of digital tools, ensuring these technologies address diverse needs and are user-friendly, practical, and effective in improving patient care (Tan, 2019). The digitisation of healthcare has also transformed how we care for different populations and the broader community (Sharma et al., 2024).
Unique challenges are faced by rural populations and First Nations people in accessing healthcare (Fitzpatrick et al., 2023; Woods et al., 2024). Engaging with these communities in developing and implementing digital health strategies ensures their needs are met. Tailored solutions, such as telehealth services and culturally sensitive tools, are necessary to address specific requirements (Woods et al., 2024). Additionally, strategies to overcome barriers like limited internet connectivity and digital literacy need to be addressed to ensure equitable access (Tagne et al., 2025). Leadership from nurses and midwives in digital health initiatives will help ensure that technology is integrated seamlessly into clinical workflows, ultimately leading to better healthcare delivery and patient safety.
1.8 Legal and ethical challenges and requirements
Nurses and midwives working in digitally enabled healthcare environments face several ethical challenges and legal requirements in ensuring digital transformational is safe, effective and meets required standards. This is particularly so for privacy, confidentiality and potential legal exposure through poor data entry practice, including ignoring clinical decision support, late data entries and changes, failure to document or incomplete or inaccurate documentation, and copying and pasting notes (Balestra, 2017).
1.9 Case study: Digitisation in the Year of the Nurse – electronic patient record implementation, 2020
Bendigo Health, a regional health service located in the Central Goldfields of Victoria, Australia, is featured in this case study. This case highlights insights from Kate Renzenbrink, the Chief Clinical Informatics Officer, reflecting on the pivotal role nurses and midwives played in the successful implementation of an electronic patient record system in 2020.
case study
*Fully electronic medication management system (records, tracks all steps, order to administration)
activity – Reflective questions
- What pivotal role does each nurse and midwife have in the ePR implementation in this case study?
- Provide examples of why technology uptake is considered poor among clinical nurses and midwives.
2. Digital health management principles
2.1 Business alignment and healthcare goals
The National Nursing and Midwifery Digital Health Capability Framework (Australian Digital Health Agency, 2020b) outlines the capabilities required to support individuals and organisations in extending their digital health development. Five domains, listed under the nursing and midwifery digital capabilities, serve as a resource to align healthcare business development planning and delivery for person-centred, safe, quality and connected care. The five domains for digital health practice are described in Table 1.
Table 1: Digital health capability framework
| Nursing and midwifery digital capabilities | Summary of the capabilities |
| Digital professionalism | Nurses and midwives will demonstrate professional attitudes and behaviours reflecting traditional nursing and midwifery professional standards through using digital tools professionally and personally. |
| Leadership and advocacy | Nurses and midwives will actively be involved in the leadership, development and advocacy for digital health at individual, local and national levels. |
| Data and information quality | Data quality is the backbone of digital health. Nurses and midwives have a crucial role to capture complete, timely and accurate data and manage it in a way that is accessible, reliable, private and secured, for different purposes in healthcare contexts. |
| Information-enabled care | Evidence-based care and continuity of care across settings require appropriate use and sharing of data and the creation and use of information to extend, develop and support evidence-based care. |
| Technology | Nurses and midwives can identify, recommend and use appropriate technology to improve patient outcomes more effectively and efficiently, and to implement policy and procedure to govern the use of digital tools in health care. |
Source: Australian Digital Health Agency (2020b).
video
National Nursing and Midwifery Digital Health Capability Framework: Episode 2 – Digital health benefits
Source: AuDigitalHealth on YouTube.
2.2 Stakeholder engagement and communication, collaborating, and building and managing teams
To lead and manage the development of digital health, it is important to include stakeholders in planning and implementation. The National Digital Health Capability Action Plan (Australian Digital Health Agency, 2024a, p. 5) outlines the strategic priorities for effectively building digital health capabilities across the health workforce to respond to the needs of consumers now and in the future. The action plan has been built in partnership and consultation with government bodies, primary health organisations, professional and clinical peak bodies, digital health peak bodies, education and standards organisations, and industry. It sets out a roadmap for building a competent and capable digital health workforce.
Overall, there are three digital health workforce enablers that require collaboration in order to promote a shared digital culture and continuous learning:
- Frameworks and guidelines: to support consistent digital health capabilities and practice nationally
- Education and training: to enable the health workforce to upskill and adopt digital
- Regulation: to require the inclusion of digital health in regulated health education.
According to the National Digital Health Capability Action Plan Australian Digital Health Agency, 2024a, p.4), building a digitally capable health workforce will lead to significant advancements in healthcare delivery and outcomes (see Table 2). Ultimately, these improvements will contribute to safer, more efficient and person-centred care across the health system.
Table 2: Building a digitally capable workforce
| Benefits of a digitally capable workforce |
| Improved ability to diagnose, treat and manage health conditions |
| Reduction in clinical risk, including minimisation of adverse drug events |
| Enhancement of clinical workflows and the automation of routine and repetitive tasks |
| Improved patient flow and sharing of information throughout the health system |
| Enablement of care outside of hospital settings, in the community or at home |
| Increased transparency of health care |
| Improved population health management |
| Improved operational efficiencies |
Source: Australian Digital Health Agency (2024a)
2.3 Risk management processes
Effective professional and therapeutic relationships build on mutual trust. While communication (e.g. data sharing) in digital health promotes more efficient and personalised care to achieve health goals, it is also a significant concern for information security and privacy. For example, personal and health information and healthcare provider information of 12.9 million individuals may have been exposed in the MediSecure cybersecurity incident. This highlights significant concerns about how best to protect the confidentiality and privacy of customer data in digital health. According to a systematic review to understand patient perspectives on health information exchange (Shen et al., 2019), privacy was the top concern among patients in 59 articles.
Since privacy and confidentiality are big concerns in digital health, cybersecurity must be a solid risk management tool for any digital health system. In Australia, the Cyber Security Strategy 2022–2025 (Australian Digital Health Agency, 2022) sets guiding principles, approaches and areas for action to be taken on cybersecurity. These are described in Table 3.
Table 3: Cybersecurity guiding principles
| Focus areas for cybersecurity and risk management | Guiding principles for cybersecurity and risk management |
| Business led | Cybersecurity services and solutions are aligned with strategic agency objectives and clinical outcomes |
| Future focused | Staying ahead of the evolving digital healthcare environment, ready to securely support the next horizon of digital health |
| Prioritised effort | Resources are focused on maximising value for the Agency and the Australian healthcare ecosystem |
| Security by design | Creating a development, security and operations environment that integrates security into every stage of product development |
| Focus areas | Governance and operations, security culture, workforce investment, capability and proportionality |
Source: Australian Digital Health Agency (2022)
2.4 Quality management tools and techniques
Digital health generates a large volume of healthcare information for administrative, educational, research and clinical purposes. Therefore, information quality is vital and relevant to patient safety. Fadahunsi et al. (2021) conducted a systematic review to synthesise information quality frameworks for digital health technologies and identified a clinical information quality (CLIQ) framework for digital health involving 13 unique dimensions (Figure 2).

The work of Fadahunsi et al. (2021) provides universal coverage on information quality. On top of information quality, the Clinical Governance Framework for Digital Health (Australian Digital Health Agency, 2020a) provides an even wider coverage on quality management and is an important tool for clinical safety, quality and continuous improvement in the delivery of health and care, including through health technologies. The governance framework has five guiding principles:
- Leading with our people
- Systems safety and quality improvement
- Person centredness
- Partnership
- Evidence-based practice.
Watch The role of clinical governance in advancing digital health transformation in global health systems to understand the growth in demands for care, the challenge of workforce sustainability and shifts in consumer expectations.
The role of clinical governance in advancing digital health transformation in global health systems
Source: AuDigitalHealth on YouTube.
2.5 Process reengineering, redesigning workflows and digital solutions
First in this section, watch the following video to understand the possible digital solutions in a healthcare context.
video
Watch Intelligent automation in health care to explore digital solutions on healthcare workflow and the benefits they offer.
Intelligent automation in health care
Source: Excellarate is now Encora on YouTube
Given the advances in digital technology, there is potential for workflow automation in digital health, offering opportunities to optimise work processes, reduce time and cost, assure patient safety, and improve quality of care and communication. A recent systematic review (Layadi, 2023) showed that healthcare automation is an emerging research area. An example is the protocol of Frasquilho et al. (2021) on using digital algorithms to support stepped care for mental health.
activity
Read Protocol for the implementation and assessment of ‘MoodUP’: A stepped care model assisted by a digital platform to accelerate access to mental health care for cancer patients amid the COVID-19 pandemic (Frasquilho et al., 2021)
Discuss the benefits of using digital algorithms to support stepped care for mental health.
This example shows the potential of digital solutions, from primary prevention to tertiary prevention. However, it is important to consider levels of automation because a main tenet of health care is to be person–centred, for which human interaction and knowledge is often required. According to Zayas-Cabán et al. (2021), there are three levels of automation, depending on the nature of the task. These levels are described in Table 4.
Table 4: Levels of work automation
| Low automation | Semi-automated | Fully automated |
|
|
|
Source: Zayas-Cabán et al. (2021, p. 690)
video
Watch Case study: How HM Hospitals improve patient care with automation to understand how automation benefited internal process control, reduced administrative tasks and kept the focus on delivering great patient care in this hospital.
How HM Hospitals improved patient care with automation
Source: UiPath on YouTube
3. Leading digital transformation in health
3.1 Understanding components of change
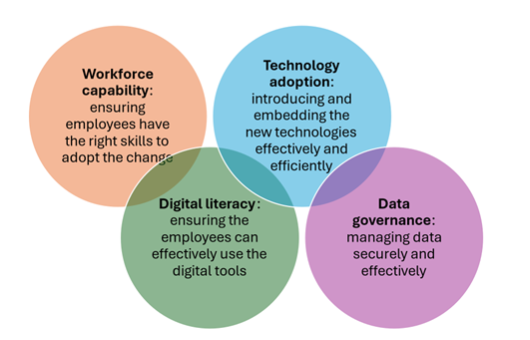
Nurses and midwives play varied and important roles in the implementation of new digital platforms like electronic medical records (see the Bendigo Health case study). Successful change initiatives require effective communication and recognition of organisational change from leaders as a long-term, multi-step approach (Attaran et al., 2019). To reap the benefits of a digital workplace, organisations must prepare for significant change, adopt digital technologies and use data to create positive, intelligent environments for employees. Nurses and midwives can embrace change as a way of improving health care for patients. Understanding the reasons for change is also a crucial step to accepting change in any organisation. Figure 3 illustrates the four essential elements to managing organisational change.
video
Watch What is the future of digital health? for a closer look at change and adoption of evolving technology.
Identify three areas of digital health change that have occurred in the last five years.
What is the future of digital health?
Source: AuDigitalHealth on YouTube
3.2 Program and project management methods and tools
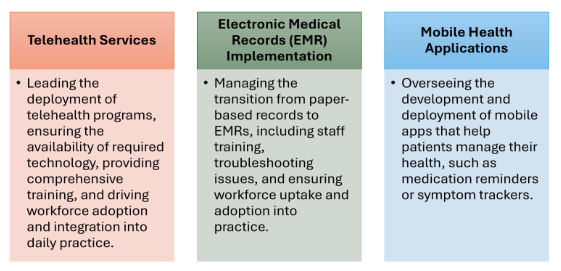
It is increasingly evident that digital solutions will be the foundation of modern health care, so the successful implementation of digital health interfaces is crucial (Dendere et al., 2021). Effective project management tools and methods are essential for the smooth transition and implementation of projects like electronic medical records in health care. Figure 4 shows some examples of digital health implementation that directly impact nursing and midwifery work. Understanding these project management aspects helps nurses and midwives facilitate the effective adoption of digital solutions in health care.
3.3 Value management and benefit realisation from digital health initiatives
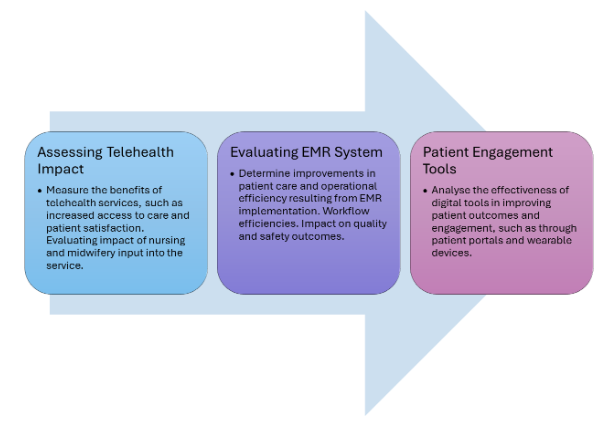
Value management and benefit realisation are crucial concepts that allow investments in healthcare technologies and digital solutions to lead to tangible improvements in patient care, operational efficiency and effective systems uptake. Value management is the process of identifying, maximising and sustaining the value of digital health initiatives throughout their lifecycle (Mathews et al., 2019). The focus is to align digital health projects with the organisation’s goals, ensuring that these projects deliver tangible, measurable outcomes to benefit patients and healthcare organisations. Figure 5 illustrates how this can be achieved.
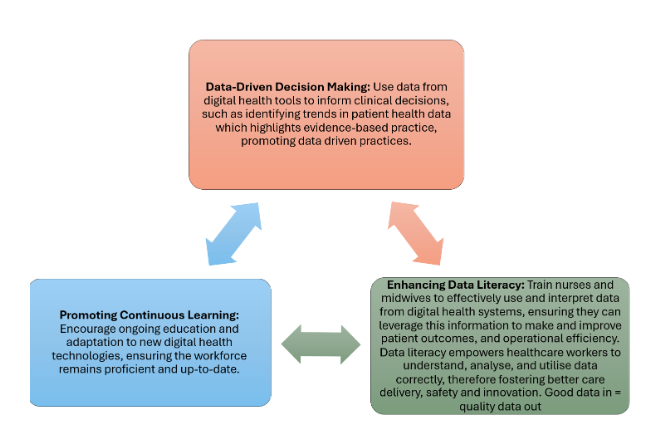
3.4 Information culture
Fostering an information culture in healthcare organisations is essential for making decisions and enhancing data literacy. In relation to digital health, an information culture ensures that data becomes a normal part of daily operations, decision-making processes and patient care strategies. Figure 6 shows some examples of how this works effectively. Digital transformation is primarily about people, not just technology. It necessitates organisational change that is supported by leadership and fuelled by fundamental shifts in workplace culture (Abbu et al., 2022).
4. Future directions, trends and challenges in navigating digital transformation
4.1 Digital transformation and new ways of working
Leaders, nurses and midwives must understand digital transformation in health care, as it will impact how we work in the future (Aroles et al., 2021). Embracing change will prepare the workforce to be at the forefront of modern health care. This change is driven by new technologies, interdisciplinary person-centred care, evolving expectations and data automation (Janssen et al., 2024; Pang et al., 2023). In recent years, technologies like the internet of things (IoT), robotics, AI, big data and blockchain have significantly impacted health care through automation and efficiency. The so-called ‘fifth industrial revolution’ further combines human-centric technologies for flexible, adaptive and sustainable systems (Pang et al., 2023). Personalised and connected health care with real-time data analysis is becoming more common. As organisations become increasingly digitally focused, the skills for a ‘digital culture’ include digital ways of thinking and working (Australian Digital Health Agency, 2024a). This requires engaged and capable leaders and a workforce to support the transition.
4.2 Technological trends in health care
Table 5 summarises significant trends that highlight the transformative impact of technology on health care. These advancements underscore the importance of integrating advanced digital tools and systems to enhance patient care, streamline workflows and create operational efficiency. One of the most significant trends is the increasing influence of AI and machine learning (ML) models. As AI continues to evolve, its integration into various healthcare aspects will deepen. Human–machine collaboration, with robotics and AI systems working alongside humans, will enhance productivity and safety. The advent of 6G technology will further fundamentally transform health care with the promise of unprecedented speed, reliability and connectivity.
Table 5: Some innovative technologies and their healthcare applications
4.3 Threats and opportunities
Emerging work practices across various sectors and the ever-evolving work environment introduce new challenges and opportunities (Aroles et al., 2021). The COVID-19 pandemic fast-tracked the introduction of many advanced technologies into health care, but it also highlighted significant gaps in digital health infrastructure (Tiase & Hobensack, 2023; Woods et al., 2023). Table 6 highlights key threats and opportunities.
Table 6: Threats and opportunities of digital transformation in health care
|
Element |
Threat |
Opportunity |
Outcome |
|
Nursing and midwifery practice |
Need for appropriate workforce development |
Enhanced clinical decision-making through AI decision support systems |
Improved patient care and efficiency |
|
Data security |
Potential for data security breaches and misuse |
Improved patient care and efficiency through technology capabilities |
Enhanced trust and reliability in digital systems |
|
AI integration |
Need for responsible integration and understanding of AI limitations |
Addressing healthcare challenges like access to care and administrative burdens |
Efficiency, productivity, reduced errors and improved patient outcomes |
|
Data ownership |
Debate over data ownership and sovereignty |
Greater transparency and control for consumers over their personal data |
Increased patient engagement and trust |
|
Standardisation and interoperability |
Data inconsistency due to multiple terminologies |
Seamless information exchange and improved healthcare outcomes through standardised terminologies |
Enhanced coordination and quality of care |
|
Health equity (techquity) |
Disparities in access to technology and digital literacy |
Bridging health equity gaps and improving access to care and patient outcomes |
More equitable healthcare delivery |
Sources: Australian Digital Health Agency, 2024b; Janssen et al., 2024; Pang et al., 2023; Woods et al., 2023
4.4 Strategies to manage digital transformation
Nursing and midwifery leaders, and the workforce more broadly, can play a crucial role in maximising the benefits of digital transformation in health care. Concerns and benefits arise because of the increasing role of technology. To ensure the benefits of digital transformation in health care outweigh the threats, it is essential to take proactive and strategic steps. Table 7 provides more information on specific strategies to navigate the digital transformation.
Table 7: Strategies to effectively manage the digital transformation
| Workforce, technology and techquity needs | Strategies to address workforce, technology and techquity needs |
| Nursing and midwifery practice | Create and implement training programs focused on technology, information, data and AI literacy. Undertake continuous education and professional development to keep up with technological advancements. |
| Data security | Develop robust cybersecurity measures to protect sensitive patient data. Undertake regular security audits and updates to maintain system security. |
| AI integration | Provide thorough education on AI limitations and appropriate use for health professionals. Establish and enforce ethical guidelines for AI use in clinical settings. |
| Data ownership | Create transparent policies for data collection, sharing and use. Empower individuals by giving them more control over their personal data. |
| Standardisation and interoperability | Adopt standardised health terminologies like *SNOMED-CT and *ICNP. Develop frameworks for seamless information exchange across the different clinical and healthcare systems. |
| Health equity (techquity) | Work to ensure equitable access to technology for all patients. Provide resources and training to improve digital literacy among healthcare providers, staff and consumers. |
*Systemised nomenclature of medicine – clinical terms; International Classification for Nursing Practice.
Sources: Australian Digital Health Agency, 2024b; Janssen et al., 2024; Pang et al., 2023; Woods et al., 2023
4.5 Evolving healthcare roles
As digital transformation progresses, healthcare roles are also changing. Health professionals must now integrate digital competencies into their traditional skill sets. New digital health roles are emerging, such as informaticians, data scientists, digital health strategists and telehealth coordinators. Educating future graduates for new roles and upskilling the current workforce will be crucial to ensuring that technology adoption is sustainable and supports quality healthcare delivery. This change requires new skills, adaptation to a fast-changing environment, collaboration and a transdisciplinary perspective (Australian Digital Health Agency, 2024b). Leaders and the health workforce must work closely with IT professionals, data scientists and other healthcare leaders to implement and optimise technology solutions in the digital health ecosystem.
4.6 Implications for leadership and management
What are the implications of this digital transformation for practice? Leaders must embrace modern technologies and foster a culture of innovation and continuous improvement. This shift requires incorporating digital literacy, data-driven decision-making, and an understanding of emerging technologies that affect nursing and midwifery work. Driving these changes requires contributing to the strategic vision for workforce education and policy development while addressing ethical issues related to digital health.
Further reading
Refer to the article by Pang et al. (2023) for what the future of work, the workplace and the workforce might involve. Take note of Figure 3 in the article.
5. Conclusion
Digital transformation in health care presents challenges and opportunities for nursing and midwifery leadership. Embracing technology, continuous learning and ethical practices can drive innovation and enhance patient care. Cultivating a digital culture requires not only innovation. Interdisciplinary collaboration and data-driven decisions are also crucial in this process.
Key Takeaways
- Importance of leadership in digital health
- Essential for successful technology integration in health care
- Aims to improve patient care, operational efficiency and data management
- Nursing and midwifery leadership
- Critical for adopting digital health innovations
- Aligns with healthcare goals like person-centred care and improved patient outcomes
- Leadership theories and approaches
- Transformational leadership provides insights for guiding change
- Encourages a positive, collaborative healthcare team environment
- Competency development for nurses and midwives
- Digital literacy, communication and policy advocacy skills are crucial
- Must ensure equitable access and address ethical and legal challenges
- Key elements for digital health success
- Stakeholder engagement and clear communication
- Adherence to privacy and cybersecurity standards
- Challenges and opportunities
- Digital technologies offer opportunities for person-centred care and equity
- Potential challenges include cybersecurity threats
- Leadership responsibilities
- Stay updated on digital health applications
- Integrate new roles (e.g. digital health strategists)
- Collaborate with stakeholders and uphold ethical principles
- Workforce development
- Continuous learning and collaboration build a digitally capable workforce
- Drives safer, more efficient and person-centred care.
6. Further reading
AlHamad, A., Alshurideh, M., Alomari, K., Kurdi, B., Alzoubi, H., Hamouche, S., & Al-Hawary, S. (2022). The effect of electronic human resources management on organizational health of telecommunications companies in Jordan. International Journal of Data and Network Science, 6(2), 429–438.
Australian Digital Health Agency. (2024). Workforce Strategy 2021–2026. Australian Government. https://www.digitalhealth.gov.au/sites/default/files/documents/agency-workforce-strategy-2021-2026.pdf
Pang, T. Y., Lee, T.-K., & Murshed, M. (2023). Towards a new paradigm for digital health training and education in Australia: Exploring the implication of the fifth industrial revolution. Applied Sciences, 13(11), 6854. https://www.mdpi.com/2076-3417/13/11/6854
7. References
Abbu, H., Mugge, P., Gudergan, G., Hoeborn, G., & Kwiatkowski, A. (2022). Measuring the human dimensions of digital leadership for successful digital transformation. Research Technology Management, 65(3), 39–49. https://doi.org/10.1080/08956308.2022.2048588
Abiodun, K. M., Adeniyi, E. A., Awotunde, J. B., Chakraborty, C., Aremu, D. R., Adebiyi, A. A., & Adebiyi, M. O. (2022). Blockchain and internet of things in healthcare systems: Prospects, issues, and challenges. In Digital Health Transformation with Blockchain and Artificial Intelligence (pp. 1–22). CRC Press.
Aroles, J., Cecez-Kecmanovic, D., Dale, K., Kingma, S. F., & Mitev, N. (2021). New ways of working (NWW): Workplace transformation in the digital age. Information and Organization, 31(4), 100378. https://doi.org/10.1016/j.infoandorg.2021.100378
Attaran, M., Attaran, S., & Kirkland, D. (2019). Technology and organizational change: Harnessing the power of digital workplace. In Handbook of research on social and organizational dynamics in the digital era (pp.383–408). IGI Global. https://doi.org/10.4018/978-1-5225-8933-4
Australian Digital Health Agency. (2020a). Clinical Governance Framework for Digital Health. Australian Government. https://www.digitalhealth.gov.au/sites/default/files/documents/clinical_governance_framework-2023.pdf
Australian Digital Health Agency. (2020b). National Nursing and Midwifery Digital Health Capability Framework. Australian Government. https://www.digitalhealth.gov.au/sites/default/files/2020-11/National_Nursing_and_Midwifery_Digital_Health_Capability_Framework_publication.pdf
Australian Digital Health Agency. (2022). Cyber Security Strategy 2022–2025. Australian Government. https://www.digitalhealth.gov.au/sites/default/files/documents/adha-cyber-security-strategy-2022-25.pdf
Australian Digital Health Agency. (2024a). The National Digital Health Capability Action Plan. Australian Government. https://www.digitalhealth.gov.au/sites/default/files/documents/national-digital-health-capability-action-plan.pdf
Australian Digital Health Agency. (2024b). Workforce Strategy 2021–2026. Australian Government. Australian Government. https://www.digitalhealth.gov.au/sites/default/files/documents/agency-workforce-strategy-2021-2026.pdf
Balestra, M. L. (2017). Electronic health records: Patient care and ethical and legal implications for nurse practitioners. Journal for Nurse Practitioners, 13(2), 105–111. https://doi.org/10.1016/j.nurpra.2016.09.010
Bass, B. M. (2012). Transformational Leadership (2nd ed.). Taylor and Francis.
Brommeyer, M., Whittaker, M., Mackay, M., Ng, F., & Liang, Z. (2023). Building health service management workforce capacity in the era of health informatics and digital health: A scoping review. International Journal of Medical Informatics, 169, 104909. https://doi.org/10.1016/j.ijmedinf.2022.104909
Chang, J. E., Lai, A. Y., Gupta, A., Nguyen, A. M., Berry, C. A., & Shelley, D. R. (2021). Rapid transition to telehealth and the digital divide: Implications for primary care access and equity in a post-COVID Era. Milbank Quarterly, 99(2), 340–368. https://doi.org/10.1111/1468-0009.12509
Dao, N.-N. (2023). Internet of wearable things: Advancements and benefits from 6G technologies. Future Generation Computer Systems, 138, 172–184. https://doi.org/10.1016/j.future.2022.07.006
Dendere, R., Janda, M., & Sullivan, C. (2021). Are we doing it right? We need to evaluate the current approaches for implementation of digital health systems. Australian Health Review, 45(6), 778–781. https://doi.org/10.1071/AH20289
Fadahunsi, K. P., O’Connor, S., Akinlua, J. T., Wark, P. A., Gallagher, J., Carroll, C., Car, J., Majeed, A., & O’Donoghue, J. (2021). Information quality frameworks for digital health technologies: Systematic review. Journal of Medical Internet Research, 23(5): e23479.
Fitzpatrick, K. M., Ody, M., Goveas, D., Montesanti, S., Campbell, P., MacDonald, K., Crowshoe, L., Campbell, S., & Roach, P. (2023). Understanding virtual primary healthcare with Indigenous populations: a rapid evidence review. BMC health services research, 23(1), 303. https://doi.org/10.1186/s12913-023-09299-6
Frasquilho, D., Matias, R., Grácio, J., Sousa, B., Luís-Ferreira, F., Leal, J., Cardoso, F., & Oliveira-Maia, A. J. (2021). Protocol for the implementation and assessment of ‘MoodUP’: A stepped care model assisted by a digital platform to accelerate access to mental health care for cancer patients amid the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 18(9), 4629. https://doi.org/10.3390/ijerph18094629
Holland, J., Kingston, L., McCarthy, C., Armstrong, E., O’Dwyer, P., Merz, F., & McConnell, M. (2021). Service robots in the healthcare sector. Robotics, 10(1), 47. https://www.mdpi.com/2218-6581/10/1/47
Hussain, M., Sarfraz, I., & Sharma, A. (2023). Demystifying the role of digital leadership in the healthcare industry: A systematic review towards the development of a digital leadership framework in the healthcare industry. In Digital human modeling and applications in health, safety, ergonomics and risk management. Springer.
Janes, G., Chesterton, L., Heaslip, V., Reid, J., Lüdemann, B., Gentil, J., Oxholm, R.-A., Hamilton, C., Phillips, N., & Shannon, M. (2025). Current nursing and midwifery contribution to leading digital health policy and practice: An integrative review. Journal of Advanced Nursing, 81(1), 116–139. https://doi.org/10.1111/jan.16265
Janssen, A., Baysari, M., Igasto, C., Quirke, K., Milnes, P., Shaw, T., & Dunn, A. (2024). A digitally enabled health workforce for Australia. Australian Health Review, 48(6), 700–704. https://doi.org/10.1071/AH24286
Judge, T. A., Piccolo, R. F., & Zedeck, S. (2004). Transformational and transactional leadership: A meta-analytic test of their relative validity. Journal of Applied Psychology, 89(5), 755–768. https://doi.org/10.1037/0021-9010.89.5.755
Kruahong, N., & Lachman, J. M. (2021). What can good leadership do to support the digital revolution in health? Health Policy and Technology, 10(4), 100579. https://doi.org/10.1016/j.hlpt.2021.100579
Laukka, E., Huhtakangas, M., Heponiemi, T., & Kanste, O. (2020). Identifying the roles of healthcare leaders in HIT implementation: A scoping review of the quantitative and qualitative evidence. International Journal of Environmental Research and Public Health, 17(8), 2865. https://doi.org/10.3390/ijerph17082865
Laukka, E., Pölkki, T., & Kanste, O. (2022). Leadership in the context of digital health services: A concept analysis. Journal of Nursing Management, 30(7), 2763–2780. https://doi.org/10.1111/jonm.13763
Layadi, I.C. (2023). Healthcare automation: A systematic literature review. In V. G. Duffy, M. Lehto, Y. Yih, & R. W. Proctor (Eds.), Human-automation interaction: Vol. 10. Automation, Collaboration, & E-Services. Springer. https://doi.org/10.1007/978-3-031-10780-1_9
Marsh, E. (2018). Understanding the Effect of Digital Literacy on Employees’ Digital Workplace Continuance Intentions and Individual Performance. International Journal of Digital Literacy and Digital Competence, 9(2), 15–33. https://doi.org/10.4018/IJDLDC.2018040102
Mathews, S. C., McShea, M. J., Hanley, C. L., Ravitz, A., Labrique, A. B., & Cohen, A. B. (2019). Digital health: a path to validation. NPJ Digital Medicine, 2(1), 38–38. https://doi.org/10.1038/s41746-019-0111-3
Ndlovu, K., Mars, M., & Scott, R. E. (2021). Interoperability frameworks linking mHealth applications to electronic record systems. BMC Health Services Research, 21(1), 459–459. https://doi.org/10.1186/s12913-021-06473-6
Pang, T. Y., Lee, T.-K., & Murshed, M. (2023). Towards a new paradigm for digital health training and education in Australia: Exploring the implication of the fifth industrial revolution. Applied Sciences, 13(11), 6854. https://www.mdpi.com/2076-3417/13/11/6854
Schlieter, H., Marsch, L. A., Whitehouse, D., Otto, L., Londral, A. R., Teepe, G. W., Benedict, M., Ollier, J., Ulmer, T., Gasser, N., Ultsch, S., Wollschlaeger, B., & Kowatsch, T. (2022). Scale-up of digital innovations in health care: Expert commentary on enablers and barriers. Journal of Medical Internet Research, 24(3), e24582. https://doi.org/10.2196/24582
Sharma, Y., Saha, A., & Goldsack, J. C. (2024). Defining the Dimensions of Diversity to Promote Inclusion in the Digital Era of Health Care: A Lexicon [Viewpoint]. JMIR Public Health Surveill, 10, e51980. https://doi.org/10.2196/51980
Shen, N., Bernier, T., Sequeira, L., Strauss, J., Silver, M. P., Carter-Langford, A., & Wiljer, D. (2019). Understanding the patient privacy perspective on health information exchange: A systematic review. International Journal of Medical Informatics (Shannon, Ireland), 125, 1–12. https://doi.org/10.1016/j.ijmedinf.2019.01.014
Spanos, S., Leask, E., Patel, R., Datyner, M., Loh, E., & Braithwaite, J. (2024). Healthcare leaders navigating complexity: A scoping review of key trends in future roles and competencies. BMC Medical Education, 24(1), 720. https://doi.org/10.1186/s12909-024-05689-4
Stoumpos, A. I., Kitsios, F., & Talias, M. A. (2023). Digital Transformation in Healthcare: Technology Acceptance and Its Applications. International Journal of Environmental Research and Public Health, 20(4), 3407-. https://doi.org/10.3390/ijerph20043407
Tagne, J. F., Burns, K., O’Brein, T., Chapman, W., Cornell, P., Huckvale, K., Ameen, I., Bishop, J., Buccheri, A., Reid, J., Shee, A. W., Budge, M., Huggins, C. E., Peeters, A., & Metcalf, O. (2025). Challenges for remote patient monitoring programs in rural and regional areas: A qualitative study. BMC Health Services Research, 25(1), 374. https://doi.org/10.1186/s12913-025-12427-z
Tan, T. Q. (2019). Principles of Inclusion, Diversity, Access, and Equity. The Journal of Infectious Diseases, 220(Supplement_2), S30-S32. https://doi.org/10.1093/infdis/jiz198
Tiase, V. L., & Hobensack, M. (2023). Enabling techquity in nursing practice: Informatics, technology, and innovation. In S. Hassmiller, A. Darcy Mahoney, & K. Beard (Eds.), The future of nursing 2020–2030: Global applications to advance health equity (pp. 131–144). Springer. https://doi.org/10.1007/978-3-031-29746-5_10
Wan, S., Nappi, M., Chen, C., & Berretti, S. (2022). Guest editorial: Emerging IoT-driven smart health: From cloud to Edge. IEEE Journal of Biomedical and Health Informatics, 26(3), 937–938. https://doi.org/10.1109/JBHI.2022.3149040
Wickramasinghe, N., Jayaraman, P. P., Forkan, A. R. M., Ulapane, N., Kaul, R., Vaughan, S., & Zelcer, J. (2021). A vision for leveraging the concept of digital twins to support the provision of personalized cancer care. IEEE Internet Computing, 26(5), 17–24.
Woods, L., Janssen, A., Robertson, S., Morgan, C., Butler-Henderson, K., Burton-Jones, A., & Sullivan, C. (2023). The typing is on the wall: Australia’s healthcare future needs a digitally capable workforce. Australian Health Review, 47(5), 553–558. https://doi.org/10.1071/AH23142
Woods, L., Eden, R., Macklin, S., Krivit, J., Duncan, R., Murray, H., Donovan, R., & Sullivan, C. (2024). Strengthening rural healthcare outcomes through digital health: qualitative multi-site case study. BMC health services research, 24(1), 1096. https://doi.org/10.1186/s12913-024-11402-4
Woźniak, M., Płoska, A., Siekierzycka, A., Dobrucki, L. W., Kalinowski, L., & Dobrucki, I. T. (2022). Molecular imaging and nanotechnology: Emerging tools in diagnostics and therapy. International Journal of Molecular Sciences, 23(5), 2658. Zayas-Cabán, T., Haque, S. N., & Kemper, N. (2021). Identifying Opportunities for Workflow Automation in Health Care: Lessons Learned from Other Industries. Applied Clinical Informatics, 12(3), 686–697. https://doi.org/10.1055/s-0041-1731744
The application of information and communication technologies in the fields of health care and medicine.
Jandoo, T. (2020). WHO guidance for digital health: What it means for researchers. Digital Health, 6, 2055207619898984–2055207619898984. https://doi.org/10.1177/2055207619898984.
The process of guiding and influencing the development, implementation and strategic direction of digital health technologies and solutions in healthcare systems.
Laukka, E., Pölkki, T., & Kanste, O. (2022). Leadership in the context of digital health services: A concept analysis. Journal of Nursing Management, 30(7), 2763–2780. https://doi.org/10.1111/jonm.13763.
The process of converting analogue information into a digital format, enabling the content to be programmed, addressed, traced and communicated.
Fahndrich, J. (2023). A literature review on the impact of digitalisation on management control. Journal of Management Control, 34(1), 9–65. https://doi.org/10.1007/s00187-022-00349-4
An interdisciplinary field that focuses on the effective use of biomedical data, information and knowledge for scientific research, problem-solving and decision making with the goal to enhance human health.
Jen, M. Y., Mechanic, O. J., & Teoli, D. (2023). Informatics. In StatPearls. StatPearls Publishing.
Refers to the ability to effectively and critically navigate and create information using a range of digital skills.
Tinmaz, H., Lee, Y.-T., Fanea-Ivanovici, M., & Baber, H. (2022). A systematic review on digital literacy. Smart Learning Environments, 9(1), 21. https://doi.org/10.1186/s40561-022-00204-y.
The ethical obligation to protect private and sensitive information from unauthorised disclosure.
The integration of digital technology into all areas of a business, fundamentally changing how it operates and delivers value to customers.
Andriole, S. J. (2020). The hard truth about soft digital transformation. IT Professional, 22(5), 13–16. DOI: 10.1109/MITP.2020.2972169.
Involves digital ways of thinking and working, to drive innovation, efficiency, productivity and user experience.
Australian Digital Health Agency. (2024). Workforce Strategy 2021–2026. Australian Government. https://www.digitalhealth.gov.au/sites/default/files/documents/agency-workforce-strategy-2021-2026.pdf.

