1.2 Communication in the digital health context
Angela Brown; Joanne Harmon; and Ken Ho

The integration of digital communication into health care has revolutionised the way healthcare services are delivered, enhancing the accessibility, efficiency and quality of nursing and midwifery care. This chapter aims to contextualise digital communication within health care. We first provide a scope for communication in the digital health context with reference to national digital health strategies. We then provide an overview of digital communication tools used nationally and internationally. The challenges and opportunities brought by such tools are then discussed, particularly for vulnerable and marginalised groups in Australia. Throughout the chapter, you will be guided to relevant readings and websites, and we provide examples to help your understanding of concepts and apply digital communication in practice contexts. This chapter will be a foundation for later chapters to develop deeper knowledge in digital health.
Learning Outcomes
By the end of this chapter you will be able to:
- Describe how digital communication is used in health contexts and the national strategies guiding its development.
- Describe digital information and communication tools employed in the Australian health system.
- Identify challenges and opportunities for digital communication in healthcare contexts.
Framing Questions
- What is meant by ‘digital health’ and ‘digital communication’?
- What primary tools are involved in digital health nationally and internationally?
- Who are the stakeholders in digital communication in healthcare contexts in Australia?
- What are challenges and opportunities of digital communication in healthcare contexts?
- How can digital communication enhance accessibility and inclusivity and the health literacy of vulnerable or marginalised populations?
- How can digital communication support person-centred care in nursing and midwifery?
1. Introduction to digital health communication in national and international contexts
Digital health refers to ‘systems, tools and services based on information and communication technology that can be used to treat patients and collect and share a patient’s health information’ (Australian Institute of Health and Welfare, 2025). Digital health is a contemporary development, nationally and internationally. It shows great potential in helping to overcome traditional challenges in health care, such as inequitable accessibility, management of chronic illnesses, duplicated investigations and more. The World Health Organization (WHO, 2021) in its Global strategy on digital health 2020–2025 (PDF) has suggested that digital and information and communication technologies are essential for universal health coverage and better protection from health emergencies. Therefore, digital health is an enabling factor for people to enjoy better health and wellbeing. However, the use of digital and information and communication technologies to improve healthcare delivery and patient outcomes (generally known as digital transformation) can be challenging for institutions, healthcare professionals, healthcare providers and end users (e.g. patients and caregivers).
In the context of digital health, communication has two-way functionality involving data sharing between a sender and a receiver. It can be synchronous or asynchronous for the purpose of delivering or receiving health and medical care. While sharing and exchange of health data is essential for communication in the context of digital health, those health data are also personally identifiable and contain sensitive information. As such, a high safety and security standard is crucial, and this requires strategic commitment and investment. In Australia, the Australian Digital Health Agency is the lead organisation for guiding the operation and development of the national digital health infrastructure that underpins the delivery of digital health.
Video: National Digital Health Strategy 2023–2028
Source: National Digital Health Strategy 2023–2028 on YouTube.
1.1 National digital health strategy: outcomes, enablers and roadmap priorities
The video above, introduced the National Digital Health Strategy 2023–2028. In this section, you are going to develop a deeper understanding of the National Digital Health Strategy, in terms of its outcomes, enablers and roadmap priorities.
Activity
Refer to Table 1: Health system outcomes and digital health
Re: National Digital Health Strategy outcomes.
- Explore the four health system outcomes.
- Identify how and why these outcomes are relevant to communication in digital health care for nurses and midwives?
Table 1: Health system outcomes and digital health
| Health system outcome | Relevance to communication in digital health |
|---|---|
| Digitally enabled | Digital health tools help healthcare providers to work together, connect services, share information and make decisions. |
| Person-centred | More reliable and comprehensive health information lets clients interact with healthcare providers to develop personalised support for unique health needs. |
| Inclusive | Through information and communication tools (e.g. telehealth), individuals (e.g. people in rural areas) in unconventional health service settings have more access to health care. |
| Data-driven | Data sharing between individuals and healthcare providers facilitates more informed clinical decision-making based on an individual’s needs. |
Activity
To deliver the outcomes of the National Digital Health Strategy effectively and successfully, four change enablers have been identified. Explore these four change enablers.
Finally, Table 2 summarises the 12 priorities in the strategy delivery roadmap of the National Digital Health Strategy.
Table 2: Health system outcomes and priorities
| Digitally enabled | Person-centred | Inclusive | Data-driven |
|---|---|---|---|
| Connect care
Enable a digitally ready workforce Enhance and maintain modern and integrated digital solutions |
Support strong consumer digital health literacy
Increase availability of health information Enhance consent management and flexible health information exchange |
Improve and expand virtual care
Integrate personal devices Support equitable health access |
Use health information for research and public health purposes
Plan for emerging data sources and technology Monitor and evaluate outcomes and progress |
The National Digital Health Strategy has driven the development of digital communication initiatives in Australia. These initiatives are now increasingly used by people across the country.
Activity
Visit the Australian Digital Health Agency website digitalhealth.gov.au
- Which digital health initiatives have you used, as an Australian citizen or resident, or as an international student?
- How do these initiatives appropriately use digital technologies in health?
2. Digital communication tools in Australia
Digital communication tools are at the heart of Australia’s journey toward enhancing healthcare service and delivery. Ensuring communication systems are connected and can share information easily is key. In Australia this is supported by the:
- National Digital Health Strategy
- Digital Health Blueprint and Action Plan 2023–2033
- National Healthcare Interoperability Plan.
The National Digital Health Strategy has digitally enabled connection of care as a core priority. This means digital communication tools are required for virtual connection of care episodes. These tools can streamline workflows, promote timely decision-making and support person-centred care across the nursing and midwifery professions.
Australians increasingly expect, as a norm, the use of digital capabilities to support their health and wellbeing. Therefore, it is important that nurses and midwives are informed and understand the evolving expectations and needs related to digital health communication tools. Increasingly, communication can be improved by consumers and healthcare providers using digital devices such as smartphones, applications (apps) and websites, combined with the availability of near real-time data to support and enhance services.
In Australia there has been a shift from paper-based records to digital (electronic) medical records. More efficient communication and collaboration can occur between different health care providers when notes are located on a patient’s electronic medical record. For example, patient medications, investigation results and discharge summaries.
Activity
Before we look at the types of digital health tools in detail, jot down a list of where you think digital health communication tools could be used and what their implications are.
- Think about people seeking health care in regional places. What could digital communication mean for these communities?
- Think about your previous or future clinical placements. How could digital health communication improve the transfer of information for service delivery? What do you think the barriers might be?
Table 3 shows some digital communication initiatives and examples.
Table 3: Digital communication initiatives and examples
| Digital communication initiative | Examples of use |
|---|---|
| National secure messaging capability for the exchange of clinical documents | When a nurse caring for a patient in a rural hospital requires input from a metropolitan nurse, the patient’s clinical records can be accessed |
| Connection of residential aged care facilities to My Health Record | When a resident receives an intervention such as a vaccine, their health record is kept up to date |
| Electronic referrals, transfers of care and discharge summaries | For every episode of care, documentation provides for subsequent continuity of care that is culturally safe which is inclusive, providing convenience, often beyond traditional business hours |
| Electronic prescribing | No more use of paper prescriptions means valuable information is not lost. Prescriptions are legible |
| Newborn enrolment information | Registration of a child’s birth in their state or territory, with Medicare enrolment and birth verification to enable ease of access to other government payments and services |
| Advance care planning | Accurate and accessible documents to support, ongoing care and treatment preferences, and end-of-life decisions |
The next sections introduce a range of digital health communication tools and explores their application in real-world Australian healthcare contexts.
2.1 Mobile health
Mobile health (or mHealth) leverages mobile devices and applications (apps) to deliver health services and messages, facilitate patient engagement and improve health outcomes.
For example, parents can digitally manage their child’s health information through the My Child’s eHealth Record. This ensures continuity of care, as clinicians can access past care information, vaccination records, allergy information, medication records and pathology tests at the point of care.
Activity
Explore an mHealth app like Healthdirect or Pregnancy+.
- Evaluate its features. Consider how it supports midwifery or nursing care.
- Identify issues with the app.
- Identify potential improvements that could be made to protect people.
2.2 Digital medicines: electronic prescribing and medication charts
Electronic prescribing (ePrescribing) and medication charts can reduce errors and improve patient safety by providing accurate and up-to-date information. ePrescribing is the use of electronic rather than paper prescriptions. An ‘eScript’ can be sent to a person by SMS or email. The benefit of an eScript is that it comes with a QR code (also known as a digital token). The pharmacist then scans this so that they can access the prescription and give the person their medication. eScripts might also benefit those who are travelling or short on time, as the eScript can be forwarded to the pharmacist for pick up. Additionally, eScripts are less likely to be forged. The challenge with handwritten prescriptions is that they can contain errors, be inaccurate and have poor legibility, therefore, be more susceptible to fraud (Sendlhofer et al, 2019)
Activity
Read this paper by Sendlhofer et al (2019) on a new approach of assessing patient safety aspects in routine practice using the example of “doctors handwritten prescriptions”.
It is important to note that handwritten medication prescriptions may still be common in some hospitals, more so when situations arise when the internet is unavailable or on weekends.
Reflect on how incorrect, incomplete or illegible prescriptions risks patient safety and impacts workload for nurses and midwives as well as doctors due to the misinterpretation of handwriting.
Case study
Review the Australian Digital Health Agency website.
A patient in rural Victoria received a prescription electronically via the ePrescribing platform, avoiding the need to travel to a general practitioner (GP). Discuss how this aligns with the Australian Digital Health Agency’s goals.
2.3 Healthcare identifiers
The Healthcare Identifiers Service assigns unique identifiers to individuals, providers and organisations, facilitating seamless data exchange.
Websites
Read more about individual healthcare identifiers on the Services Australia website and about healthcare identifiers generally on the national Department of Health and Aged Care website.
Activity
How do healthcare identifiers support continuity of care in a midwifery caseload model or a GP medical clinic, particularly to ensure accurate data exchange, maintain patient privacy and enhance care coordination across multidisciplinary teams?
2.4 Electronic health records
The My Health Record system is a cornerstone of Australia’s National Digital Health Strategy, centralising health information for access by authorised healthcare providers.
Activity
See AuDigital Health on YouTube.
Access a video tutorial on the My Health Record system.
- Discuss with your student peers how electronic health records impact interdisciplinary collaboration in nursing or midwifery care.
- Consider the ethical implications of accessing sensitive patient information through electronic health records.
2.5 Telehealth
Telehealth refers to the provision of healthcare services, information and education using digital communication technology. This includes virtual consultations, remote monitoring and health education, allowing care to be delivered across geographical barriers. As a tool to enhance nursing care, telehealth supports telenursing, enabling patients to receive remote monitoring, telephone triage, health coaching and help with postoperative recovery or chronic health condition management. Likewise, telemidwifery integrates telehealth technologies into midwifery care. It enables midwives to remotely monitor pregnancies, offer antenatal education and provide postnatal support, such as breastfeeding guidance and postpartum recovery care. This approach is particularly beneficial for individuals in remote or underserved areas, ensuring that they receive consistent and quality maternity care.
Telehealth can provide vital healthcare services to remote and marginalised populations in Australia. What other populations could benefit from telehealth? Review the list below and see if you can think of any others.
- Rural and remote communities: provide access to specialists and healthcare services that may be unavailable locally.
- Elderly populations: reduces the need for travel and supports chronic disease management and routine care.
- People with disabilities: offers convenience and accessibility for individuals facing mobility or transportation challenges and those with high healthcare needs.
- Disadvantaged communities: bridge gaps in healthcare access for those in low-income or resource-poor settings.
- Chronic conditions: facilitates ongoing monitoring and management of conditions like diabetes, hypertension, arthritis and asthma.
- Mental health patients: provides accessible therapy and counselling, particularly in areas with limited mental health services.
- Parents and newborns: supports postnatal care and consultations for babies in remote locations.
- Aboriginal and Torres Strait Islander communities: enhances culturally appropriate healthcare access in remote areas.
- Immunocompromised people: reduces exposure risks by enabling remote consultations.
- Adolescents and young adults: offers accessible sexual and reproductive health services, including education and support.
Overall, telehealth ensures more equitable healthcare delivery by overcoming geographical, financial and physical barriers.
Activity
Midwifery students
A midwife in the Northern Territory conducts a telehealth consultation with a pregnant woman experiencing gestational diabetes.
Discuss the benefits and challenges of telehealth in rural maternity care.
Task
Simulate a teleconsultation session between the midwife and a pregnant woman. Have a third person take notes. Focus on communication and building rapport. Make sure each participant attempts each of the three roles.
Nursing students
A community nurse in a remote South Australian town conducts a telehealth consultation with a patient managing chronic heart failure who has difficulty attending in-person appointments.
Discuss the benefits and challenges of telehealth in rural nursing care, focusing on chronic disease management, patient education and access to care.
Task
Simulate a teleconsultation session between the community nurse and the remote patient. Have a third person take notes. Emphasise clear communication, patient education and assessing the patient’s understanding and engagement. Make sure each participant attempts each of the three roles.
2.6 Wearable devices
Wearable technologies like smartwatches and fitness trackers offer real-time health monitoring and empower patients to take charge of their health.
Reading
Read this paper by Canali et al. (2022): Challenges and recommendations for wearable devices in digital health: Data quality, interoperability, health equity, fairness
The four main functions of wearable devices are monitoring, screening, detection and prediction (Canali et al., 2022). Data from wearable devices can be used for continuous and remote monitoring, the aim being the connection with, for example, remote telehealth for individuals who may be at risk of deterioration and require hospitalisation. The role of a nurse or midwife would be accessing and interpreting crucial physiological data such as heart rate, oxygen saturation and so on. Digital technology enables efficient access to and communication of patient data and supports nurses and midwives’ workflow, routine tasks, and information management (Schlicht et al 2025).
During COVID-19 remote monitoring of mild cases allowed patients to report their vital signs from home to a nurse or other care provider via access to an app or telehealth, reducing the risk of transmission to healthcare providers and other patients by avoiding an in-person assessment (Seshadri et al., 2020).
Wearable devices can also be used for prediction, more so in relation to outbreaks, as uploading of data from those who are infected means primary healthcare nurses can be informed of hotspots and increase education on preventive measures.
What did you think of the paper? Can you think of any other benefits or challenges in the use of wearable devices for collecting health care data?
Activity
Continuous glucose monitoring (CGM) devices are invaluable for managing gestational diabetes or unstable diabetes for example Explore how wearable devices can support shared decision-making in antenatal care or diabetes care.
Critical thinking exercise
What ethical considerations arise with the use of wearables in vulnerable populations?
2.7 Electronic referrals
Electronic referral systems streamline communication between healthcare providers, reducing delays and improving care coordination. Once an electronic referral (eReferral) is made, it can be integrated into the electronic medical record system. This integration, for example, facilitates the automatic sharing of a patient’s referral documentation and information in preparation for an outpatient visit.
Website
Read about how NSW Health is using eReferrals at this NSW eHealth website: Engage outpatients
eReferrals save time, enable secure submission of patient information and improve communication between referrers, patients and outpatient clinics. Standardised forms help to ensure that accurate medical information, including test results, medical history and current medications, is captured correctly at the time of referral. The benefits electronic referrals have meant a move away from paper-based referrals, which are usually sent in the mail. Importantly, eReferrals can provide real-time notifications for patients and carers in languages other than English.
Activity
Midwifery activity
A GP refers a patient with a hypertensive disorder of pregnancy to a specialist via an eReferral system.
How do eReferrals improve communication across healthcare disciplines?
Nursing activity
A GP refers a patient with hypertension and renal failure to a specialist via an eReferral system.
How do eReferrals improve communication across healthcare disciplines?
2.8 Access to trusted data
Access to trusted, evidence-based data is essential for safe and effective nursing and midwifery practice. Sources like the Australian Institute of Health and Welfare (AIHW) and the Joanna Briggs Institute (JBI) offer reliable, evidence-based resources that support clinical decision-making and policy development.
Activity
Review the AIHW website for data related to chronic disease management in Australia: Australia’s health 2024: data insights: The ongoing challenge of chronic conditions in Australia
Identify one statistic and explain how it could influence nursing or midwifery practice or the development of a health promotion strategy.
For example: Find a statistic on the prevalence of diabetes in Australia. Discuss how this data could inform nursing interventions, such as targeted patient education, community programs for diabetes prevention or adjustments to hospital-based care pathways for diabetic patients.
Midwifery students
Search AIHW’s website for data on maternal health.
Identify one statistic and discuss how it could influence policy or practice in midwifery.
Key Takeaways
- Digital tools such as electronic health records, telehealth and AI enhance communication and care delivery in nursing and midwifery.
- Interactive technologies like wearables empower patients and improve outcomes.
- Ethical considerations, including privacy and equity of access, are integral to using digital tools responsibly.
3. Challenges and opportunities for digital communication in health care
Digital communication in health care has transformed the way information is shared, stored and accessed, enabling more streamlined and person-centred care. However, the rapid evolution of technology presents challenges and opportunities that must be addressed to maximise its potential while ensuring equitable and ethical practices.
3.1 Challenges

Equity of access
Digital communication relies heavily on technology, which is not equally accessible to all populations. Disparities in access to devices, reliable internet connections and digital skills can make existing health inequities worse, particularly for those in rural or remote areas, for individuals with low socioeconomic status and for older populations. Addressing these barriers is critical to ensuring that healthcare communication is inclusive and equitable for all.
Interoperability and data standards
Healthcare systems often use diverse technologies that lack interoperability, leading to challenges in sharing and accessing patient information across platforms. Without universal data standards, important details may be fragmented or lost, hindering continuity of care and potentially compromising patient safety.
Data literacy and data citizenship
Healthcare providers and people accessing health care need adequate data literacy to understand and effectively use digital health tools. Data citizenship – an individual’s ability to engage responsibly with digital data – becomes increasingly important in fostering trust and collaboration in the digital healthcare landscape. Lack of knowledge in this area can limit the effective adoption of technology.
Security and privacy
As health care becomes more digital, the risk of data breaches and cyberattacks grows. Patient data is highly sensitive, and any breach can have devastating consequences for individuals and institutions. Striking a balance between accessibility and robust security measures is essential for maintaining patient trust and compliance with legal and ethical standards.
Activity
You are a healthcare professional using a new telehealth platform. A patient expresses concern about how their data will be stored and who can access it.
- What steps would you take to reassure the patient about their data privacy?
- Identify one potential ethical dilemma that could arise with the telehealth platform.
- Suggest a best practice that healthcare organisations should follow to maintain data security and build patient trust.
Activity
Barriers and solutions
Review the following barriers and solutions table and match the correct barrier with the correct solution.
| Barrier | Solution |
|---|---|
| Lack of devices in low-income communities | Establish public wi-fi hotspots |
| Older adults struggling with digital tools | Partner with charities to donate refurbished devices |
| Limited internet access in rural areas | Offer free digital literacy workshops |
Choose one barrier and write a paragraph explaining how implementing the solution might improve healthcare outcomes.
3.2 Opportunities
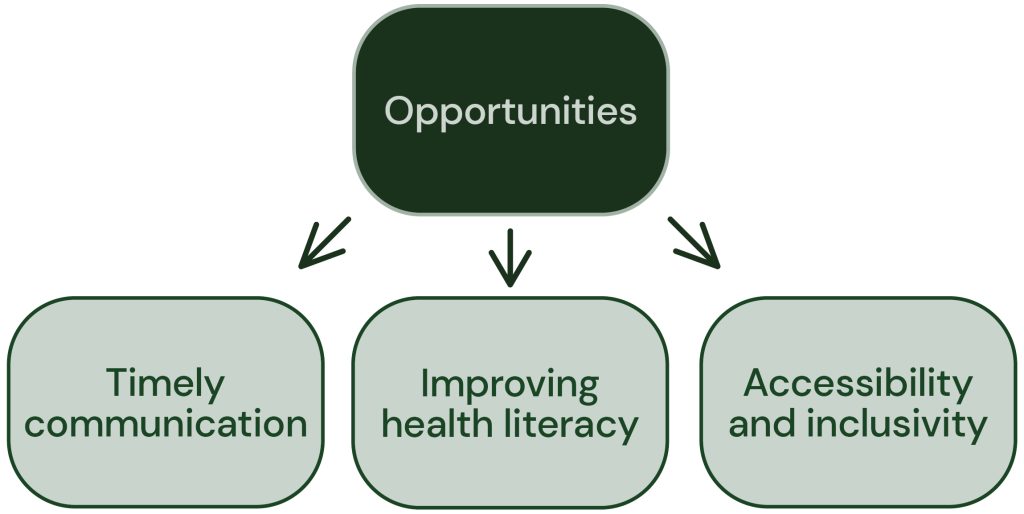
Timely communication
Digital platforms enable real-time communication between healthcare providers and the people they care for, facilitating faster decision-making and improving outcomes. Tools such as telehealth, patient portals and instant messaging allow for immediate access to care and support, even across large distances.
Improving health literacy
Digital communication opens up opportunities to improve health literacy by providing people with easy access to accurate, evidence-based information. Interactive tools, videos and infographics can enhance understanding, enabling individuals to make informed decisions about their health.
Accessibility and inclusivity
Well-designed digital tools can enhance accessibility for diverse populations, including those with disabilities or language barriers. Features such as screen readers, translation services and simplified interfaces make health care more inclusive, empowering people to engage more actively in their care.
Activity
Design challenge: accessibility and inclusion for digital tools
Imagine you are designing a patient portal that caters to diverse populations, including people with disabilities and those with limited English proficiency.
- Create a list of five accessibility features.
- Draw a simple interface mock-up or write a description of how these features would work.
- Write a short explanation of how each feature addresses the needs of specific populations, fostering inclusivity and active engagement in health care.
Activity
Infographic design: timely communication in action
Design an educational infographic or poster showcasing how tools like telehealth, patient portals and instant messaging:
- improve communication between providers and patients
- enable faster decision-making
- support patients in remote or rural areas.
Include real-world examples or hypothetical scenarios to illustrate your points.
Share your infographic with peers and gather feedback.
3.3 Making positive change in digital communication
Digital communication is reshaping the healthcare landscape, offering immense potential to improve accessibility, consumer engagement and outcomes. However, these opportunities can only be realised by addressing challenges such as inequities in access, technological fragmentation and the need for robust security and privacy measures. Recognising and tackling these issues ensures that digital communication serves as a tool for positive change, fostering a more equitable and efficient healthcare system.
Ethical and legal principles
Health professionals must maintain confidentiality, professionalism and legal compliance when using digital tools. Ethical communication requires safeguarding patient privacy, avoiding misinformation and adhering to privacy laws and professional codes of conduct.
Social media policies for health professionals
Social media offers opportunities for education and networking but must be used responsibly. The Australian Nursing and Midwifery Federation advises avoiding patient-identifiable information and maintaining professional boundaries (ANMF, 2022). The Australian Health Practitioner Regulation Agency emphasises confidentiality, accurate information and adherence to advertising rules to avoid disciplinary action (Ahpra, 2022). These will be explored further in the next chapter (1.3).
Key Takeaways
Health professionals should always:
- protect patient privacy
- reflect professionalism in all communications
- follow institutional and regulatory guidelines.
By following these principles, health professionals can engage responsibly in digital spaces.
4. Conclusion
This chapter has described digital health, digital communication and various digital tools used nationally and internationally. It introduced communication strategies used in the context of digital health and outlined how the WHO global strategy on digital health has served as a foundation for communication.
Importantly, this chapter introduced some of the key stakeholders in digital communications within an Australian healthcare context. It outlined digital information and communication tools used in the Australian healthcare system and introduced some of the evolving digital communication initiatives, with examples of use ranging from mobile health and applications to record keeping, wearable devices and electronic health records. This provides important foundational knowledge and gives those new to health an insight into the complexity of digital communication tools in use in an Australian healthcare context.
The chapter also introduced how nurses and midwives can use digital health communication tools to support person-centred care in the Australian healthcare system, along with challenges, opportunities and ethical considerations. This included examples of how digital communication can enhance accessibility and inclusivity and increase health literacy for vulnerable and marginalised populations. Ranging from the use of digital communication tools for those in rural or remote locations to those in marginalised populations, the chapter explored challenges for security and privacy, equity of access, data literacy and citizenship, and interoperability and standards. In addition, opportunities for timely communication, increased accessibility and inclusivity and improved health outcomes were also introduced. Many of these will be explored in more depth in later chapters.
Key Takeaways
- Health system outcomes for digital communication are based on digital enablement. The are also person centred, inclusive and data driven.
- The core priority of Australia’s National Digital Health Strategy is a focus on connection of care that is digitally enabled to provide person-centred care.
- Digital communication strategies and tools enhances accessibility and inclusivity.
- Digital health strategies can increase the health literacy of vulnerable or marginalised populations.
5. Further reading
Plans, strategies, and websites
Australian Digital Health Agency: National Digital Health Strategy
Australian Digital Health Agency: National Healthcare Interoperability Plan
Australian Government Department of Health and Aged Care: The Digital Health Blueprint and Action Plan 2023–2033
Australian Health Practitioner Regulation Agency. (2022). Social media guidance. https://www.ahpra.gov.au/Resources/Social-media-guidance.aspx
Australian Nursing and Midwifery Federation. (2022). Guidance note: Social media and online networking. https://anmf.org.au/media/ntfjgv00/anmf-guidance-note-social-media-and-online-networking.pdf
eHealth NSW: Engage outpatients – Outpatient referral management
Healthcare IT News: Inpatient care experience gets a boost from telenursing and AI A story about the provision of care with minimal disturbance to the patient.
Journal articles
Cresswell, N. R., Walker, S. T., Harrison, C., & Kent, F. (2024). Teaching digital interprofessional collaboration. The Clinical Teacher, 21(6), e13651. https://doi.org/10.1111/tct.13651
Hants, L., Bail, K., & Paterson, C. (2023). Clinical decision-making and the nursing process in digital health systems: An integrated systematic review. Journal of Clinical Nursing, 32(19–20), 7010–7035. https://doi.org/10.1111/jocn.16823
This paper identifies how nursing processes of assessment, planning, intervention and outcome evaluations have been incorporated into digital health systems.
6. References
Australian Health Practitioner Regulation Agency. (2022). Social media guidance. https://www.ahpra.gov.au/Resources/Social-media-guidance.aspx
Australian Nursing and Midwifery Federation. (2022). Guidance note: Social media and online networking. https://anmf.org.au/media/ntfjgv00/anmf-guidance-note-social-media-and-online-networking.pdf
Australian Institute of Health and Welfare. (2025). Digital health. https://www.aihw.gov.au/reports/australias-health/digital-health
Canali, S., Schiaffonati, V., & Aliverti, A. (2022). Challenges and recommendations for wearable devices in digital health: Data quality, interoperability, health equity, fairness. PLOS digital health, 1(10), e0000104. https://doi.org/10.1371/journal.pdig.0000104
NSW Department of Health. (2025). Engage outpatients – Outpatient referral management. NSW Government. https://www.ehealth.nsw.gov.au/solutions/patient-experience/electronic-referral/engage-outpatients
Paola, S. (2020). Pharmacies ‘often targeted on weekends and after hours’. AJP.com.au. https://ajp.com.au/news/pharmacies-often-targeted-on-weekends-and-after-hours/
Schlicht, L., Wendsche, J., Melzer, M., Tschetsche, L., & Rösler, U. (2025). Digital technologies in nursing: An umbrella review. International Journal of Nursing Studies, 161, 104950. https://doi.org/https://doi.org/10.1016/j.ijnurstu.2024.104950
Sendlhofer, G., Pregartner, G., Gombotz, V., Leitgeb, K., Tiefenbacher, P., Jantscher, L., Richter, C., Hoffmann, M., Kamolz, L. P., & Brunner, G. (2019). A new approach of assessing patient safety aspects in routine practice using the example of “doctors handwritten prescriptions”. Journal of Clinical Nursing, 28(7-8), 1242-1250. https://doi.org/https://doi.org/10.1111/jocn.14736
Seshadri, D. R., Davies, E. V., Harlow, E. R., Hsu, J. J., Knighton, S. C., Walker, T. A., Voos, J. E., & Drummond, C. K. (2020). Wearable sensors for COVID-19: A call to action to harness our digital infrastructure for remote patient monitoring and virtual assessments. Frontiers in Digital Health, 2, 8. https://doi.org/10.3389/fdgth.2020.00008
Shen, Y., Guo, D., Long, F., Mateos, L. A., Ding, H., Xiu, Z., Hellman, R. B., King, A., Chen, S., Zhang, C., & Tan, H. (2020). Robots under COVID-19 pandemic: A comprehensive survey. IEEE Access: Practical Innovations, Open Solutions, 9, 1590–1615. https://doi.org/10.1109/ACCESS.2020.3045792
World Health Organization. (2021). Global strategy on digital health 2020–2025. https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf
Wu, M., Du, X., Gu, R., & Wei, J. (2021). Artificial intelligence for clinical decision support in sepsis. Frontiers in Medicine, 8, 665464. https://doi.org/10.3389/fmed.2021.665464
Yadav, P., Chaudhari, K., Dave, A., & Sindhu, A. (2024). Exploring the evolution of robotic surgery in obstetrics and gynecology: Past, present, and future perspectives. Cureus, 16(3), e57155.
The application of information and communication technologies in the fields of health care and medicine.
Jandoo, T. (2020). WHO guidance for digital health: What it means for researchers. Digital Health, 6, 2055207619898984–2055207619898984. https://doi.org/10.1177/2055207619898984.
Founded in 1948, WHO is the United Nations agency that connects nations, partners and people to promote health, keep the world safe and serve the vulnerable.
The integration of digital technology into all areas of a business, fundamentally changing how it operates and delivers value to customers.
Andriole, S. J. (2020). The hard truth about soft digital transformation. IT Professional, 22(5), 13–16. DOI: 10.1109/MITP.2020.2972169.
Happening at the same time.
Happening at different times.
Standardised form to send a referral to an electronic medical record system; linked also to electronic medical records.
Refers to the ability to effectively and critically navigate and create information using a range of digital skills.
Tinmaz, H., Lee, Y.-T., Fanea-Ivanovici, M., & Baber, H. (2022). A systematic review on digital literacy. Smart Learning Environments, 9(1), 21. https://doi.org/10.1186/s40561-022-00204-y.
The ethical obligation to protect private and sensitive information from unauthorised disclosure.

